Abstract
Background Noncommunicable diseases (NCDs) account for an increasing proportion of global morbidity and mortality and unsparingly affecting war-torn populations. Diabetes and hypertension, in particular, were implicated in 80% of deaths in pre-conflict Syria (ca. 2010) [Sethi], and are as persistent as ever throughout the ongoing Syrian civil war. Over the past several years, evidence has been accruing to suggest that mobile health (“mHealth”) interventions are efficacious in improving health outcomes all over the world. Sana, an interdisciplinary organization comprising many healthcare-sector stakeholders, has devised a patient-controlled health records (PCHR) app that will allow physicians to monitor and impact their patients’ long-term health outcomes. Objective We intend to implement this technology solution in close collaboration with front-line healthcare workers, patients, local governments, and humanitarian organizations, so as to better understand the on-the-ground populations we are seeking to serve. Methods The first phase of product development and testing is slated to occur within 21 months of the project’s commencement. During months 0–6, the Sana.PCHR application will be iterated and optimized using available guidelines and inputs from country-based healthcare providers. At the same time, data on existing NCD treatment will be collected at local healthcare facilities for comparison purposes. During months 7–8, frontline healthcare workers will be trained to use the app, which will be subsequently deployed in selected health care facilities. Finally, during months 9–21, use of the application will be monitored and supported by MIT Sana and JHU, and modifications will be made as needed. Related data will be collected for research purposes. Results We anticipate that the Sana.PCHR app will improve health outcomes along four key axes: (1) the overall quality of NCD care by promoting adherence guidelines, both during patient-doctor interactions and throughout the patient’s longitudinal treatment; (2) care coverage by supporting lesser-trained providers in lower-resource settings during care delivery; (3) continuity of care by maintaining patient-specific information that can smooth transitions between healthcare providers; and (4) data analytics so that in the long term, humanitarian organizations can apply machine learning to improve operations and outcomes. Conclusion Sana.PCHR is an innovative approach to addressing the emerging global refugee crisis while simultaneously curbing the escalating burden of NCDs. Successfully implementing this application will lead to more granular and effective monitoring of refugees’ health, especially in resource-constrained settings.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Noncommunicable diseases (NCDs) represent one of the most formidable 21st Century public health challenges. As the worldwide infectious disease burden dwindles (thanks to modern medical advancements) and lifestyles adapt to globalization, NCDs will account for an increasingly large percentage of overall morbidity and mortality. NCDs (diabetes and hypertension in particular) were implicated in 80% of deaths in pre-conflict Syria (ca. 2010) [Sethi], and these problems persist even as the Syrian people face violence, displacement, and other consequences of war. Indeed, while the international media and medical communities remain keenly attuned to the conflict-related health concerns of Syria and other war-torn populations, little attention is paid to the relatively more “mundane” ravages of noncommunicable diseases.
Over the past several years, mobile health (“mHealth”) interventions have been touted as a possible means of delivering care to vulnerable and underserved populations, and there has been a great deal of evidence to support the efficacy of such tools in improving health outcomes along a variety of axes. An mHealth intervention in Somalia helped diagnose conditions that would have otherwise gone unnoticed in 25% of children participating in the study [Zachariah]. A digital nutritional questionnaire in Burma was similarly impactful [Selanikio]. Several studies conducted in among Palestinian refugees in Jordan used electronic medical records and cohort monitoring to improve diabetes and hypertension outcomes [Khader].
Sana is a cross-disciplinary organization, including clinicians and engineers as well as policy, public health, and business experts along the entire healthcare value chain. Hosted at the Laboratory for Computational Physiology at MIT’s Institute for Medical Engineering & Science, the Sana Project G Team—in conjunction with the International Rescue Committee and the Johns Hopkins Bloomberg School of Public Health—has devised a patient-controlled health records (PCHR) app that will allow physicians to monitor and impact their patients’ long-term health outcomes. Currently the only known mHealth tool for noncommunicable disease (NCD) management targeted towards gatekeepers in health care, the Sana.PCHR application has shown promise during its development in Lebanon. We intend to implement this technology solution in close collaboration with front-line healthcare workers, patients, local governments, and humanitarian organizations, so as to better understand the on-the-ground populations we are seeking to serve.
2 Methods
The Sana.PCHR app provides disease management guidelines as well as intuitive protocols for patient data storage. This application serves as a decision-making support tool for healthcare providers, thus promoting treatment adherence and ensuring a high quality of care. Patient-oriented outputs, such as printed reminders of a treatment regimen or daily text messages recommending behavioral changes, are also generated and delivered free of charge to patients. This is a particularly valuable component of NCD treatment, since many noncommunicable diseases depend heavily on lifestyles and personal habits. According to a recent article in the journal Science, “The United Nations Secretary-General’s report on prevention and control of NCDs is remarkably clear in recommending that ‘the greatest reductions in noncommunicable diseases will come from…population-wide interventions’ that address the risk factors of tobacco use, unhealthy diet, lack of physical activity, and harmful use of alcohol” [Chokshi]. The Sana.PCHR app also allows healthcare workers to avoid the hassle of maintaining paper records, which are unwieldy, error-prone, and susceptible to loss, damage, or disarray.
The Team: The Sana Research group is headquartered in the Laboratory for Computational Physiology at MIT’s Institute for Medical Engineering & Science. The Sana.PCHR team is comprised of students from the Harvard T. H. Chan School of Public Health and the Harvard-MIT Health Sciences and Technology Division. Other key partners include the Johns Hopkins Bloomberg School of Public Health and the International Rescue Committee (which provide support on the ground in our target locations), as well as students at the University of Waterloo (who are responsible for the technological implementation of the app).
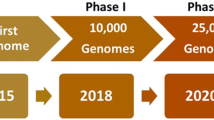
Development Timeline: The first phase of product development and testing is slated to occur within 21 months of the project’s commencement. Below is a more detailed breakdown of the individual tasks and their estimated durations.
-
Months 0–6: The Sana.PCHR application will be iterated and optimized using available guidelines and inputs from country-based healthcare providers. At the same time, data on existing noncommunicable disease treatment will be collected at local healthcare facilities for comparison purposes.
-
Months 7–8: Frontline healthcare workers will be trained to use the app, which will be subsequently deployed in selected health care facilities.
-
Months 9–21: Use of the application will be monitored and supported by MIT Sana and JHU, and modifications made as needed. Related data will be collected for research purposes.
Website: Our team has developed a website to showcase our ongoing progress on the Sana.PCHR application. Hosted on a Wix platform, the site is accessible via the following https://sanapchr2018.wixsite.com/projectg.
2.1 Product Specifications
The Project G Group was responsible for drafting the product specifications, which will ultimately be sent to our partner cohort of software developers at the University of Waterloo for implementation. For the purposes of this deliverable, we will adhere to the standard “product specs” format used widely throughout the software industry.
Problem: Succinctly stated, our team has been tasked with the responsibility of building a product that will store a patient’s clinical data from visit to visit, with new healthcare information added at each physician interaction. In software engineering terms, this boils down to maintaining a database of patients and their associated information for each user of the app (i.e. healthcare provider).
Features and Functional Requirements:
-
Maintains a database of care providers for each healthcare facility, each with his or her own login information (via secure authentication protocols)
-
Maintains a database of patients for each care provider
-
Fully operational offline
-
Syncs data to the cloud once a network connection is available
-
Interoperability with a backend web interface for data analytics.
Workflow:
See Fig. 27.1.
-
(1)
Log-in: The user can access his/her profile either with a username and password or through a QR code scan (see Fig. 27.2a). Possible actions:
-
Log in with password
-
Log in with QR code.
-
-
(2)
Welcome: Once logged in, the Sana.PCHR welcome screen will appear, prompting the user to either access an existing patient profile or generate a new one (see Fig. 27.2b). Possible actions:
-
Add new patient
-
Access existing patient data.
-
-
(3)
Add New Patient: The Add New Patient screen will prompt the care provider to upload details of the patient’s medical history (see Fig. 27.3a). Possible actions:
-
Input patient demographic data
-
Cancel entry and return to previous screen
-
Validate entry and proceed.
-
-
(4)
Enter Medical History: This portal will allow the physician to register the patient’s chief complaint, record previous diagnoses and medical problems, and flag any family histories of disease (see Fig. 27.3b). Possible actions:
-
Input medical history data
-
Cancel entry and return to previous screen
-
Validate entry and proceed.
-
-
(5)
Access Existing Patient Data: This portal will pull up the patient’s medical history, recorded during a previous session. Possible actions:
-
Return to previous screen
-
Proceed to the recording of clinical observations.
-
-
(6)
Record Clinical Observations: The physician can enter new physical measurements and clinical observations as well as record lab test results. Possible actions:
-
(7)
Adjust Treatment Plan: Here, the physician can make changes to existing treatment recommendations and medications (see Fig. 27.5a). She can upload a new prescription to the patient’s record, recommend lab tests following the consultation, add referrals to an external care provider, or recommend a return visit. Possible actions:
-
(8)
Finish and Print: Finally, the healthcare provider can confirm the visit details she has just input and print the resulting electronic medical record (presuming printing facilities are available). Possible actions:
-
Continue editing medical history, clinical observations, or recommendations
-
Finish and finalize the assessment
-
Print the medical record.
-
-
(9)
Send Ongoing Treatment Reminders: Throughout the patient’s treatment, he will receive free text-message alerts about any upcoming follow-up appointments, medication management, and behavioral “nudges” that will help mitigate or forestall the effects of NCDs. Thus, data within the patient’s record should trigger a scheduling protocol that sends automated messages at predetermined intervals.
At any point throughout this workflow, the patient has the capacity to log out or sync their data with the underlying cloud-hosted database, should an internet connection be available.
Use Cases: We can explore hypothetical use cases by considering each possible stakeholder/actor and imagining their interactions with the app.
Actor | Scenario | Requirements |
|---|---|---|
Individual care provider | A care provider wants to log into her account and access or amend existing patient data, so as to assess the patient’s disease progression | Each care provider has her own account with her own database of patients, whose data is stored securely and diachronically |
Patient | A patient visits a different clinic and wishes to bring his treatment records along | Patient records should be centralized so that they follow a given patient through the local healthcare system |
Local clinic | A clinic coordinator wants to track how many patients have been presenting with a particular set of complaints in the past year | Clinics should have access to high-level analytics about the patients that have visited their facility |
Government | A national public health official wishes to track any changes in NCD incidence after the implementation of a new policy | Government partners (if authorized) should have access to high-level, anonymized data about disease progression |
Humanitarian Organization | An international NGO wants to calculate the overall incidence of NCDs in a given locale, so as to allocate resources accordingly | Aid organizations should also have access to overall data trends |
System Requirements: We have selected Android as our app development platform, given the wide availability of Android-driven devices in the developing world.
Graphic Design: We generated mock-ups of our application, representing the various possible program states as seen in Figs. 27.2, 27.3, 27.4, 27.5 and 27.6. This design will be iterated in conjunction with our colleagues at the University of Waterloo.
3 Results
Proposed Impact: We anticipate that the Sana.PCHR app will improve health outcomes along four key axes. Our technology seeks to enhance:
-
(1)
The overall quality of noncommunicable disease care by promoting adherence guidelines, both during patient-doctor interactions and throughout the patient’s longitudinal treatment;
-
(2)
Care coverage by supporting lesser-trained providers in lower-resource settings during care delivery;
-
(3)
Continuity of care by maintaining patient-specific information that can smooth transitions between healthcare providers; and
-
(4)
Data analytics so that in the long term, humanitarian organizations can apply machine learning to improve operations and outcomes.
So far, testing has been conducted among roughly 800 Syrian refugees in primary care settings in Lebanon [Doocy].
Monitoring and evaluation of the application will be conducted throughout the development process. The Sana.PCHR tool will upload data to the cloud during use (presuming an active network connection), enabling us to collect crucial data for impact assessment. Qualitative data will be acquired through interviews, abiding by the guidelines of the Lean Research Framework (developed by the MIT D-Lab, the Feinstein International Center, and the Fletcher School of Law and Diplomacy) [Lean]. Country-specific outcomes will be evaluated according to the following metrics:
-
(1)
Number and type of providers using the application.
-
(2)
Provider retention rates.
-
(3)
Number of consultations per provider.
-
(4)
Completeness of records and management (in accordance with guidelines provided by partner humanitarian institutions).
-
(5)
Health outcomes (disease control, risk categories) if feasible.
-
(6)
Patient perceptions of application and benefits (if any).
Longer-term results will be evaluated as follows:
-
(1)
Number of organizations using the application.
-
(2)
Number of countries where the application is in use.
-
(3)
Number of NCD patients benefiting from the application.
-
(4)
Awareness of and feedback from the stakeholders (e.g. patients, care providers, last-mile health facilities, local NGOs, government partners, and international humanitarian organizations).
4 Discussion
Technology is not a panacea, and clever apps alone will not solve all the world’s global health challenges. Far too often, resources are indiscriminately thrown at problems without a holistic understanding of what really works in a given context. Furthermore, technology cannot simply be transferred wholesale from developed countries to resource-limited settings; solutions that work in one context usually need to be adapted to suit the needs of another locale.
This is especially important when considering the different contexts in which the Sana.PCHR app will be used. While community health workers in Syria have a long history of managing chronic NCDs such as diabetes and hypertension and may be able to refer their patients to primary and secondary centers without outside guidance, community health workers in conflict settings such as the Democratic Republic of Congo are not as familiar with these diseases, and may therefore use Sana.PCHR as a medium through which to track lifestyle and behavioral changes. It will be important to consider the nature and purpose of the application in different contexts as we proceed with the scale-up of Sana.PCHR.
Sana.PCHR provides an innovative tool with which community health workers and physicians can manage complex, chronic diseases in a transient and dynamic patient population. It is widely known that diseases such as hypertension and diabetes mellitus are difficult to manage even in stationary populations with established primary care physicians, and management of such diseases requires special considerations among refugee populations in conflict scenarios. With the development of Sana.PCHR, we hope to provide healthcare providers in different scenarios with a streamlined approach for accessing and modifying a patient’s medical records, in order to provide patients with the best possible care, even in non-traditional and transient settings.
References
Behar, J., Newton, A., Dafoulas, G., Celi, L.A., Chigurupati, R., Naik, S., & Paik, K. (2012). Sana: democratizing access to quality healthcare using an open mHealth architecture. International Journal of Integrated Care, 12.
Chokshi, D. A., & Farley, T. A. (2014). Changing behaviors to prevent noncommunicable diseases. Science, 345, 1243–1244. https://doi.org/10.1126/science.1259809.
Doocy, S. NCD guidelines and mHealth records for refugees in Lebanon. Research for Health in Humanitarian Crises (R2HC) Research Proposal Full Application. Johns Hopkins School of Public Health. App. No. 9880.
Khader, A., Farajallah, L., Shahin, Y., Hababeh, M., Abu-Zayed, I., Kochi, A., et al. (2012a). Cohort monitoring of persons with diabetes mellitus in a primary healthcare clinic for Palestine refugees in Jordan. Tropical Medicine & International Health, 17, 1569–1576. https://doi.org/10.1111/j.1365-3156.2012.03097.x.
Khader, A., Farajallah, L., Shahin, Y., Hababeh, M., Abu-Zayed, I., Kochi, A., et al. (2012b). Cohort monitoring of persons with hypertension: An illustrated example from a primary healthcare clinic for Palestine refugees in Jordan. Tropical Medicine & International Health, 17, 1163–1170. https://doi.org/10.1111/j.1365-3156.2012.03048.x.
Lean Research|D-Lab [www document], n.d. Retrieved November 5, 2018, from https://d-lab.mit.edu/lean-research.
Selanikio, J. D., Kemmer, T. M., Bovill, M., & Geisler, K. (2002). Mobile computing in the humanitarian assistance setting: An introduction and some first steps. Journal of Medical Systems, 26, 113–125.
Sethi, S., Jonsson, R., Skaff, R., & Tyler, F. (2017). Community-based noncommunicable disease care for Syrian refugees in Lebanon. Global Health: Science and Practice, 5, 495–506. https://doi.org/10.9745/GHSP-D-17-00043.
Zachariah, R., Bienvenue, B., Ayada, L., Manzi, M., Maalim, A., Engy, E., et al. (2012). Practicing medicine without borders: Tele-consultations and tele-mentoring for improving paediatric care in a conflict setting in Somalia? Tropical Medicine & International Health, 17, 1156–1162. https://doi.org/10.1111/j.1365-3156.2012.03047.x.
Author information
Authors and Affiliations
Corresponding authors
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2020 The Author(s)
About this chapter
Cite this chapter
McSharry, P. et al. (2020). Sana.PCHR: Patient-Controlled Electronic Health Records for Refugees. In: Celi, L., Majumder, M., Ordóñez, P., Osorio, J., Paik, K., Somai, M. (eds) Leveraging Data Science for Global Health. Springer, Cham. https://doi.org/10.1007/978-3-030-47994-7_27
Download citation
DOI: https://doi.org/10.1007/978-3-030-47994-7_27
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-47993-0
Online ISBN: 978-3-030-47994-7
eBook Packages: Computer ScienceComputer Science (R0)