Abstract
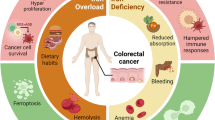
Cancer metabolism is a well-known target of cancer therapeutics. Classically, cancer metabolism has been studied in terms of the dependence of cancer cells on crucial metabolites, such as glucose and glutamine. But, the accumulating data show that iron metabolism in tumor microenvironment is also an important factor in preserving the survival of cancer cells. Cancer cells have a distinct phenotype of iron metabolism, which secures the much-needed iron for these metabolically active cells. In order to use this iron efficiently, cancer cells need to increase their iron supply and decrease iron loss. As recent research suggests, this is not only done by modifying the expression of iron-related proteins in cancer cells, but also by interaction of cancer cells with other cells from the tumor milieu. Tumor microenvironment is a dynamic environment characterized with intricate relationship between cancer cells, tumor-associated macrophages, fibroblasts, and other cells. Some of the mechanistic aspects of this relationship have been elucidated, while others are yet to be identified. In any case, identifying the details of the iron phenotype of the cells in tumor microenvironment presents with a new therapeutic opportunity to treat this deadly disease.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
DelNero P, Hopkins BD, Cantley LC, Fischbach C (2018) Cancer metabolism gets physical. Sci Transl Med 10:eaaq1011
Torti SV, Manz DH, Paul BT, Blanchette-Farra N, Torti FM (2018) Iron and Cancer. Annu Rev Nutr 38:97–125
Manz DH, Blanchette NL, Paul BT, Torti FM, Torti SV (2016) Iron and cancer: recent insights. Ann N Y Acad Sci 1368:149–161
Masaldan S, Clatworthy SAS, Gamell C, Meggyesy PM, Rigopoulos AT, Haupt S et al (2018) Iron accumulation in senescent cells is coupled with impaired ferritinophagy and inhibition of ferroptosis. Redox Biol 14:100–115
Sánchez M, Sabio L, Gálvez N, Capdevila M, Dominguez-Vera JM (2017) Iron chemistry at the service of life. IUBMB Life 69:382–388
Ebina Y, Okada S, Hamazaki S, Ogino F, Li JL, Midorikawa O (1986) Nephrotoxicity and renal cell carcinoma after use of iron- and aluminum-nitrilotriacetate complexes in rats. J Natl Cancer Inst 76:107–113
Akatsuka S, Yamashita Y, Ohara H, Liu Y-T, Izumiya M, Abe K et al (2012) Fenton reaction induced cancer in wild type rats recapitulates genomic alterations observed in human cancer. PLoS One 7:e43403
Zhang F, Wang W, Tsuji Y, Torti SV, Torti FM (2008) Post-transcriptional modulation of iron homeostasis during p53-dependent growth arrest. J Biol Chem 283:33911–33918
Chanvorachote P, Luanpitpong S (2016) Iron induces cancer stem cells and aggressive phenotypes in human lung cancer cells. Am J Physiol Cell Physiol 310:C728–C739
Vela D, Vela-Gaxha Z (2018) Differential regulation of hepcidin in cancer and non-cancer tissues and its clinical implications. Exp Mol Med 50:e436
Straud S, Zubovych I, de Brabander JK, Roth MG (2010) Inhibition of iron uptake is responsible for differential sensitivity to V-ATPase inhibitors in several cancer cell lines. PLoS One 5:e11629
Miles AL, Burr SP, Grice GL, Nathan JA (2017) The vacuolar-ATPase complex and assembly factors, TMEM199 and CCDC115, control HIF1α prolyl hydroxylation by regulating cellular iron levels. elife 6:e22693
Wang Y, Yu L, Ding J, Chen Y (2019) Iron metabolism in cancer. Int J Mol Sci 20:95
Ornstein DL, Zacharski LR (2007) Iron stimulates urokinase plasminogen activator expression and activates NF-kappa B in human prostate cancer cells. Nutr Cancer 58:115–126
Wang W, Deng Z, Hatcher H, Miller LD, Di X, Tesfay L et al (2014) IRP2 regulates breast tumor growth. Cancer Res 74:497–507
Babu KR, Muckenthaler MU (2019) miR-148a regulates expression of the transferrin receptor 1 in hepatocellular carcinoma. Sci Rep 9:1518
Johnson IRD, Parkinson-Lawrence EJ, Shandala T, Weigert R, Butler LM, Brooks DA (2014) Altered endosome biogenesis in prostate cancer has biomarker potential. Mol Cancer Res 12:1851–1862
Wang B, Zhang J, Song F, Tian M, Shi B, Jiang H et al (2016) EGFR regulates iron homeostasis to promote cancer growth through redistribution of transferrin receptor 1. Cancer Lett 381:331–340
Kovar J, Naumann PW, Stewart BC, Kemp JD (1995) Differing sensitivity of non-hematapoietic human tumors to synergistic anti-transferrin receptor monoclonal antibodies and deferoxamine in vitro. Pathobiology 63:65–70
Xue X, Ramakrishnan SK, Weisz K, Triner D, Xie L, Attili D et al (2016) Iron uptake via DMT1 integrates cell cycle with JAK-STAT3 signaling to promote colorectal tumorigenesis. Cell Metab 24:447–461
Gomes IM, Maia CJ, Santos CR (2012) STEAP proteins: from structure to applications in cancer therapy. Mol Cancer Res 10:573–587
Jin Y, Wang L, Qu S, Sheng X, Kristian A, Mælandsmo GM et al (2015) STAMP 2 increases oxidative stress and is critical for prostate cancer. EMBO Mol Med 7:315–331
Whitton B, Okamoto H, Packham G, Crabb SJ (2018) Vacuolar ATPase as a potential therapeutic target and mediator of treatment resistance in cancer. Cancer Med 7:3800–3811
Zhang X, Hua L, Yan D, Zhao F, Liu J, Zhou H et al (2016) Overexpression of PCBP2 contributes to poor prognosis and enhanced cell growth in human hepatocellular carcinoma. Oncol Rep 36:3456–3464
Li F, Bullough KZ, Vashisht AA, Wohlschlegel JA, Philpott CC (2016) Poly(rC)-binding protein 2 regulates hippo signaling to control growth in breast epithelial cells. Mol Cell Biol 36:2121–2131
Chen C, Lei J, Zheng Q, Tan S, Ding K, Yu C (2018) Poly(rC) binding protein 2 (PCBP2) promotes the viability of human gastric cancer cells by regulating CDK2. FEBS Open Bio 8:764–773
Deng Z, Manz DH, Torti SV, Torti FM (2017) Iron-responsive element-binding protein 2 plays an essential role in regulating prostate cancer cell growth. Oncotarget 8:82231–82243
Khiroya H, Moore JS, Ahmad N, Kay J, Woolnough K, Langman G et al (2017) IRP2 as a potential modulator of cell proliferation, apoptosis and prognosis in nonsmall cell lung cancer. Eur Respir J 49:1600711
Horniblow RD, Bedford M, Hollingworth R, Evans S, Sutton E, Lal N et al (2017) BRAF mutations are associated with increased iron regulatory protein-2 expression in colorectal tumorigenesis. Cancer Sci 108:1135–1143
Ward DM, Kaplan J (1823) Ferroportin-mediated iron transport: expression and regulation. Biochim Biophys Acta, Mol Cell Res 2012:1426–1433
Pinnix ZK, Miller LD, Wang W, D’Agostino R, Kute T, Willingham MC et al (2010) Ferroportin and iron regulation in breast cancer progression and prognosis. Sci Transl Med 2:43ra56
Deng Z, Manz DH, Torti SV, Torti FM (2019) Effects of ferroportin-mediated iron depletion in cells representative of different histological subtypes of prostate cancer. Antioxid Redox Signal 30:1043–1061
Zhang S, Chen Y, Guo W, Yuan L, Zhang D, Xu Y et al (2014) Disordered hepcidin-ferroportin signaling promotes breast cancer growth. Cell Signal 26:2539–2550
Gu Z, Wang H, Xia J, Yang Y, Jin Z, Xu H et al (2015) Decreased ferroportin promotes myeloma cell growth and osteoclast differentiation. Cancer Res 75:2211–2221
Porporato PE, Filigheddu N, Pedro JMBS, Kroemer G, Galluzzi L (2018) Mitochondrial metabolism and cancer. Cell Res 28:265–280
Vela D (2019) Keeping heart homeostasis in check through the balance of iron metabolism. Acta Physiol 228:e13324. https://doi.org/10.1111/apha.13324
Fryknäs M, Zhang X, Bremberg U, Senkowski W, Olofsson MH, Brandt P et al (2016) Iron chelators target both proliferating and quiescent cancer cells. Sci Rep 6:38343
Sandoval-Acuña C, Tomkova V, Cardenas NT, Neuzil J, Repkova K, Stursa J et al (2018) Mitochondrial iron chelation as a novel anti-cancer strategy. Free Radic Biol Med 120(Supp. 1):S61
Wu KJ, Polack A, Dalla-Favera R (1999) Coordinated regulation of iron-controlling genes, H-ferritin and IRP2, by c-MYC. Science 283:676–679
Tsuji Y, Kwak E, Saika T, Torti SV, Torti FM (1993) Preferential repression of the H subunit of ferritin by adenovirus E1A in NIH-3T3 mouse fibroblasts. J Biol Chem 268:7270–7275
Ozaki T, Nakagawara A (2011) Role of p53 in cell death and human cancers. Cancers 3:994–1013
Jiang X, Zhang C, Qi S, Guo S, Chen Y, Du E et al (2016) Elevated expression of ZNF217 promotes prostate cancer growth by restraining ferroportin-conducted iron egress. Oncotarget 7:84893–84906
Li JL, Okada S, Hamazaki S, Ebina Y, Midorikawa O (1987) Subacute nephrotoxicity and induction of renal cell carcinoma in mice treated with ferric nitrilotriacetate. Cancer Res 47:1867–1869
Vela D (2018) Iron metabolism in prostate cancer; from basic science to new therapeutic strategies. Front Oncol 8:547
Lin Y, Xu J, Lan H (2019) Tumor-associated macrophages in tumor metastasis: biological roles and clinical therapeutic applications. J Hematol Oncol 12:76
Gollapudi K, Galet C, Grogan T, Zhang H, Said JW, Huang J et al (2013) Association between tumor-associated macrophage infiltration, high grade prostate cancer, and biochemical recurrence after radical prostatectomy. Am J Cancer Res 3:523–529
Recalcati S, Locati M, Marini A, Santambrogio P, Zaninotto F, De Pizzol M et al (2010) Differential regulation of iron homeostasis during human macrophage polarized activation. Eur J Immunol 40:824–835
Jung M, Mertens C, Bauer R, Rehwald C, Brüne B (2017) Lipocalin-2 and iron trafficking in the tumor microenvironment. Pharmacol Res 120:146–156
Mertens C, Mora J, Ören B, Grein S, Winslow S, Scholich K et al (2018) Macrophage-derived lipocalin-2 transports iron in the tumor microenvironment. Onco Targets Ther 7:e1408751
Jung M, Ören B, Mora J, Mertens C, Dziumbla S, Popp R et al (2016) Lipocalin 2 from macrophages stimulated by tumor cell-derived sphingosine-1-phosphate promotes lymphangiogenesis and tumor metastasis. Sci Signal 9:ra64
Mertens C, Akam EA, Rehwald C, Brüne B, Tomat E, Jung M (2016) Intracellular iron chelation modulates the macrophage iron phenotype with consequences on tumor progression. PLoS One 11:e0166164
Prill S, Rebstock J, Tennemann A, Körfer J, Sönnichsen R, Thieme R et al (2019) Tumor-associated macrophages and individual chemo-susceptibility are influenced by iron chelation in human slice cultures of gastric cancer. Oncotarget 10:4731–4742
Leftin A, Ben-Chetrit N, Joyce JA, Koutcher JA (2019) Imaging endogenous macrophage iron deposits reveals a metabolic biomarker of polarized tumor macrophage infiltration and response to CSF1R breast cancer immunotherapy. Sci Rep 9:857
Recalcati S, Gammella E, Cairo G (2019) Dysregulation of iron metabolism in cancer stem cells. Free Radic Biol Med 133:216–220
Basuli D, Tesfay L, Deng Z, Paul B, Yamamoto Y, Ning G et al (2017) Iron addiction: a novel therapeutic target in ovarian cancer. Oncogene 36:4089–4099
Kanojia D, Zhou W, Zhang J, Jie C, Lo PK, Wang Q et al (2012) Proteomic profiling of cancer stem cells derived from primary tumors of HER2/Neu transgenic mice. Proteomics 12:3407–3415
Schonberg DL, Miller TE, Wu Q, Flavahan WA, Das NK, Hale JS et al (2015) Preferential iron trafficking characterizes glioblastoma stem-like cells. Cancer Cell 28:441–455
Ninomiya T, Ohara T, Noma K, Katsura Y, Katsube R, Kashima H et al (2017) Iron depletion is a novel therapeutic strategy to target cancer stem cells. Oncotarget 8:98405–98416
Rychtarcikova Z, Lettlova S, Tomkova V, Korenkova V, Langerova L, Simonova E et al (2017) Tumor-initiating cells of breast and prostate origin show alterations in the expression of genes related to iron metabolism. Oncotarget 8:6376–6398
El Hout M, Dos Santos L, Hamaï A, Mehrpour M (2018) A promising new approach to cancer therapy: targeting iron metabolism in cancer stem cells. Semin Cancer Biol 53:125–138
Brabletz T, Kalluri R, Nieto MA, Weinberg RA (2018) EMT in cancer. Nat Rev Cancer 18:128–134
Liu W, Xing F, Iiizumi-Gairani M, Okuda H, Watabe M, Pai SK et al (2012) N-myc downstream regulated gene 1 modulates Wnt-β-catenin signalling and pleiotropically suppresses metastasis. EMBO Mol Med 4:93–108
Shan Z, Wei Z, Shaikh ZA (2018) Suppression of ferroportin expression by cadmium stimulates proliferation, EMT, and migration in triple-negative breast cancer cells. Toxicol Appl Pharmacol 356:36–43
Kobayashi H, Enomoto A, Woods SL, Burt AD, Takahashi M, Worthley DL (2019) Cancer-associated fibroblasts in gastrointestinal cancer. Nat Rev Gastroenterol Hepatol 16:282–295
Sandberg TP, Stuart MPME, Oosting J, Tollenaar RAEM, Sier CFM, Mesker WE (2019) Increased expression of cancer-associated fibroblast markers at the invasive front and its association with tumor-stroma ratio in colorectal cancer. BMC Cancer 19:284
Ippolito L, Morandi A, Taddei ML, Parri M, Comito G, Iscaro A et al (2019) Cancer-associated fibroblasts promote prostate cancer malignancy via metabolic rewiring and mitochondrial transfer. Oncogene 38:5339–5355
Blanchette-Farra N, Kita D, Konstorum A, Tesfay L, Lemler D, Hegde P et al (2018) Contribution of three-dimensional architecture and tumor-associated fibroblasts to hepcidin regulation in breast cancer. Oncogene 37:4013–4032
Lee S, Schmitt CA (2019) The dynamic nature of senescence in cancer. Nat Cell Biol 21:94–101
Chen T, Yang P, Wang H, He ZY (2017) Silence of long noncoding RNA PANDAR switches low-dose curcumin-induced senescence to apoptosis in colorectal cancer cells. Onco Targets Ther 10:483–491
Jiao Y, Wilkinson J IV, Christine Pietsch E, Buss JL, Wang W, Planalp R et al (2006) Iron chelation in the biological activity of curcumin. Free Radic Biol Med 40:1152–1160
Hassannia B, Vandenabeele P, Vanden BT (2019) Targeting ferroptosis to iron out cancer. Cancer Cell 35:830–849
Dixon SJ, Stockwell BR (2019) The hallmarks of ferroptosis. Annu Rev Cancer Biol 3:35–54
Ma S, Henson ES, Chen Y, Gibson SB (2016) Ferroptosis is induced following siramesine and lapatinib treatment of breast cancer cells. Cell Death Dis 7:e2307
Geng N, Shi B-J, Li S-L, Zhong Z-Y, Li Y-C, Xua W-L et al (2018) Knockdown of ferroportin accelerates erastin-induced ferroptosis in neuroblastoma cells. Eur Rev Med Pharmacol Sci 22:3826–3836
Mai TT, Hamaï A, Hienzsch A, Cañeque T, Müller S, Wicinski J et al (2017) Salinomycin kills cancer stem cells by sequestering iron in lysosomes. Nat Chem 9:1025–1033
Sui S, Zhang J, Xu S, Wang Q, Wang P, Pang D (2019) Ferritinophagy is required for the induction of ferroptosis by the bromodomain protein BRD4 inhibitor (+)-JQ1 in cancer cells. Cell Death Dis 10:331. https://doi.org/10.1038/s41419-019-1564-7
Sun Y, Li C, Feng J, Li Y, Zhai X, Zhang L et al (2019) Ferritinophagic flux activation in CT26 cells contributed to EMT inhibition induced by a novel iron chelator, DpdtpA. Oxid Med Cell Longev 2019:1–14
Tury S, Assayag F, Bonin F, Chateau-Joubert S, Servely JL, Vacher S et al (2018) The iron chelator deferasirox synergises with chemotherapy to treat triple-negative breast cancers. J Pathol 246:103–114
Miller LD, Coffman LG, Chou JW, Black MA, Bergh J, D’Agostino R et al (2011) An iron regulatory gene signature predicts outcome in breast cancer. Cancer Res 71:6728–6737
Toshiyama R, Konno M, Eguchi H, Asai A, Noda T, Koseki J et al (2018) Association of iron metabolic enzyme hepcidin expression levels with the prognosis of patients with pancreatic cancer. Oncol Lett 15:8125–8133
Kalaydina RV, Bajwa K, Qorri B, Decarlo A, Szewczuk MR (2018) Recent advances in “smart” delivery systems for extended drug release in cancer therapy. Int J Nanomedicine 13:4727–4745
Camp ER, Wang C, Little EC, Watson PM, Pirollo KF, Rait A et al (2013) Transferrin receptor targeting nanomedicine delivering wild-type p53 gene sensitizes pancreatic cancer to gemcitabine therapy. Cancer Gene Ther 20:222–228
Senzer N, Nemunaitis J, Nemunaitis D, Bedell C, Edelman G, Barve M et al (2013) Phase I study of a systemically delivered p53 nanoparticle in advanced solid tumors. In: Molecular Therapy, vol 21. Nature Publishing Group, New York, pp 1096–1103
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Vela, D. (2020). Iron in the Tumor Microenvironment. In: Birbrair, A. (eds) Tumor Microenvironment. Advances in Experimental Medicine and Biology, vol 1259. Springer, Cham. https://doi.org/10.1007/978-3-030-43093-1_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-43093-1_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-43092-4
Online ISBN: 978-3-030-43093-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)