Abstract
There are many therapeutic options for keloids and hypertrophic scars, including surgery, radiation, corticosteroids, 5-fluorouracil, cryotherapy, laser therapy, anti-allergy agents, anti-inflammatory agents, bleaching creams, and make-up therapies. In terms of laser therapy, we have used long-pulsed 1064 nm Nd:YAG laser to treat keloids and hypertrophic scars. This laser was developed for the treatment of vascular diseases, including inflammatory scars that exhibit neovascularization. The depth that is reached is determined by the spot size, the laser power, and the fluence: the larger the spot size, power, or fluence, the deeper the laser beam penetrates. The laser should generally be applied to the skin surface with the following standard treatment settings: a spot diameter of 5 mm, an energy density of 75 J/cm2, an exposure time per pulse of 25 ms, and a repetition rate of 2 Hz.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Take-Home Messages-
It has been used long-pulsed 1064 nm Nd:YAG laser to treat keloids and hypertrophic scars.
-
Long-pulsed 1064 nm Nd:YAG laser was developed for the treatment of vascular diseases, including inflammatory scars that exhibit neovascularization.
-
The depth that is reached is determined by the spot size, the laser power, and the fluence: the larger the spot size, power, or fluence, the deeper the laser beam penetrates.
-
The standard treatment setting is a spot diameter of 5 mm, an energy density of 75 J/cm2, an exposure time per pulse of 25 ms, and a repetition rate of 2 Hz.
1 Background
Keloids and hypertrophic scars are fibroproliferative disorders of the skin that are caused by abnormal healing of injured or irritated skin [1]. Both disorders have similar histological features: the epidermis and the papillary layer of the dermis are almost normal apart from slight inflammation, and the only abnormality is in the reticular layer of the dermis [2]. While keloids typically exhibit marked hyalinized collagen deposition as a result of prolonged and strong inflammation, this feature is less pronounced in hypertrophic scars [3]. Thus, it is possible that hypertrophic scars and keloids are manifestations of the same fibroproliferative skin disorder and just differ in the intensity and duration of inflammation. These features may in turn be influenced by genetic, systemic, and local risk factors. It is possible that keloids arise largely as a result of genetic and systemic factors that promote massive and extended inflammation, while hypertrophic scars are more likely to be due to local factors. Genetic factors may include single nucleotide polymorphisms [4, 5], while systemic factors may include hypertension [6, 7], pregnancy [8, 9], hormones, and cytokines. The most important local factor is skin tension on the edges of the scar [10,11,12].
Our understanding of the pathogenesis of keloids and hypertrophic scars has improved markedly in the last 10 years, and these previously intractable scars are now regarded as being treatable. This has dramatically improved the quality of life of patients with these heavy scars [3]. There are many therapeutic options for keloids and hypertrophic scars, including surgery, radiation, corticosteroids, 5-fluorouracil, cryotherapy, laser therapy, anti-allergy agents, anti-inflammatory agents, bleaching creams, and make-up therapies. In terms of laser therapy, we have used long-pulsed 1064 nm Nd:YAG laser (Cutera Inc., Brisbane, CA) to treat keloids and hypertrophic scars and have reported its indications and limitations previously [13, 14].
2 Laser Therapies for Keloids and Hypertrophic Scars
Pulsed dye laser (PDL) has long been the therapy of choice for cutaneous vascular diseases, including telangiectasia, hemangioma, and vascular malformations [15,16,17]. It has also been used to treat keloids and hypertrophic scars because they have more blood vessels than normal skin. However, although PDL is effective for vascular diseases that affect the superficial skin layers (i.e., the epidermis and the papillary layer of the dermis), it does not penetrate deep enough to reach the deep dermal regions (i.e., the reticular layer of the dermis). Thus, PDL is not particularly effective for keloids and hypertrophic scars. By contrast, 1064 nm Nd:YAG laser reaches more deeply than PDL. As a result, it is increasingly being used to treat keloids and hypertrophic scars [13, 18,19,20,21]. It has been suggested that it acts by suppressing neovascularization and the dilatation of blood vessels.
Long-pulsed (not Q-switched) 1064 nm Nd:YAG laser plays an important role in our treatment algorithms for keloids and hypertrophic scars. This laser was developed for the treatment of vascular diseases, including inflammatory scars that exhibit neovascularization. It is also used to remove hair and to rejuvenate the skin [13]. The depth that is reached is determined by the spot size, the laser power, and the fluence: the larger the spot size, power, or fluence, the deeper the laser beam penetrates. Therefore, a large spot size and/or power are used for deep targets such as hair follicles and the blood vessels in the reticular layer of the dermis. However, since larger power increases the risk of cutaneous burn injury, the power should be determined on a case-by-case basis.
3 Indications and Limitations of Long-Pulsed 1064 nm Nd:YAG Laser for Keloids and Hypertrophic Scars
Keloid and hypertrophic scar development is due to chronic inflammation of the dermis during the course of wound healing. This associates with prolonged angiogenesis and collagen production. As mentioned above, long-pulsed 1064 nm Nd:YAG laser treatment may effectively treat keloid and hypertrophic scars because it reduces their vascularity. This reduction in vascularity may in turn decrease cytokine or growth factor levels in the tissue, which then promote collagen deposition. This notion is supported by the ability of several vascularity-suppressing treatments to improve inflammation and thereby ameliorate abnormal scars. One such treatment may be compression therapy, which is widely used with heavy scars, especially for hypertrophic scars that arise from burn wounds. This therapy may force the collapse of blood vessels in the scar, thereby decreasing cytokine or growth factor levels in the tissue. Moreover, it has been suggested that radiation therapy is effective for keloids because it suppresses angiogenesis. However, studies elucidating the mechanisms underlying long-pulsed 1064 nm Nd:YAG laser treatment efficacy in abnormal scars are warranted.
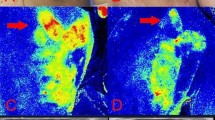
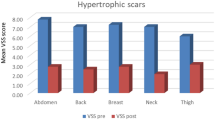
Our previous study [13] suggests that repeated tension on the edges of scars that is imposed by body movements prolongs scar inflammation: we observed that the patterns of mechanical force distribution around keloids and hypertrophic scars are largely consistent with the shape of the scar. In particular, our study suggests that keloids grow into the direction of the dominant prevailing skin tension. This mechanism explains why keloids on different regions of the body adopt specific shapes, such as the butterfly on the shoulder, the dumbbell on the upper arm, and the crab’s claw on the anterior chest. These observations suggest that, if scars will continue to be subjected to strong tension due to the daily movements of the body, long-pulsed 1064 nm Nd:YAG laser will not be successful. Indeed, our experience suggests that scars on less stretched areas (i.e., the face and anterior lower leg) respond better to this therapy than scars on highly stretched areas (i.e., the anterior chest wall and scapula). We also found that (1) less inflamed scars (i.e., the typical hypertrophic scar) (◘ Figs. 32.1, 32.2, and 32.3) respond better than highly inflamed scars (i.e., the typical keloid) (◘ Figs. 32.4, 32.5, and 32.6); (2) thinner scars respond better than thick scars; (3) small scars respond better than large scars; (4) single scars respond better than multiple scars (◘ Fig. 32.7); and (5) if even a little scar redness and induration remains after long-pulsed 1064 nm Nd:YAG laser treatment, these scars are highly likely to recur.
Upper lip hypertrophic scar. Left: before treatment. Right: 1 year after treatment. Two years before her referral to our clinic, a 20-year-old female received an abrasion injury to her upper lip that turned into a hypertrophic scar. Long-pulsed 1064 nm Nd:YAG laser was used at the following settings: 5 mm spot diameter, 65–70 J/cm2, 25 ms, and 2 Hz. After 1 year of this treatment, the scar continued to exhibit a textural difference, but its redness and elevation had improved. (This figure is cited from Ref. [13] with approval from the publisher. © All rights reserved)
Lower lip hypertrophic scar. Left: before treatment. Right: 1 year after treatment. One year before her referral to our clinic, an 11-year-old female received an abrasion injury to her lower lip that developed into hypertrophic scars. Long-pulsed 1064 nm Nd:YAG laser was used at the following settings: 5 mm spot diameter, 60–70 J/cm2, 25 ms, and 2 Hz. After 1 year of treatment, the scars continued to display textural differences and elevation, but there was clear improvement in their redness. (This figure is cited from Ref. [13] with approval from the publisher. © All rights reserved)
Abdomen hypertrophic scar. Upper: before treatment. Lower: 1 year after treatment. Four years before her referral to our clinic, a 50-year-old female developed hypertrophic scars on her abdomen after uterine myoma surgery. Long-pulsed 1064 nm Nd:YAG laser was used at the following settings: 5 mm spot diameter, 75 J/cm2, 25 ms, and 2 Hz. After 1 year of treatment, the scar had almost disappeared. (This figure is cited from Ref. [13] with approval from the publisher. © All rights reserved)
Anterior chest wall keloid. Left: before treatment. Right: 1 year after treatment. Eleven years before her referral to our clinic, a 29-year-old female developed butterfly-shaped keloids on her anterior chest. Treatment with steroid ointment and tape at other clinics did not improve these scars. Long-pulsed Nd:YAG laser was used at the following settings: 5 mm spot diameter, 65–75 J/cm2, 25 ms, and 2 Hz. After 1 year of treatment, the textural differences and elevation had improved but there was remaining redness on some parts. (This figure is cited from Ref. [13] with approval from the publisher. © All rights reserved)
Shoulder keloid. Left: before treatment. Right: 30 months after treatment. About 20 years before her referral to our clinic, a 52-year-old female developed butterfly-shaped keloids on her upper arm and shoulder. Long-pulsed 1064 nm Nd:YAG laser was used at the following settings: 5 mm spot diameter, 70–75 J/cm2, 25 ms, and 2 Hz. After 1 year of treatment, there were clear improvements in the textural differences and elevation but there was remaining redness on some parts. There was also some capillary dilation that was the result of steroid injections in the past. (This figure is cited from Ref. [13] with approval from the publisher)
Scapular keloid. Left: before treatment. Right: 3 years after treatment. About 30 years before her referral to our clinic, a 52-year-old female developed a butterfly-shaped keloid on her scapula. Steroid injections and tape at other clinics yielded little improvement. Long-pulsed 1064 nm Nd:YAG laser was used at the following settings: 5 mm spot diameter, 70–75 J/cm2, 25 ms, and 2 Hz. After 2 years of treatment, the texture, redness, induration, and elevation of the scar had clearly improved. (This figure is cited from Ref. [13] with approval from the publisher)
Scapular keloid. Left images: before treatment. Middle images: after 1 year of treatment. Right images: after 4 years of treatment. About 30 years before her referral to our clinic, a 42-year-old female developed multiple keloids on both the left (top images) and right (bottom images) scapular areas. The keloids had been slowly increasing in size. Steroid injections and tape treatment at other clinics yielded little improvement. Long-pulsed 1064 nm Nd:YAG laser was used at the following settings: 5 mm spot diameter, 75 J/cm2, 25 ms, and 2 Hz. Moreover, a Chinese herb (Saireito) was administered every day. After 4 years of treatment, the texture, redness, induration, and elevation of the scars have improved. However, the scars are not yet completely cured
4 Treatment Settings of Long-Pulsed 1064 nm Nd:YAG Laser for Keloids and Hypertrophic Scars
The laser should generally be applied to the skin surface with the following standard treatment settings: a spot diameter of 5 mm, an energy density of 75 J/cm2, an exposure time per pulse of 25 ms, and a repetition rate of 2 Hz. However, in the case of the face (◘ Figs. 32.1 and 32.2) or pediatric patients, the treatment should start with a lower energy density (60–70 J/cm2) to reduce the possibility of a burn injury. The best way to prevent such burn injuries is to cool the tip or air-cool the targeted skin before and immediately after irradiation. Each session should consist of three passes unless the patient feels strong pain at the second pass; in this case, the session should be stopped. Even if the patient feels no pain after the third pass, the session should be stopped. Local anesthesia is not necessary. However, if the patient expresses concern, anesthesia cream or tape can be used. The intervals between the sessions should generally be 2–4 weeks depending on the patient’s schedule.
Steroid tape is often used to decrease the inflammation in keloids and hypertrophic scars; this practice is particularly common in Japan and several other countries [22]. We use fludroxycortide tape (Drenison®, Dainippon Sumitomo Pharma Co., Ltd., Tokyo, Japan) with or without 1064-nm Nd:YAG laser (Cutera Inc., Brisbane, CA, USA) to treat pathological scars, including keloids and hypertrophic scars in recent years [23]. A retrospective cohort study [23] was performed to determine whether adding contact mode 1064-nm Nd:YAG laser therapy to conservative therapy (steroid tape) reduces the treatment time for hypertrophic Caesarean-section scars. In the results, combination of Nd:YAG laser and steroid tape treatment effectively decreased the total treatment time of hypertrophic Caesarean- section scars [23].
5 Follow-Up of Keloids and Hypertrophic Scars
It is important that patients with keloids and hypertrophic scars who undergo sequential treatments are followed up over the long term and that they are appropriately educated about scar management [3]. This is true regardless of the treatment that is being used. This is because, if patients develop pathological scars in the first place, they may be particularly prone to recurrence or the development of new pathological scars in response to minor stimulation. Thus, these patients should be educated in the self-management of both their abnormal scars and new wounds. In particular, they should be encouraged to apply steroid tape/plasters during the early stages of scar development. This will rapidly reduce the inflammation in the scar and improve its appearance. Moreover, laser therapy, anti-allergy agents (including tranilast), anti-inflammatory agents, bleaching creams, and make-up therapies can be used on a case-by-case basis [3].
6 Conclusion
Long-pulsed 1064 nm Nd:YAG laser has been used to treat keloids and hypertrophic scars. This laser was developed for the treatment of vascular diseases, including inflammatory scars that exhibit neovascularization. The depth that is reached is determined by the spot size, the laser power, and the fluence: the larger the spot size, power, or fluence, the deeper the laser beam penetrates. The standard treatment setting is a spot diameter of 5 mm, an energy density of 75 J/cm2, an exposure time per pulse of 25 ms, and a repetition rate of 2 Hz. Moreover, it is important that patients with keloids and hypertrophic scars who undergo sequential treatments are followed up over the long term and that they are appropriately educated about scar management.
References
Tredget EE, Nedelec B, Scott PG, Ghahary A. Hypertrophic scars, keloids, and contractures. The cellular and molecular basis for therapy. Surg Clin North Am. 1997;77(3):701–30.
Huang C, Murphy GF, Akaishi S, Ogawa R. Keloids and hypertrophic scars: update and future directions. Plast Reconstr Surg Glob Open. 2013;1(4):e25.
Ogawa R, Akaishi S, Kuribayashi S, Miyashita T. Keloids and hypertrophic scars can now be cured completely: recent progress in our understanding of the pathogenesis of keloids and hypertrophic scars and the most promising current therapeutic strategy. J Nippon Med Sch. 2016;83(2):46–53.
Nakashima M, Chung S, Takahashi A, Kamatani N, Kawaguchi T, Tsunoda T, Hosono N, Kubo M, Nakamura Y, Zembutsu H. A genome-wide association study identifies four susceptibility loci for keloid in the Japanese population. Nat Genet. 2010;42(9):768–71.
Ogawa R, Watanabe A, Than Naing B, Sasaki M, Fujita A, Akaishi S, Hyakusoku H, Shimada T. Associations between keloid severity and single-nucleotide polymorphisms: importance of rs8032158 as a biomarker of keloid severity. J Invest Dermatol. 2014;134(7):2041–3.
Arima J, Huang C, Rosner B, Akaishi S, Ogawa R. Hypertension: a systemic key to understanding local keloid severity. Wound Repair Regen. 2015;23(2):213–21.
Huang C, Ogawa R. The link between hypertension and pathological scarring: does hypertension cause or promote keloid and hypertrophic scar pathogenesis? Wound Repair Regen. 2014;22(4):462–6.
Moustafa MF, Abdel-Fattah MA, Abdel-Fattah DC. Presumptive evidence of the effect of pregnancy estrogens on keloid growth. Case report. Plast Reconstr Surg. 1975;56(4):450–3.
Mendelsohn ME, Karas RH. Estrogen and the blood vessel wall. Curr Opin Cardiol. 1994;9(5):619–26.
Ogawa R, Okai K, Tokumura F, Mori K, Ohmori Y, Huang C, Hyakusoku H, Akaishi S. The relationship between skin stretching/contraction and pathologic scarring: the important role of mechanical forces in keloid generation. Wound Repair Regen. 2012;20(2):149–57.
Ogawa R, Akaishi S, Huang C, Dohi T, Aoki M, Omori Y, Koike S, Kobe K, Akimoto M, Hyakusoku H. Clinical applications of basic research that shows reducing skin tension could prevent and treat abnormal scarring: the importance of fascial/subcutaneous tensile reduction sutures and flap surgery for keloid and hypertrophic scar reconstruction. J Nippon Med Sch. 2011;78(2):68–76.
Akaishi S, Akimoto M, Ogawa R, Hyakusoku H. The relationship between keloid growth pattern and stretching tension: visual analysis using the finite element method. Ann Plast Surg. 2008;60(4):445–51.
Koike S, Akaishi S, Nagashima Y, Dohi T, Hyakusoku H, Ogawa R. Nd:YAG laser treatment for keloids and hypertrophic scars: an analysis of 102 cases. Plast Reconstr Surg Glob Open. 2015;2(12):e272.
Akaishi S, Koike S, Dohi T, Kobe K, Hyakusoku H, Ogawa R. Nd:YAG laser treatment of keloids and hypertrophic scars. Eplasty. 2012;12:e1.
Dover JS, Arndt KA. New approaches to the treatment of vascular lesions. Lasers Surg Med. 2000;26(2):158–63.
Alster TS, Williams C. Treatment of keloid sternotomy scars with 585 nm flashlamp-pumped pulsed-dye laser. Lancet. 1995;345:1198–200.
Paquet P, Hermanns JF, Pierard GE. Effect of the 585nm flash-pumped pulsed dye laser for the treatment of keloids. Dermatol Surg. 2001;27(2):171–4.
Dragoni F, Bassi A, Cannarozzo G, Bonan P, Moretti S, Campolmi P. Successful treatment of acne keloidalis nuchae resistant to conventional therapy with 1064-nm ND:YAG laser. G Ital Dermatol Venereol. 2013;148(2):231–2.
Rossi A, Lu R, Frey MK, Kubota T, Smith LA, Perez M. The use of the 300 microsecond 1064 nm Nd:YAG laser in the treatment of keloids. J Drugs Dermatol. 2013;12(11):1256–62.
Al-Mohamady AE, Ibrahim SM, Muhammad MM. Pulsed dye laser versus long-pulsed Nd:YAG laser in the treatment of hypertrophic scars and keloid: a comparative randomized split-scar trial. J Cosmet Laser Ther. 2016;8:1–5.
Tian WC. Savior of post-blepharoepicanthoplasty scarring: novel use of a low-fluence 1064-nm Q-switched Nd:YAG laser. J Cosmet Laser Ther. 2016;18(2):69–71.
Goutos I, Ogawa R. Steroid tape: a promising adjunct to scar management. Scars Burn Heal. 2017;3:2059513117690937.
Tsai CH, Kao HK, Akaishi S, An-Jou Lin J, Ogawa R. Combination of 1,064-nm Neodymium-doped Yttrium Aluminum Garnet Laser and Steroid Tape. Decreases the Total Treatment Time of Hypertrophic Scars: An Analysis of 40 Cases of Cesarean-Section Scars [published online ahead of print, 2019 Nov 5]. Dermatol Surg. 2019;10.1097/DSS.0000000000002235.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2020 The Author(s)
About this chapter
Cite this chapter
Ogawa, R. (2020). Long-Pulsed 1064 nm Nd:YAG Laser Treatment for Keloids and Hypertrophic Scars. In: Téot, L., Mustoe, T.A., Middelkoop, E., Gauglitz, G.G. (eds) Textbook on Scar Management. Springer, Cham. https://doi.org/10.1007/978-3-030-44766-3_32
Download citation
DOI: https://doi.org/10.1007/978-3-030-44766-3_32
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-44765-6
Online ISBN: 978-3-030-44766-3
eBook Packages: MedicineMedicine (R0)