Abstract
This chapter presents a state-of-the-art insight into the use of fractional laser for the management of this complex problem. In particular, we focus on the management of complex scars such as those occurring post-burn injury and split-thickness skin grafting.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Hypertrophic fractional laser and keloid scars present a spectrum of disorders that are difficult to treat. Multiple treatments have been tried, to ameliorate the clinical sequelae of scarring, such as erythema, pruritus, functional limitation, reduced range of movement, dyschromias, hyper and/or hypopigmentation. Early international clinical recommendations on scar management first recognized the importance of laser therapy in this armamentarium [1]. Within the years that followed, laser technology and the understanding of how it modulates the underlying processes that leads to hypertrophic and keloid scarring have experienced a quantum leap [2] and are still evolving. Lasers also present a considerable financial commitent, and it is possible, in the authors’ experience, that limited early results partially stemmed from limited availability of multiple lasers with consequent attempts to overstretch the indications for what was available.
This chapter presents a state-of-the-art insight into the use of fractional laser for the management of this complex problem. In particular, we focus on the management of complex scars such as those occurring post-burn injury and split-thickness skin grafting.
2 Method of Action
Light energy can be used to modulate or ablate specific targets in the skin through selective absorption of energy and specific heat energy dissipation properties [3]. The theory of selective photothermolysis, first described in 1983, laid the foundations for subsequent developments and standard practices [3]. When used to induce a controlled thermal injury, lasers initiate information processes to increase vascular permeability and modulate matrix metalloproteinase production of collagen fiber deposition and tissue hypoxia caused by targeted vascular ablation [4]. Through these processes, wound healing specifically in the remodeling phase may be manipulated, resulting in scar maturation and obviation of symptoms [5]. Different types of lasers are useful in targeting the different components of this disease scar tissue and it is important that the laser practitioner has the essential range of appropriately powered tools required to produce an optimal effect.
The choice of fractional laser in the management of a hypertrophic spectrum scar depends upon whether an ablative or non-ablative effect is desired, the target chromophore, the background skin type, the thickness of scarring, requirement for laser-assisted drug delivery (LADD), and the patient’s compliance with postoperative downtime and regimes. The Azzopardi classification of chromophores also helps the practitioner rationalize the likely target and downstream metabolic effects [6]. Fractionated lasers with established effectiveness include CO2 and Er YAG (nanosecond modality). More recently, fractioned, picosecond Nd: YAG has emerged as a potent platform in this context.
3 Fractioned Laser Platforms
Fraction laser resurfacing creates microscopic columns of ablation in epidermis and dermis, termed microscopic treatment zones. The relationship of these zones to intervening blocks of normal tissue permit rapid heat dissipation yet deliver enough energy to allow immediate changes in scar pliability, and instigate scar remodeling and neocollagenesis. The use of non-fractioned platforms such as pulsed dye and KTP (532 nm) are well documented and discussed elsewhere.
Fractioned CO2 (10,600 nm) and Er:YAG (2940 nm) are the two main ablative modalities in use, targeting water and collagen to produce mass transfer zones (MTZs) of defined diameter (70–100 μm) and depth, tissue vaporization, and coagulation.
At the molecular level, fractional ablative laser treatment induces upregulation of heat shock protein, upregulation of matrix metalloproteinase, fibroblast apoptosis, downregulation of transforming growth factors and basic fibroblast growth factors, and modulation of collagen-type ratios. These changes are evident beyond the microscopic treatment zones, yet the spared tissues contribute to rapid, normalized wound healing. A major difference however between CO2 and Er:YAG laser is the potential to achieve immediate coagulation and hemostasis: CO2 laser is 10 times more effective in this regard. This is critically important when considering resurfacing of extensive areas and when considering LADD, as in our experience, bleeding results in plugging and reduced LADD efficacy. Moreover, the waveform characteristics of a CO2 laser have a significant bearing on the potential for side effects.
4 Fractioned CO2 Laser
Indications and timing: The latest version of consensus international guidelines for prevention and treatment of pathological scarring (2014) reserve the use of fractional laser therapy for scars refractory to pulsed dye laser; widespread hypertrophic burn scars that failed to improve with treatment with silicone gel or sheeting, pressure garments, and/or onion extract preparations for 8–12 weeks; minor keloids that failed to improve within 8–12 weeks with silicone gel sheeting and intralesional corticosteroids; and major keloids resistant to improvement with intralesional corticosteroids and 5-FU may be treated with ablative fractional laser or PDL therapy. This philosophy has been challenged by recent literature.
First, the use of fractioned CO2 has since been successfully used (to date, off-license) with extensive and well-documented success, as an adjunct facilitating transdermal delivery (see below) [7]. Pulsed dye is less effective in scars more than 1.2 mm depth, and do not allow for effective scar pliability that may substantially facilitate post-procedure physical therapy. From a basic sciences perspective, once it has been established that fractioned ablative laser may re-instigate appropriate scar remodeling, it would be more useful to target the scar during the remodeling phase once epidermal integrity is well established. Recent literature supports earlier intervention than the previous 6 months to a year postinjury dogma, in concordance with our experience. In our experience, a treatment interval of 4–6 weeks is acceptable. Further, given the tendency of corticosteroid to exacerbate telangiectasias, use of fractioned CO2 first (±LADD) followed by vascular-type laser to correct any resulting telangiectasia may also be an acceptable and more time-efficient approach.
5 Settings for Ablative Fractional CO2 Laser
Utmost caution is advised when deciding clinical settings as these will vary between platforms. Many superpulsed lasers can only produce a shark tooth–type waveform. This results in the need to impart substantially more energy for the therapeutic threshold to be achieved. This additional energy may be responsible for the increased risk of complications seen in the literature (both medical and legal) with these laser platforms. In contrast, lasers imparting a “top hat pattern” waveform impart only enough energy for the therapeutic threshold to be achieved. Further safety considerations include maintaining an inverse ratio of power to density, and ideally to avoid imparting a fluence that is above TRT, density sets the number of MTZs per unit area, which should not be above 10%. Ideally, for purposes of safety, pre- and post-cooling regime should also be considered. A cold-air blower provides excellent pre-and post-cooling as well as being an effective analgesic.
Further settings include the size, shape, pulse stacking, and depth. Shape and size of the fractioned beam can be changed according to prevailing need. Whether the beam should penetrate beyond the scar thickness is still being investigated; however, injuries beyond the dermis may well lead to scarring and should be avoided [8].
6 Fractioned Erbium:YAG
The clinical efficacy of Er:YAG in keloid scars is limited. Cavale et al. combined Er:YAG with twice daily topical betamethasone under occlusion until therapeutic maximum was achieved, resulting in 50% improvement (median, n = 70), but recurrences also occurred in 22% of lesions [9]. One factor which may explain this disappointing result is the limited ability of current Er:YAG technology to penetrated deeply, and lower hemostasis.
7 Fractional Non-ablative Laser
Fractional 1550 nm Erbium-doped fiber laser reported overall improvement in scar texture after four treatments spaced 2 weeks apart, compared to the non-treated part of this split-scar study [10]. Literature reports that the response is mediated by heat shock protein, fibroblast proliferation, and consequent neocollagenesis [10].
A recent comparative RCT reports 1550 nm Er-doped fiber (70 mJ/23% coverage) to be superior to pulsed dye laser (7.5 mJ/10 mm/0.45 ms), with a 75% compared to 53% improvement reported [11, 12].
8 Picosecond, Fractioned, 1064 nm Nd:YAG
Management of hypertrophic and keloid scarring in darker skin types is a formidable challenge. Longer wavelengths, cooling devices, and lower treatment fluences have been shown to minimize complications [13, 14]. Recently, fractional picosecond 1064 lasers have reported good outcomes with very few side effects [15]. Compared to the conventional nanosecond domain QS Nd:YAG laser, the ps-Nd:YAG can produce significantly higher peak powers at the same energy level [16]. It is therefore expected that such technology works principally through photomechanical rather than photothermal effects [17]. The inhibitory effect of the 1064-nm Nd:YAG laser against dermal collagen formation is documented in the literature [18,19,20]. More recently, the use of fractioned 755 nm picosecond laser has been reported to be effective and safe in patients with Fitzpatrick skin types 4–6 [20].
9 Cautions and Contraindications
Caution is advised with any underlying process that impedes wound healing. History of herpes simplex virus, especially if lasering is to be attempted in the peroral area, should prompt prophylactic management. Oral antivirals or more recently bromelain should be considered [12, 21, 22]. Current depth of penetration for ablative fractional devices is approximately 4 mm, and therefore management of deeper scars is less likely to be as effective [22].
10 Preoperative and Postoperative Regimes
No consensus exists with regard to preoperative preparation. Some prepare skin with chlorhexidine solution and moistening hair-bearing areas prior to treatment [23]. Others, including the authors, are content with cleansed, dry skin [24]. It is important to note that whatever preparation method is favored, that moist and humid surfaces result in reduced ablation, and increased heat latency since the primary target, water, is now in increased abundance.
Several factors influence the choice of anesthesia, depending on the age of the patients, available equipment, and extent of surface area treated. However, overarching principles governing the practice of both authors include the use of the safest, least-invasive modality first, pre-optimization, and dual effect of skin cooling in increasing safety as well as providing an analgesic effect. Within this context, pretreatment with topical anesthetics of increasing strength coupled with cold-air blowers may provide the mainstay of analgesia requirements [25].
Where general anesthesia is required, it is possible to apply topical anesthesia immediately after fractioned CO2 lasering. However, the facilitation of transdermal delivery will facilitate increased absorption (see below), and therefore it important to consider the maximum safe dose to avoid anesthesia-related toxicity. Use of ice-water packs immediately following treatment provides additional modalities for heat dissipation and analgesia [26].
Again, postoperative regimes vary widely, depending on resource, patient compliance, and experience. Use of antiseptic moisturizers, followed by a regime of moisturization is strongly advised, along with hydrocortisone for pruritus. Sun protection is mandatory. Patients may resume normal activity almost immediately, including physical or occupational therapy. Showering is permitted, with the exception of full immersion in standing (bath) water where ablative laser has been used. Some degree of edema is expected. Depending on the patient’s tolerance, compressive garments may be worn immediately after, but they may cause shear of treated tissue, and therefore it is sensible to recommend waiting for 24–48 h before use.
11 Expected Outcomes
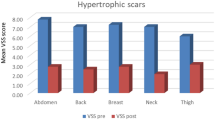
Benefits associated with CO2 laser treatment include increased scar pliability and reduced tightness, but it is important to impress on the patient that laser treatment creates the potential for increased scar pliability which is accomplished only by compliance with aggressive physical therapy postoperatively. Appropriate patient selection is therefore paramount, as is the availability of experienced and motivating physical therapists. Further benefits include reduced scar height and thickness. Pruritus has been observed to decrease in several studies presumably because nerve endings are no longer encased in tight scar tissues.
Similarly, fractioned CO2 laser may directly address the source of keloid formation, when this occurs in hair-bearing skin. Here, the hair follicle is encapsulated in the scar, which subsequently inflames, infects, and results in perpetuation of the insult-driving keloid growth. Scar remodeling results in amelioration of pliability, and in the authors’ experience it is not uncommon to result in resolution of the insult-driving keloidal growth as well as regrowth of hair in the site.
By inversely relating density to energy settings, it is also possible to attenuate relative scar height, resulting in flattening.
12 Potential Complications
The principal complications reported in the literature include burns, infection (viral, bacterial, mycotic) postoperative pain, and abnormal pigmentation: Post-inflammatory hyperpigmentation as well as hypopigmentation have been reported. In those being treated for burn injury memory flashbacks to the original incident have been reported in the literature, therefore it is essential that patients are forewarned. It is of course important to discuss the potential of multiple treatments. A large prospective study performed by Hultmann and colleagues puts the overall complication rate at 3.9% of all treatments: in decreasing order of incidence, hypopigmentation, blistering, hyperpigmentation, infection, cellulitis of the adjacent skin, superficial mycoses, and oral herpes simplex [27].
Practical recommendations for improving patient safety are judicious use of fluence (especially in darker skin types), use of pre- and post-cooling regimes, single pass, and avoiding stacking pulses, intentionally or otherwise [8]. Multimodality treatment to one area within the same sitting is indeed possible, given the mastery of the underlying principles, correct understanding of the disease extent, the background skin type, and the patient’s potential for healing. However, it significantly increases the risk for adverse events and therefore best avoided, except where mandated by individual risk–benefit considerations and availability of experts with appropriate experience. The use of test-patching and initiation of treatment in non-cosmetically conspicuous areas are advocated. In addition, a readily available database of previous patient-specific settings allows setting optimization to be delivered based on previous successes or complications.
13 Fractioned CO2 Laser as a Method for Potentiating Transdermal Laser-Assisted Drug Delivery (LADD)
Ablative fractional laser breaches epidermal integrity, producing newly formed, uniform, and deep channels into hard dermal scars. It is well established (but at time of publishing as yet off license) to harness this phenomenon as an effective method for trans-dermal drug delivery (◘ Fig. 33.1). The two-fold advantages may be summarized as follows: less pain and more even distribution. First, traditional injection of volume into tight dermal scarring produces uneven distribution, creating blebs of volume while no treatment to adjacent areas. Volume injection into a tight scar also increases pain and discomfort [28]. Recent literature also points to various aspect of improvement this technique addresses, including pain tolerance, texture, dyschromia, and hypertrophy [26, 28, 29].
In Laser Assisted Drug Delivery, is a recent advancement where laser energy is used to enhance trans-dermal drug delivery. For scarring a, typically, a fractioned ablative laser beam is used to create channels within the scar b. This is followed expeditiously with topical application c. The topical application is massaged in to the lasered area to enhance absorbtion d
Pain relief: Intra-scar injection is often poorly tolerated pain-wise, especially when larger surface areas are being considered. Several studies have established that fractional Er:YAG pretreatment reduces up to twelvefold the time required for topical anesthesia to take effect. However, within these studies, it is impossible to assess whether mild adverse events reported (including residual pain, redness, or mild-moderate swelling) was due to the needle or laser, as the effect was measured only after the needle was inserted. Typical settings for this indication are fluence of 250 mJ/pulse, a pulse width of 300 microseconds, and an estimated pore depth of less than 20 mm [30,31,32].
More importantly, this data demonstrates that application of local anesthesia post-procedure is likely to be more efficiently absorbed. While care needs to be taken with maximum dose due to altered absorption, post-procedure topical anesthesia may provide valuable pain relief, and is the standard practice of one of the authors (EA) when treating larger areas of sheet hypertrophic scarring post burns, with no side effects noted to date.
LADD has been used to potentiate transdermal delivery of both corticosteroid [33,34,35,36,37] as well as 5-fluorouracil [38] as well as combination treatment [38]. More recent evidence suggests that both are equally effective, but 5-FU does not lead to dermal atrophy or telangiectasia seen with corticosteroid delivery [39].
14 Consensus Practice
Established clinical consensus is that ablative lasers are significantly more effective per treatment for scar improvement than their non-ablative counterparts, especially for keloid and hypertrophic contracted scars, with significant gain in pruritus, pain, and physical mobility within days and up to 2 weeks posttreatment. Usually, rapid improvement in dyspigmentation is followed by slower improvement in texture and range of movement [22].
Take-Home Messages
-
Hypertrophic and keloid scars present a spectrum of difficult to treat disorders, and different types of lasers are useful in targeting the different components of this disease scar tissue.
-
The choice of fractional laser in the management of a hypertrophic spectrum scar depends upon whether an ablative or non-ablative effect is desired, the target chromophore, the background skin type, the thickness of scarring, requirement for laser-assisted drug delivery (LADD), and the patient’s compliance with postoperative downtime and regimes.
-
Fraction laser resurfacing creates microscopic columns of ablation in epidermis and dermis, termed microscopic treatment zones.
-
The relationship of these zones to intervening blocks of normal tissue permit rapid heat dissipation yet deliver enough energy to allow immediate changes in scar pliability and instigate scar remodelling and neo-collagenesis.
-
Fractional ablative laser treatment induces remodelling changes that are evident beyond the microscopic treatment zones, yet the spared tissues contribute to rapid, normalized wound healing.
-
The main modalities in use are CO2 and Er:YAG laser. CO2 has the potential to achieve 10-fold more immediate coagulation and hemostasis. This is critically important when considering resurfacing of extensive areas and for LADD.
-
Picosecond systems act principally through photomechanical rather than photothermal effects and may be useful in darker skin types.
-
Ablative fractional laser breaches epidermal integrity, producing newly formed, uniform, and deep channels into hard dermal scars. It is well established (but at time of publishing as yet off license) to harness this phenomenon as an effective method for trans-dermal drug delivery.
-
There is no universally accepted skin prep regime, however moist surfaces result in reduced ablation, and increased heat latency.
References
Mustoe, Thomas A., et al. “International clinical recommendations on scar management.” Plastic and reconstructive surgery 110.2 (2002):560–71.
Gold MH, et al. Updated international clinical recommendations on scar management: part 2—algorithms for scar prevention and treatment. Dermatol Surg. 2014;40:825–31. https://doi.org/10.1111/dsu.0000000000000050.
Manstein D, Herron GS, Sink RK, Tanner H, Anderson RR. Fractional photothermolysis: a new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med. 2004;34:426–38.
Jih MH, Kimyai-Asadi A. Seminars in cutaneous medicine and surgery. Philadelphia: WB Saunders. 2008. p. 63–71.
Laubach HJ, Tannous Z, Anderson RR, Manstein D. Skin responses to fractional photothermolysis. Lasers Surg Med. 2006;38:142–9.
Azzopardi EA, et al. Chromophores in operative surgery: current practice and rationalized development. J Control Release. 2017;249:123–30.
Zaleski-Larsen LA, Fabi SG. Laser-assisted drug delivery. Dermatol Surg. 2016;42:919–31.
Tredget EE, Levi B, Donelan MB. Biology and principles of scar management and burn reconstruction. Surg Clin. 2014;94:793–815.
Cavalié M, et al. Treatment of keloids with laser-assisted topical steroid delivery: a retrospective study of 23 cases. Dermatol Ther. 2015;28:74–8.
Hantash BM, et al. In vivo histological evaluation of a novel ablative fractional resurfacing device. Lasers Surg Med. 2007;39:96–107.
Tierney E, Mahmoud BH, Srivastava D, Ozog D, Kouba DJ. Treatment of surgical scars with nonablative fractional laser versus pulsed dye laser: a randomized controlled trial. Dermatol Surg. 2009;35:1172–80.
Graber EM, Tanzi EL, Alster TS. Side effects and complications of fractional laser photothermolysis: experience with 961 treatments. Dermatol Surg. 2008;34:301–7.
Alexis A. Lasers and light-based therapies in ethnic skin: treatment options and recommendations for Fitzpatrick skin types V and VI. Br J Dermatol. 2013;169:91–7.
Ross EV, et al. Treatment of pseudofolliculitis barbae in skin types IV, V, and VI with a long-pulsed neodymium: yttrium aluminum garnet laser. J Am Acad Dermatol. 2002;47:263–70.
Cho S, et al. Efficacy and safety of 1064-nm Q-switched Nd: YAG laser with low fluence for keloids and hypertrophic scars. J Eur Acad Dermatol Venereol. 2010;24:1070–4.
Abergel RP, et al. Control of connective tissue metabolism by lasers: recent developments and future prospects. J Am Acad Dermatol. 1984;11:1142–50.
Koike S, et al. Nd: YAG laser treatment for keloids and hypertrophic scars: an analysis of 102 cases. Plast Reconstr Surg Glob Open. 2014;2(12):e272.
Dang Y, Ye X, Weng Y, Tong Z, Ren Q. Effects of the 532-nm and 1,064-nm Q-switched Nd: YAG lasers on collagen turnover of cultured human skin fibroblasts: a comparative study. Lasers Med Sci. 2010;25:719–26.
Abergel RP, Meeker CA, Dwyer RM, Lesavoy MA, Uitto J. Nonthermal effects of Nd: YAG laser on biological functions of human skin fibroblasts in culture. Lasers Surg Med. 1984;3:279–84.
Haimovic A, Brauer JA, Bae Y-SC, Geronemus RG. Safety of a picosecond laser with diffractive lens array (DLA) in the treatment of Fitzpatrick skin types IV to VI: a retrospective review. J Am Acad Dermatol. 2016;74:931–6.
Hassouneh B, Newman JP. Lasers, fillers, and neurotoxins: avoiding complications in the cosmetic facial practice. Facial Plast Surg Clin. 2013;21:585–98.
Anderson RR, et al. Laser treatment of traumatic scars with an emphasis on ablative fractional laser resurfacing: consensus report. JAMA Dermatol. 2014;150:187–93.
Khandelwal A, Yelvington M, Tang X, Brown S. Ablative fractional photothermolysis for the treatment of hypertrophic burn scars in adult and pediatric patients: a single surgeon’s experience. J Burn Care Res. 2014;35:455–63.
McGoldrick RB, Theodorakopoulou E, Azzopardi EA, Murison M. Lasers and ancillary treatments for scar management part 2: keloid, hypertrophic, pigmented and acne scars. Scars Burns Heal. 2017;3:2059513116689805.
Edkins RE, et al. Improving comfort and throughput for patients undergoing fractionated laser ablation of symptomatic burn scars. Ann Plast Surg. 2015;74:293–9.
Hædersdal M, et al. Fractional CO2 laser-assisted drug delivery. Lasers Surg Med. 2010;42:113–22.
Hultman CS, Friedstat JS, Edkins RE, Cairns BA, Meyer AA. Laser resurfacing and remodeling of hypertrophic burn scars: the results of a large, prospective, before-after cohort study, with long-term follow-up. Ann Surg. 2014;260:519–32.
Waibel JS, Wulkan AJ, Shumaker PR. Treatment of hypertrophic scars using laser and laser assisted corticosteroid delivery. Lasers Surg Med. 2013;45:135–40. https://doi.org/10.1002/lsm.22120.
Lee W-R, et al. Laser-assisted topical drug delivery by using a low-fluence fractional laser: imiquimod and macromolecules. J Control Release. 2011;153:240–8.
Baron ED, et al. Laser-assisted penetration of topical anesthetic in adults. Arch Dermatol. 2003;139:1288–90.
Bachhav Y, et al. Effect of controlled laser microporation on drug transport kinetics into and across the skin. J Control Release. 2010;146:31–6.
Shapiro H, Harris L, Hetzel FW, Bar-Or D. Laser assisted delivery of topical anesthesia for intramuscular needle insertion in adults. Lasers Surg Med. 2002;31:252–6.
Majid I, Imran S. Fractional carbon dioxide laser resurfacing in combination with potent topical corticosteroids for hypertrophic burn scars in the pediatric age group: an open label study. Dermatol Surg. 2018;44:1102–8. https://doi.org/10.1097/dss.0000000000001413.
Park JH, Chun JY, Lee JH. Laser-assisted topical corticosteroid delivery for the treatment of keloids. Lasers Med Sci. 2017;32:601–8. https://doi.org/10.1007/s10103-017-2154-5.
Sobhi RM, et al. Comparative study of fractional CO2 laser and fractional CO2 laser-assisted drug delivery of topical steroid and topical vitamin C in macular amyloidosis. Lasers Med Sci. 2018;33:909–16. https://doi.org/10.1007/s10103-018-2457-1.
Tu JH, Udkoff JA, Eichenfield LF. Treatment of pediatric treadmill burn contractures with ablative fractional laser and topical triamcinolone suspension. Dermatol Surg. 2018;44:1656–9. https://doi.org/10.1097/dss.0000000000001553.
Willows BM, Ilyas M, Sharma A. Laser in the management of burn scars. Burns: J Int Soc Burn Inj. 2017;43:1379–89. https://doi.org/10.1016/j.burns.2017.07.001.
Lee BW, et al. Ablative fractional laser resurfacing with laser-assisted delivery of 5-fluorouracil for the treatment of cicatricial ectropion and periocular scarring. Ophthal Plast Reconstr Surg. 2018;34:274–9. https://doi.org/10.1097/iop.0000000000000948.
Waibel JS, Wulkan AJ, Rudnick A, Daoud A. Treatment of hypertrophic scars using laser-assisted corticosteroid versus laser-assisted 5-fluorouracil delivery. Dermatol Surg. 2019;45:423–30. https://doi.org/10.1097/dss.0000000000001678.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2020 The Author(s)
About this chapter
Cite this chapter
Tretti Clementoni, M., Azzopardi, E. (2020). Minimally Invasive Technologies for Treatment of HTS and Keloids: Fractional Laser. In: Téot, L., Mustoe, T.A., Middelkoop, E., Gauglitz, G.G. (eds) Textbook on Scar Management. Springer, Cham. https://doi.org/10.1007/978-3-030-44766-3_33
Download citation
DOI: https://doi.org/10.1007/978-3-030-44766-3_33
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-44765-6
Online ISBN: 978-3-030-44766-3
eBook Packages: MedicineMedicine (R0)