Abstract
In this chapter we argue that a genuine revision of the norms and practices in clinical work needs to start from a revision of the way we think about the world, and in particular the way we think about the most foundational concepts, such as causality. We present the dispositionalist theory of causality and explain why this theory is better suited for the clinic than the orthodox Humean theory which motivated the EBM framework. We argue that causality ought to be understood as something singular and intrinsic rather than as a pattern of regularity across different contexts. From a dispositionalist perspective, causal knowledge ought to start from the single case. In the clinic, this means that the more we know about the multiple dispositions that are involved and how they interact in this specific context, the better equipped we will be to make good and relevant explanations, predictions and decisions for the individual seeking care.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
I have been working as a regular GP for many years and experienced how useful it is to know patients as persons. Through repeated encounters over time, I became familiar with many of my patients as persons—who they were and how they lived their lives—whether I was aiming for it or not.
Although such information may be of medical relevance, it is rarely written down in the medical records. In many aspects, it is tacit knowledge. Nevertheless, as General Practitioners we use this kind of knowledge all the time in everyday medical practice, tailoring the approach and follow-up of individual patients, especially when we are dealing with the patients we see the most.
There is also a growing body of research documenting that adverse life experiences can have a decisive impact on people’s health. However, traditional biomedicine, the dominant perspective through which today’s medical practice is conceptualised, has placed little emphasis on expert findings, such as those within modern stress physiology, indicating that biographical and person-related knowledge has medical relevance.
Bente Prytz Mjølstad, ‘Does your regular GP know you – as a person?’, CauseHealth blog (https://causehealthblog.wordpress.com/2017/11/09)
1 The Similar and the Unique
From the biomedical perspective, medicine primarily deals with what is common for all: cells, tissues, organs, anatomy and biological processes and interactions. In the clinical encounter, however, one has to also deal with what is particular and unique. But how much space should the practitioner give to evidence that is specific to the single patient? Given that time and resources are limited, the highest priority must be given to the clearly defined medical facts. Then, if there is time, one can talk to the patient about other and more personal matters. Or so one might argue.
In the quotation above, general practitioner Bente Prytz Mjølstad offers a different perspective. She suggests that knowing the patient as a person might also help the clinician to better understand their medical condition and medical needs. Perhaps, then, knowledge of what is unique to a patient ought to be given a higher priority in the clinic. Or would that take time and resources away from what is most important: to understand, diagnose and treat the patient? In the CauseHealth project, we have met a number of practitioners who emphasise the importance of patient narratives, and who use the patient’s perspective and story as a source of valuable medical information (many of these have contributed to Part II of this book). Immunologist and psychotherapist Brian Broom describes this as follows:
Sometimes people wonder why I am so keen on the ‘story’. It is simply that we clinicians who want to practice in a whole person way need practical doorways into the world of the whole person, and especially that part of the person’s world not accessed by the normal biomedical approach to disease. The latter, as currently practised, focuses on the expertise of information-holding, the power of drugs and physical interventions, activities directed at restoring, repairing and compensating for ‘mechanical’ deficits and distortions, and so on. I greatly value the benefits of much of this.
But listening for the patient’s story opens up an entirely different world, and its power derives from quite a different set of assumptions, attitudes and relational values. Asking for a story may seem a simple matter but the implications are hugely important. In reality, most of the stories implicated in illness are relational stories: of trauma, failure, loss, abuse, abandonment, manipulation, and much more. We are all fundamentally relational…
We don’t need to be a psychologist or psychotherapist to start this process, or to make simple connections, or to give the patient permission and encouragement to consider the connections. The interaction doesn’t have to be perfect, or prolonged, or all done at once. Patients know that we are persons too, and have limits on our capacities. We can be good-enough.
Brian Broom, ‘Imagination and its companions’, CauseHealth blog (https://causehealthblog.wordpress.com/2017/07/03)
Clinicians might see an advantage in knowing more about their patients’ stories, for the purpose of finding the causes of health and illness and for making predictions about treatment and recovery. But there is little support for patient stories within current medical thinking. In evidence based medicine and practice, information from the single patient is not generally treated as strong evidence, at least not of causality. One might even refer to the experience of individuals as ‘subjective’ or ‘anecdotal’, suggesting that their stories are relevant mainly for themselves and not scientifically valid for claiming, for instance, that a certain factor contributed to a certain condition. A question we should ask is then: at what point does information from individual patients become causal evidence (see also Kerry, Chap. 13, this book)? Is there a threshold at which anecdotes transform into evidence, for instance when there is a sufficient number of individuals who report similar experiences?
Say a patient reports experiencing a possible side effect from a prescribed medicine. If no one else using the medicine has reported the same side effect, one might be reluctant to conclude that the medicine caused that effect, and for good reasons. But if, after a few years on the market, a sufficient number of people using the medicine report the same reaction, it might be concluded that it is a side effect after all.
From an epistemological perspective, meaning from the perspective of what we can or cannot know, this is reasonable. If one knows little about the medicine’s causal mechanisms, a single report is not itself sufficient evidence of causality. But if one thinks that 10, 100 or 1000 reports amounts to sufficient causal evidence, then didn’t causality happen within each of these individuals? So even if the first patient reporting the effect was not sufficient evidence of this causal link, it does not follow that causality did not happen also in that instant. Lack of evidence does not imply lack of causality: we cannot conclude that there is no causality happening in that particular person, ontologically, simply because we, epistemologically, lack evidence of causality. Ontologically, meaning from the perspective of what does or does not exist, if causality happens, it does so in the particular instance and does not depend on what happens in other cases to similar patients.
Simply put…
Ontology concerns reality: what exists or happens in the world.
Epistemology concerns knowledge: what we can and cannot know about reality.
Example: Ontologically, one might have a rare genetic disease even if one has yet not discovered it. Lack of knowledge does, therefore, not entail lack of reality. Ontologically, the disease exists, but epistemologically, we don’t have any evidence or symptoms of it. In other situations, there might be symptoms or evidence of some disease that is not actually there, such as when a cancer screening gives a false positive. Epistemologically, there was evidence of cancer, but ontologically, there was no cancer.
Why is the distinction between epistemology and ontology important? First of all, if causality happens in the particular case (ontologically), this means that each individual patient represents a valuable source of evidence (epistemologically), also for causality. Secondly, this distinction also points to a tension in how we understand causality as a phenomenon. Philosophically it boils down to the question of whether there in principle could be a case of a unique causal event. Could causality happen only once and never be repeated throughout the whole history of time? This is an ontological question and not the same as the epistemological question of whether we could ever scientifically establish causality for such a unique case.
This question is relevant for the clinical encounter because it matters in terms of how one deals with medical uniqueness and individual variation. Should we place much weight on single case reports or patient stories of seemingly unique effects or experiences? Or must we wait for results from larger clinical studies to even consider causality?
In the original evidence hierarchy of evidence based medicine (EBM) (Fig. 2.1), patient narratives, or even case reports, do not count for much, at least not with respect to causality. The idea is that unless there is repetition, and preferably many repetitions, one simply cannot know if something is causally related. This places EBM within the philosophical tradition of empiricism and its emphasis on the observable. We will now see how empiricism has influenced our understanding of causality.
2 Empiricism: Causality Requires Repeated Observations
Historically, empiricism is the most influential view for how we understand causality, in philosophy and science in general. This view has itself been largely shaped by the empiricist philosopher David Hume and his famous work A Treatise of Human Nature from 1739. Hume was critical of ontology: he was skeptical about making claims about what ultimately exists. Indeed, he believed that all we can really know about the world is restricted by what we can experience through our senses. This is the empiricist assumption, namely that our observations are the only evidence we can have of reality. Positivism is the idea that science should be strictly empirical, and only deal with what can be observed and measured.
This scepticism toward ontology also meant that Hume was critical of any theory that says more than what can be backed up by data. If we try to explain what we observe by appealing to some general, underlying principle, this would be to say more than what we have evidence of. In practice, however, this might mean that all scientific theories have a speculative element to them, unless they simply report the available data. For Hume, therefore, as for any empiricist, epistemology trumps ontology.
Simply put…
Empiricism is the idea that we can only know what can be experienced through our senses. This means that all scientific knowledge should ultimately come from observation data.
Positivism is a strict empiricist view of science, stating that science should only deal with what can be established through observation and measurement, and that everything else is metaphysical speculations.
When analysing the concept of causality, Hume used the example of the billiard ball table. Here, we think that hitting the object ball with the cue ball causes the object ball to roll. But what do we actually observe on the table? Hume found three observable features of causality:
-
1.
The cause is perfectly correlated with its effect, so that every time the cause happens, the effect follows. He called this the constant conjunction of cause and effect.
-
2.
The cause always happens before the effect. He called this temporal priority.
-
3.
There must be some contact between cause and effect in time and space, so that the cause and effect meet. He called this contiguity.
What Hume could not observe, however, was any form of link or necessary connection between cause and effect. We cannot observe that also the next time the cause occurs, the effect will necessarily happen. If we have not observed this yet, we cannot infer that it will happen, even if we are convinced that it will.
To assume that what we have observed until now will be what we observe also in the future, is what Hume called an inductive inference. These inferences are logically invalid, since the conclusion goes beyond the premises. So we have seen something happening in the past, but then we infer that it will be the same in the future. This is something that we cannot know yet. When it comes to causality, therefore, all we can know is that it is a form of regularity, as specified by 1–3 above. We cannot infer from this that there is a causal law that guarantees the same pattern of regularity in the future, as this is yet to be observed.
Simply put…
Inductive inference is the process of drawing a conclusion by going beyond the available evidence. For example, one could infer a conclusion for a whole population from the results of a study conducted on a representative sample of such a population. Since the conclusion goes beyond the premises, we cannot be sure that inductive inferences are logically valid.
Hume’s is a very strict form of empiricism. To follow it up scientifically, we would have to constrain ourselves from making any form of general or theoretical claims that also involve future events. The law of gravitational attraction, for instance, might have worked in the past and the present, but whether it will work tomorrow is not yet evident. A causal law is then nothing but a claim that the cause and the effect have been repeatedly observed to follow one another in a certain way in the past.
This is now known as the regularity theory of causality, in which repetition is the key to calling something causality. From this perspective, the same cause should always give the same effect, at least under the same or similar conditions. Hume was quite insistent on this criterion for causality: ‘The same cause always produces the same effect, and the same effect never arises but from the same cause’ (Hume 1739, I, iii: 173). In the clinic, we might refer to a certain sub-population of patients that share some important features, such as their diagnosis. If these patients are given the same treatment, we might expect that they should also get the same effect from it. But we know that this is not generally the case. How can this be explained philosophically?
There is an important consequence of Hume’s principle, that same cause, gives same effect. If the effect is different, it can only mean that something was different in the cause, or in the background conditions. Hume seems to think of this as an undeniable truth about causality:
The difference in effects of two resembling objects must proceed from that particular, in which they differ. For as like causes always produce like effects, when in any instance we find our expectation to be disappointed, we must conclude that this irregularity proceeds from some difference in the causes. (Hume 1739, I, iii: 174)
Hume would then say that if two patients with the same diagnosis get different effects from the same treatment, there must be some other difference between them that is causally relevant. The question is which individual differences are causally relevant for the effect and which are not. We might expect sex, age and weight to be relevant, but many treatments work across these differences. One might still expect that if everything were the same between two patients, the same intervention should produce the same outcome. If so, this would be in accordance with Hume’s understanding of causality.
Another consequence of Hume’s theory is that there can be no unique instance of causality. Without the possibility of repetition, one cannot check whether the same cause always produces the same effect. Hume accepts this and even goes as far as to say that if the creation of the universe happened only once, it could not count as causal. The alternative to this view is the position called ‘causal singularism’, which will be discussed in the next section.
Although many philosophers might disagree with Hume in one or more of these features of causality, they might still agree with his empiricist starting point: (i) that the causal link itself is not directly observable and (ii) that causality must therefore be inferred from what we can actually observe. In science, however, there seems to be a general acceptance of Hume’s idea that same cause gives the same effect, and that any difference in the effect must come from a difference in the cause.
How does this relate to how we understand causality in clinical research? Assuming the empiricist ideal of science, causal relations should then be established from observation data, for instance of an intervention and its outcomes. From such data, one might be able to observe regularities, difference-makers or probability-raisers, all of which can be detected via statistical methods. If causality is accessible via observation data in this way, causal hypotheses and theories could in principle be generated directly from data.
Crucial for this understanding of causality is that one needs repetition. Statistical methods require large samples, or at least more than one or two individuals. In cases of individual variation, one at least needs an actual or assumed sub-population of which this patient is thought to be representative. A problem with a view of causality based on repetition, is that it leaves no room for causal uniqueness, as will be explained further in the next section. If all patients are different, having a unique biology, biography, life-style, diet, and so on, then no sub-group will perfectly represent them.
If repetition is a requirement for establishing causality, all causally relevant differences between individuals seem to fall outside the scope of a single study. From the clinical perspective this is a practical problem. How to deal with causality in cases of large individual variation? Or perhaps we should say in case of uniqueness when N = 1? This question was one of the main drivers for the Cause Health project.
3 Dispositionalism: Causality Happens in the Single Case
There are two ways to think about causal uniqueness. One is to think of it as a problem of causality, because we are then lacking the possibility of confirmation from other similar cases. The other way is to think of causal uniqueness as typical of causality, and therefore as the default expectation in any causal assessment. Causal dispositionalism represents the latter view, called ‘causal singularism’. This section presents a brief overview of the dispositionalist theory of causality and explain why it gives ontological and epistemological weight to the particular over the general.
The theory of causal dispositionalism was first introduced in Mumford and Anjum (2010) and is described in detail in their book Getting Causes from Powers (Mumford and Anjum 2011). We will now explain why the individual patient and their narrative should be at the heart of causal matters from a dispositionalist perspective.
Simply put…
Causal singularism is the ontological view that causality happens in the particular case and does not require repetition.
Example: The first person to die from a rare disease is a single and unique case up until the next person dies from it. But even in the first person, the disease caused their death, ontologically. So even if one might need more cases to establish causality, epistemologically, either in animal models or in a clinical study, causality happens in each individual case.
3.1 Causes Are Dispositions
Dispositions are also referred to as ‘causal powers’, ‘abilities’ (Mumford 1998) or ‘capacities’ (Cartwright 1989). They refer to what something can do. A sharp knife can cut, a medication can heal, and a virus can make an otherwise healthy person ill. A disposition is a type of property, but one that can exist unmanifested. Examples of dispositional properties are fragility, flammability, toxicity and fertility. A substance is toxic even when it is not harming anyone. And a person can be fertile throughout their life without reproducing. Causality typically happens when dispositions manifest themselves. A fertile woman becomes pregnant, toxic arsenic kills or some explosive substance explodes. In this sense, the dispositional property is a cause and the manifestation is an effect.
Whether something or someone has a disposition is not always observable until it is manifested. The ‘proof’ of a disposition’s existence thus lies in its manifestation. Empiricist philosophers have asked how we can even know that dispositions are real if they cannot be observed. Some dispositions might be possible to tease out by an intervention or a test, such as a fertility test. But there will always be dispositions that we simply cannot know of until they are manifested, and perhaps not even then. A person might have early stage cancer without manifesting any observable symptoms, but the causal process has nevertheless started. A disposition is thus not a pure possibility, like the possibility of flying cars in the future. It is a potentiality that exits in the world here and now as a real possibility in the properties of things.
Since empiricists trust only what can be observed (observability being another disposition), they take manifestations to be real but see dispositions as merely possibly real. This seems a plausible conclusion if we think that the dispositions are nowhere until they are manifested. But many dispositions are clearly present also before they manifest. For instance, a sharp knife has a disposition to cut through skin in virtue of the shape and material of the knife. If a knife was made of a material that was too soft to penetrate the skin, it would lack that disposition.
According to Hume, our knowledge about dispositions is inferred from what we have already observed elsewhere. Hume and neo-Humean philosophers, such as David Lewis, Stathis Psillos and Helen Beebee, are therefore sceptical of dispositions. They would therefore not include dispositions in their ontology unless they are analysed into something observable (Mumford 1998, 2004). The only reason why we think a wine glass is fragile, one might say, is because we have seen other wine glasses break from very little impact elsewhere. Whether a particular wine glass is actually fragile is thus something we cannot know until it breaks.
Epistemologically, this might be the case for many dispositions. But ontologically, at least, once the glass actually breaks, doesn’t this mean that it was in fact fragile? If we had to wait until a manifestation occurred in every case before we believed in its dispositions, we could not say that a nuclear power plant was explosive unless it explodes. Dispositionalists would therefore reject the strict empiricist principle, and argue that some things could be real even if they are not directly observable.
Dispositions are seen as plausibly real because they can explain what actually happens – the underlying principles of the behaviour of things. Causal effects without underlying dispositions would on this view be unaccounted for and remain an ontological mystery. The Humeans, on the other hand, would rather see everything that is not observable as representing the real mystery, but their motivation for saying so is primarily epistemological: we could not possibly know of something’s existence (ontology) unless we can observe it (epistemology).
Although some philosophers are sceptical of dispositions, these properties seem to play an important role in our lives. That we take dispositions seriously can be seen in how they influence our behaviour. We are careful around explosive, flammable or poisonous substances, and we don’t expose ourselves unecessarily to contagious diseases or let our children play with sharp knives. As Stephen Mumford puts it in the opening section of his book Dispositions (1998: 1), referring to Nelson Goodman, this is a world of threats and promises. And our behaviour very much reveals our understanding of dispositions as real and important.
How is this relevant for the clinic? One might from the observation of a heavy smoker’s lungs see that they are disposed to emphysema, chronic bronchitis and lung cancer. And if a person’s arteries are clogged by arterial plaques, aren’t they disposed to reduced blood flow and therefore to heart attack and stroke? In this sense, the current situation points toward a possible, or even likely, future. The dispositions might reveal the direction toward which the situation is heading: what tends to be (Anjum and Mumford 2018a). Dispositions are thus useful for making prognoses for illness and recovery, but also for making the correct diagnosis. Since many symptoms could be the manifestations of a range of illnesses, it is important for choosing the right treatment that it targets the right disposition. If a headache is caused by stress, the treatment will be different from if the headache is caused by a tumour in the brain. Similarly, if chronic depression is caused by a biological disposition or by childhood trauma or abuse, or both, the treatment scheme should reflect this difference (see also Hagen, Chap. 10, this book).
3.2 Causes Are Intrinsic
Dispositions are typically intrinsic properties, belonging to some particular individual or entity. That dispositions are intrinsic is crucial for the purpose of causality, since we should not say that a drug works unless it has an intrinsic property to bring about its effect. This is why medical interventions are typically tested against a placebo, to check whether the effect on recovery comes from the intervention or from the patient’s own expectations of recovery. We might say that the placebo effect is a manifestation of the patient’s dispositions, and not of dispositions belonging to the intervention.
That dispositions are intrinsic does not mean that they have to belong to an individual. Many dispositions belong to entities that are higher-level or even abstract. A community can be supportive, friendly, homophobic or xenophobic, for instance. A family can be loving or dysfunctional. A work environment can be stimulating or draining and a legal system can be racist. Some dispositions might only emerge at group level. As a community of people, we have social dispositions related to communication, relationships, politics and law. Arguably, none of these are intrinsic to the individual but emerge as a result of interactions with others (Anjum and Mumford 2017, see also Rocca and Anjum, Chap. 5, this book).
Simply put…
A disposition is an intrinsic property that can exist unmanifested and gives its bearer a causal power, ability or capacity.
Example: Someone can have a disposition toward a disease that is never manifested, just like a glass can be fragile without being broken.
3.3 Causality Is Complex
We said that whenever dispositions are manifested, causality happens. A fertile woman becomes pregnant, a fragile glass breaks, a medicine cures an illness: these are all examples of causality. It is, however, important to recognise that all such manifestations are a result of multiple dispositions working together. It takes much more than a fertile woman and her eggs to become pregnant. Without the sperm from a fertile man, for instance, and a prepared uterus with the correct balance of hormones, the pregnancy will not happen. All these are what we call the manifestation partners for pregnancy, a term initially used by Martin (2008). That something is an appropriate manifestation partner for a disposition means that they can produce an effect together that neither of them could have produced on their own.
From a dispositionalist perspective, all causality is complex in this sense, requiring the interaction of one or more mutual manifestation partners. When a match is struck and lights, this effect is caused by the striking as well as the flammable match, the dry wood and the oxygen. But rather than treating one of these as the cause and others as background conditions, they are all causes of the effect in virtue of their own dispositions. Some of these dispositions might be necessary for the effect, while others might be thought of as triggers. Still, everything that contributes to producing the effect are on the dispositionalist view causes.
Causal complexity is particularly important to recognise in the clinic, since one cannot focus only on the medical intervention when treating a patient. What an intervention does on population level is one thing, but in this case, it will be interacting with a particular individual. Unless this individual is an appropriate manifestation partner for the intervention, it will not be able to do its causal work. For example, antibiotics tend to treat infections, but only in interaction with a non-resistant bacterium and proper conditions for being absorbed by the patient’s body. Since most medical interventions have more than one disposition, a patient might be a non-responder to the targeted effect, but still a mutual manifestation partner for one or more of the non-targeted effects (see Edwards, Chap. 9, this book).
Simply put…
Mutual manifestation partners are a pair or set of dispositions that can do causal work in interaction with each other that they cannot do on their own.
Example: When a match is struck and lights, this is the manifestation of the flammable tip, the dry wood, the presence of oxygen, and so on.
When choosing a treatment for a particular patient, therefore, one should try to learn more about the dispositions of the patient who will be interacting with the treatment, as well as looking into the dispositions of the treatment. Most of the causally relevant dispositions in a treatment situation will actually come from the patient and their unique causal set-up, including medical history, genetics, diet, life situation and biography. This is why rich patient evidence is important, but it is also why it is important to understand causal mechanisms. Such mechanisms will tell us how the treatment works in the body, but also how the various dispositions of the patient might interact with the treatment.
How important is it for the clinic to have mechanistic evidence? Evidence based medicine and practice emphasise statistical evidence over mechanistic knowledge for establishing whether an intervention works. One argument for this is that our knowledge about pathophysiological mechanisms is at any time incomplete, and might be wrong. Because of this, some EBM proponents argue (Howick 2011), prediction about the effectiveness of an intervention should be based on population trials rather than on fallible mechanistic thinking. However, for the purpose of finding out how an intervention works, knowledge of causal mechanisms seems necessary. Russo and Williamson (2007) proposed what has been called the Russo-Williamson thesis. This thesis says that in order to establish causality, one needs both statistical evidence and evidence of mechanisms. Indeed, the correlations that are yielded from population studies are not necessarily causal.
Let’s take an example. Use of paracetamol is correlated to a higher incidence of asthma, but this association could be due to confounding by indication. This means that the onset of asthma could be due to frequent infections rather than to the concomitant use of paracetamol. In order to establish whether the correlation is causal or not, it is necessary to understand the mechanism by which the cause brings about the effect.
Russo and Williamson (2007) also argue that mechanistic knowledge is needed to plan the experimental design of clinical trials, as well as for the interpretation of the results from such studies. Rocca (2018) adds to these that knowledge of the causal mechanisms underlying medical phenomena is necessary to evaluate complex evidence, and to judge which population study we need to trust when different studies give conflicting results. Gillies (2018) argues that mechanistic knowledge is needed, not only to establish causal hypotheses about the cause of illness, but also to develop an appropriate treatment and for evaluating the safety of a treatment.
From a dispositionalist point of view, knowledge of causal mechanisms is crucial for understanding causality. On this perspective, the mechanism is a complex and contextual matter, and includes the types of dispositions that are involved in the causal process, how they interact, and also a potential for dispositions interfering with and altering the causal process.
Without any understanding of causal mechanisms, it is difficult to predict how a treatment will affect a particular patient and their unique set of dispositions. Statistical data from other patients might help reveal causal mechanisms, but there will always be causally relevant differences between individual patients that influence the outcome of an intervention. The more knowledge we have of the dispositions of an intervention (both beneficial and harmful) and of the patient (including vulnerability), the better our predictions will be for how the treatment will work for that patient. This is also why one always needs to know which other medications a patient is taking. While two of the drugs might be appropriate mutual manifestation partners for the desired outcome, there might be other drugs that interfere and alter that outcome. This brings us to the context-sensitivity of causality.
3.4 Causality Is Context-Sensitive
A cause will tend to produce different effects in different contexts, depending on what else it interacts with. We have seen that this is a problem for empiricism: in order to define C as the cause of a certain outcome, we need to observe the same outcome every time we have C. For Hume, if the outcome observed is different, then we cannot talk about the same cause. This is why it is hard to define causes outside of experimental isolation. However, the story changes if we think of a cause as an intrinsic disposition that might exist without being manifested, something we saw was unacceptable for Hume. The same disposition might tend to produce different effects. In fact, anything else should be surprising. How?
Because effects are produced, not by single dispositions but multiple, we cannot expect that the same causal intervention will always produce the same effect. Different contexts will give different effects, and we should not expect that two contexts are ever exactly the same. This is essential in the clinic. Assuming that all patients are different in at least some dispositions, each patient will represent a unique set-up of mutual manifestation partners for a treatment. One patient will therefore be a different mutual manifestation partner for the treatment than another patient. So even if the treatment works in the intended way in both patients, meaning that the treatment has the same disposition in both, the two patients might get different side effects, or the treatment might work with different strength or momentum in each of them. The outcome, or manifestation, of a disposition can thus be different in different contexts, but this does not mean that the disposition of the intervention (e.g. the drug) was different. This is why we urge that the same cause does not always give the same effect. By thinking this way we need some additional strategies for making claims about the disposition of the drug, other than Hume’s perfect regularity of cause and effect. For instance, we might know the drug’s disposition because we know how it works.
We can illustrate this point with an example of extreme context-sensitivity, where the same causal disposition tends to produce widely different effects in different contexts. Antiarrythmic drugs have the disposition to calm irregular heartbeat, by altering the electrophysiology of myocardial cells at a faster heart rate. Such alteration is obtained by inhibiting the fast sodium channels. This in turn prolongs the action potential refractory period in some of the myocardial tissues. This disposition is an intrinsic property of the antiarrythmic drug, and since we are aware of this property and how it works, we can say it is present also when it is not manifested. In some patients, the same types of drugs can on the contrary worsen irregular heartbeat, by inhibiting a different type of electric flow through the cell membrane, for instance by blocking potassium channels. In this case, the manifestation is different because of a different set up of mutual manifestation partners. However, we can still say that the disposition of the drug to block the sodium channel was present and the same. What is different is the way in which the disposition of the drug manifested itself in patients with different sets of dispositions. This is what it means to say that causality is context-sensitive from a dispositionalist approach.
Could we plausibly say that the same intervention amounts to the same treatment in two different patients, if one patient’s symptoms are alleviated while the other patient’s symptoms are aggravated? In the first case, the intervention produces the effect it was intended to produce. But in the second case, another effect happened. Was it a side effect of the drug? Or did the patient interfere with the drug, preventing the effect from happening? In this case, it seems more accurate to say that the two causal set-ups produced different effects because of the different mutual manifestation partners involved.
3.5 Modelling Causality
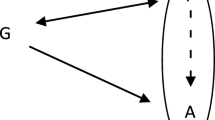
We can model causality in the single case using the vector model (Fig. 2.2). The model was developed in Mumford and Anjum (2011), adapted to the clinical scenario in Low (2017, see also Low, Chap. 8, this book) and later used by Price (see Price, Chap. 7, this book) to understand and manage the complexity of her chronic condition. In the vector model, the current situation is represented by a vertical line, on a quality space between two outcomes, F and G. In a patient with a chronic condition, such as irritable bowel syndrome, F might represent lack of gastrointestinal symptoms while G might represent continuous symptoms. Then we add the dispositions which are in place simultaneously and contribute to either of these outcomes as vectors. Vectors allow us to model two important features of dispositions: their degree of strength and their direction. Say, for instance, that for this patient consumption of fatty meals disposes toward gastrointestinal symptoms to a greater degree than salt or sugar. In that case, this should be reflected in the length of the vectors. One should not only include the dispositions that dispose toward the appearance of symptoms, of course, but also those that dispose away from them. The patient might experience less symptoms when he exercises regularly for instance, or after a good night of sleep. The resultant vector R thus shows whether the overall tendency disposes toward F or G, and how much.
An important feature of the vector model is the qualitative nature of the vectors. The length of the vector is not reflecting a numeric or statistical tendency, of how often the effect happens in a particular population. This means that the length of the vectors, as well as the type of disposition represented by the vectors, will vary from one individual to another. The reason for this is that the vector model should represent the singularism of causal dispositionalism: that causality happens in the unique particular context. While one person will tend to an impoverished gastrointestinal flora because of intensive pharmacological treatment, another person might not share this disposition, while still being overall disposed to irritable bowel syndrome. The length and direction of the vector should therefore be based on what is the case for a particular person at a particular time. One thing is that general scientific knowledge (generated by a plurality of evidence, including population studies) can be useful to suggest which causal disposition might be at play in the case of this particular patient: in general, we know that symptoms might be caused by the type of diet, emotional stress, etc. However, this general knowledge is not what the model represents.
Note that in Fig. 2.2, it is assumed that the different dispositions compose in a simple additive way, but this is not always or even usually the case. Some dispositions interact in nonlinear ways, and produce synergistic or antagonistic effects. This means that the total effect is greater than (synergistic) or smaller than (antagonistic) the sum of the individual factors. For example, knee pain can be improved or worsened by exercise, depending on the individual context, but also on the amount and type of exercise. We should therefore not expect exercise to be modelled with the same intensity or even direction in two different individual situations, or even for the same individual at two different moments in time. As physiotherapist Matthew Low (2018: 26) notes: ‘When evaluating the evidence, one must ask oneself, how does this study relate to my particular patient at this particular time?’. What is relevant for one patient might not be relevant for another.
The vector model, therefore, is a way to describe the quality of a causal situation, and not to measure and quantify it. Since we are used to thinking about vectors in connection with units of measure, it might take some time to get used to dropping such concerns in this case. But once this is left behind, it should become clear that the vector model allows us to illustrate some central features of causality: different types of causal interference, different degrees of tendency, threshold effects and tipping points, in addition to causal complexity and causal sensitivity. We will present these briefly, one by one.
3.6 Two Types of Causal Interference
The effect can be interfered with by removing a vector disposing toward the effect (subtractive interference) or by adding a vector disposing away from the effect (additive interference).
Suppose that in a patient, gastrointestinal symptoms can be counteracted subtractively (Fig. 2.3) by reducing the intake of alcohol, sugar or processed food. But one can also use additive interference (Fig. 2.4), such as probiotic supplements to enhance the gut microbiota complexity. Additive interference can be used when subtractive interference is not possible or sufficient to reduce the unwanted effect. Typically, all causal processes can be counteracted by adding something to the situation that tends away from the effect, at least in principle. In fact, most medical treatments are cases of additive interference, and even if an intervention has not been found for all health conditions, the default expectation is that we should keep looking for one.
3.7 Degree of Tendency
A disposition has a tendency towards its manifestation with a certain degree or intensity.
All dispositions come in various strengths (Fig. 2.5). For instance, oral contraception has a very strong disposition to prevention ovulation, but also a very weak disposition to produce thrombosis. So even though the correlation between oral contraception and thrombosis looks very weak, statistically, it still counts as causality because there is an intrinsic disposition in the pill toward thrombosis in combination with the appropriate manifestation partners. According to the dispositionalist theory, it is therefore no requirement that a cause produces its effect regularly or even ‘often enough’ in other similar circumstances, in order to count as causality. What counts is that there is something in the intervention that contributes to the outcome to a stronger or weaker degree.
3.8 Threshold Effects and Tipping Points
A threshold effect or tipping point is a stage in the causal process where something conspicuous happens that we might be particularly interested in bringing about or preventing.
The threshold effect (Fig. 2.6) is often a pragmatic and interest-relative matter, but it could also be the point at which a disposition manifests itself into something observable. In medicine and healthcare, a threshold effect might be the stage in the process of an illness where a problem or symptom occurs, such as fever, pain or anxiety attack. It could also represent a crucial stage toward recovery, such as in rehabilitation, where the goals or threshold might change along the way according to changes in the patient and their context.
Thresholds are useful because they can help show whether a situation is close to or far from a tipping point. One patient can be more vulnerable than another, if they are closer to the threshold for illness. In such a situation, a small change in the cause might result in a vast change in the effect. In cases of burnout or chronic fatigue, for instance, the trigger could have been something that might seem relatively harmless from a medical point of view. This could be a conflict at work, an infection or a life-changing event such as a divorce. What triggers an illness is thus not always the main cause of illness, but might simply be the ‘straw that broke the camel’s back’. In the vector model, one could then illustrate how a small change could have a big impact when the background conditions were already close to the threshold effect, although the same change would not make a difference for a person in a more robust stage of health (see also Price, Chap. 7, this book).
4 Philosophy of Causality Influences Scientific Methods
We have seen some main features of causal dispositionalism. This is primarily an ontological framework where causes are seen as dispositions. But how we think about a phenomenon will necessarily influence how we approach it. In this sense at least, ontology has an impact on practice. We will now see how ontological assumptions about the nature of causality influence even the scientific methods used for generating causal evidence.
In the CauseHealth project, we have argued that scientific methods are not philosophically neutral, but carry with them a number of assumptions about the nature of causality (Anjum and Mumford 2018b). How does this work? Let us look at some common methods and see how they attempt to establish causality, epistemologically. From this, we can see what type of features that causality needs to have, ontologically, in order for the method to be a reliable way to test for causality.
Epidemiological and other statistical methods use correlation data to search for causality. They also emphasise large amounts of data and proportion of outcomes. The idea is that more data will lead to more accurate causal conclusions. Ideally, one might think, if we had a complete set of correlation data — past, present, and future — one would also have complete causal knowledge. Philosophically speaking, this fits well with Hume’s regularity theory of causality and empiricist agenda. Further, causality is established by observing as many repetitions as possible, where the same cause is followed by the same effect. Some epidemiologists are sceptical of making causal claims based on their observations, and prefer instead to speak of correlations, raised probabilities or relative risk. This meets all the empiricist criteria for not saying something that goes beyond the available observation data and thereby avoiding inductive inference.
Other methods use comparisons of data to establish causality. Comparative methods allow us to search for causes by looking at the difference between two set-ups: one in which the cause is present (test) and a second in which it is absent (control). In randomised controlled trials (RCTs), if the outcome is more frequent in the test group than in the control group, one concludes that the increase is due to the intervention rather than the background conditions, which should be evenly distributed between the groups. The cause is then understood as a difference-maker, as suggested by Hume and Lewis (1973). Crucial for difference-making theory, is that the cause is something that can make a difference to the effect. If no difference can be observed, epistemologically, we have no reason to assume causality, ontologically.
Most scientific methodologies will rely on both regularity and difference-making. In a lab experiment, one compares what happens in the case of intervention with what happens without it, and usually with some repetition. Instead of randomisation of background conditions, these are carefully controlled for. By isolating the cause from interfering factors, one expects to better observe its causal role. Experimental methods also involve an assumption of manipulability, which is the assumption that a causal process can be manipulated in some way. This is crucial when we want to bring about or prevent a certain effect. By manipulating the cause, one also manipulates the effect. This is the basic idea of the interventionist theory of causality, with Woodward (2003) as its main proponent. Note that interventionist theory can be Humean or dispositionalist. If Humean, it would look for whether an intervention makes a difference. If dispositionalist, one would be more interested in the intrinsic properties of the intervention, its causal mechanisms and its influence across individual variations. This tension between statistical and individual effects is also seen in methodological approaches within psychology, as here discussed by psychologist Tobias Gustum Lindstad:
A prevailing idea among psychologists is that, in order to make psychotherapy evidence based, one has to prove the relevance of therapeutic models and the effects of specific techniques on a group-level. Thus, hundreds of perspectives, models and theories have been thrown into rivalry competing for the best mean results. However, this idea, that the only proper way to uncover the relevant causes is to observe their regular effects (the regularity view) threatens to throw the baby out with the bathwater. Since statistics does not take individual experiences into account, information about aspects that are relevant in each case are lost. Thus, one size does not necessarily fit all, and we must qualify our services locally and individually in any case.
Tobias Gustum Lindstad, ‘If statistics don’t get me, then what?’, CauseHealth blog (https://causehealthblog.wordpress.com/2016/02/05/if-statistics-dont-get-me-then-what/)
5 Practical Implications for the Clinic
In this chapter, we have given a brief overview of the dispositionalist theory of causality. We have explained how ontology – how we think the world is – influences epistemology – how we go about investigating the world. We saw that there are ontological assumptions about causality in all scientific methods. But what about clinical practice? What exactly are the practical and clinical implications of understanding causality in the dispositionalist way? We have already mentioned some ways in which dispositionalism might be used as a normative basis for clinical practice.
5.1 Causal Evidence Comes from the Patient
Emphasising causal singularism, mutual manifestation and interference, dispositionalism suggests that a major part of causal knowledge will rely on insights into the local context of a unique causal setup. In practice, this means that causal inquiry – both for understanding the condition and deciding how best to treat it – should begin from understanding the full complexity of the patient’s situation. This is because the patient will represent most of the causally relevant information needed to understand, diagnose or treat them. The patient’s context (the situation, the history, the narratives) is an indispensable source of medical evidence. This is not to say that general theory and population studies are of little use for clinical practice. Rather, local evidence about the patient context is needed in order to make sense of all the other types of evidence and theory available to the clinician. A practice that overlooks it is likely to end up being bad practice, even when it relies on good science and advanced technology. The question arising from this is how a clinician can get a better insight into aspects of the patient’s unique history and context that might influence their condition in positive or negative ways. One straightforward answer, which we heard from many of the clinicians we met during the project, is by listening to a patient’s narratives, and to the stories they have to tell. This is for instance what physiotherapist Neil Maltby has to say about the matter:
You’re history! Literally. What would you be without it? A void. It is impossible to change it. Your previous choice of job, degree, partner, hobby. Your exposure to family life, upbringing, culture, sports, arts, influential others. Even your genetic make up. Our histories intertwined with previous generation. It would be hard to look at these historical events without acknowledging their causal power in who you are now. What if I had been born into a richer/poorer family, the opposite gender, part of a majority/minority group? Would these not be causally relevant in who we become?
Say we randomly take 100 people off the street and show them the film Terminator. The situation is the same for each person. Same cinema, same time, same popcorn. Will they have the same reaction to the film? Of course not. Because history is more than just events. History is about people. People have dispositions. The best history for me is where people defy their circumstance. This is where we meet personal (or dispositional) attribution.
Dispositional attribution helps explain individual differences to the same stimulus or situation. This is not to say our situation has no impact on us. Clearly it does. It may help shape future dispositions. In life we lean on our internalised dispositions, feelings, previous experience. Two people (or even a single person with a time gap) may internalise the same situation in very different ways. This means we cannot rely on humans reacting robotically especially to complexity.
Is this even important?! Well I’d say so. It means as healthcare clinicians we are not striving for uniformity in treatment (situational attribution) because, as research shows, not everyone will respond to this. I think there is a lingering hope that one day we will come up with perfect protocols for lower back pain, fibromyalgia, tendon pain, irritable bowel syndrome and depression. This seems to be the aim in most research I read. Treatments based on pathology tend ultimately to look at situational attribution and not the dispositions of the individual.
Neil Maltby, ‘You’re history (hasta la vista, baby)’, CauseHealth blog (https://causehealthblog.wordpress.com/2016/02/19)
5.2 There Is No Standard or Average Patient
Assuming causal singularism and causal complexity, dispositionalism suggests that there might never be two identical causal situations in practice. All patients are in some sense medically unique, with different genetics, life situation and biography. In practice, this means that we should not expect that there is a ‘normal’, ‘ideal’ or ‘standard’ patient or even a normal response to a treatment. If something happens in one patient that cannot be backed up statistically or observed in other patients, this does not rule out the possibility of causality. Causal singularism means that all causal processes are intrinsic and particular. Effects happen in the single patient, as the result of multiple dispositions, many of which are unique to that patient. Physiotherapist and researcher Wenche Schrøder Bjorbækmo writes about standardisation:
At the end of the 1990s I perceived standardised testing and standardised procedures as the future. As a tester I became concerned with performing the tests correctly, which meant following the standardised procedures. The tasks I asked the children to do, and the questions I asked the parents were guided by the instructions and the structure of the test. It was important to remember the order of the tasks and questions. Several of the tests had many tasks and questions, and there wasn’t just one test to learn, but many. Each test had been adapted for different purposes and for different patient groups.
The test directs the professional view in particular directions, and thus away from anything else. When something in this way is brought into the foreground, other aspects, of for instance a child’s functioning, are disappearing into the background. In many ways this experience led me to think that in testing I was actually gaining less knowledge about the child and his or her functioning than in traditional clinical observations.
This experience of having ‘seen’ less and received less information frustrated and disturbed me. The test “demanded” a special form of communication and being together. I experienced the standardised framework of the test and administrative demands as framing the communication and relation made possible between the child, parents and myself.
Wenche Bjorbækmo, ‘Glasses and blind spots: through the eyes of a tester, CauseHealth blog (https://causehealthblog.wordpress.com/2017/11/20)
5.3 Unexpected Outcomes Are Valuable Causal Lessons
Dispositionalism stresses that all causal processes can be counteracted, subtractively or additively. So even when the effect typically follows from the cause, it is still possible to have the cause together with some interferer that is preventing the effect from happening. When this happens, one should aim to understand the dispositions involved and the causal mechanisms by which they interacted to produce or inhibit the effect.
This type of causal knowledge is particularly important for predicting how a patient will benefit from a treatment, or if there are any risks involved. While all treatments have a targeted effect that is tested and established, one can learn something important about the treatment’s other dispositions from their side effects. Side effects are often rare and unexpected, yet they point to dispositions in the patient that were able to causally interact with the drug. From this, we can develop new causal hypotheses for theory development, which are also relevant for basic research within medicine and biology (Rocca et al. 2019; Rocca et al. 2020). Ivor Ralph Edwards, medical doctor and senior medical advisor of the WHO collaborating Uppsala Monitoring Centre for International Drug Monitoring, has been dealing with the problem of detecting unexpected effects of pharmaceutical interventions for decades. In the following text, he explains why thinking of causes as dispositions can be useful in pharmacovigilance:
There is an ongoing debate about how to analyse and evaluate the data we gain from large data sets, and particularly what we can say about causality – after all, one is bound to find correlations by chance in vast amounts of data and with multiple analyses; but all this assumes that causality is a linear process which can be evaluated epidemiologically. Causality in real life, however, is usually multifactorial and complicated, and pharmacovigilance is concerned with data from complex healthcare systems in which multiple inter-relating factors evolve. The data we collect is affected by those changes over which we have no control….
One different approach to causality in pharmacovigilance is causal dispositionalism and is applicable to complex data. This approach considers the innate characteristics (the dispositions) of both the medicinal product and the exposed patient – some property, state, or condition that, under certain circumstances, gives the possibility of some further specific state or behaviour. The relevant properties of the medicines would include its various pharmacological actions (pharmacodynamics), its distribution in the body (pharmacokinetics), and its interactions with other drugs. The relevant properties of the patient would include specific susceptibilities, such as genetics, age, sex, physiological state such as body weight or pregnancy, co-morbidities, drug-drug interactions, and social and environmental factors that have affected the patient.
Consider a medication M, with a set of dispositions, M[d1], M[d2], and so on, known to be able to cause benefits and harm, and patient P with dispositions P[d1], P[d2], and so on. We may then begin to investigate the probabilities that any M[d] will produce beneficial or adverse outcomes in a patient with any P[d], asking the questions ‘how?’, and ‘when?’, using whatever information we have about the medicine M and the patient P to determine the benefit to harm balance. This type of analysis is not merely probabilistic, but also takes into account the strength – the power – of M to affect P, as well as any outside factor that interacts with the causal link, e.g. drug-drug interactions. It also explicitly takes into account the power of P to respond to M. A disposition may be present but not become manifest until its power reaches a particular threshold, e.g. above a certain dose of a medication, in combination with, for example, a certain degree of renal function impairment in the patient.
Alternatively, a medicine with disposition M[d4] may have maximal effects in patient P1 with dispositions P1[d2,3,4,5,6,7], partial effects in Patient P2 with dispositions P2[d2&7], and partial or maximum effects in other patients Pn with, say, dispositions Pn[d2,3,4,5,6,7,8,9], but only in certain environment where the two extra dispositions d8 and d9 result in an additional influence, such as might occur when syncope from a vasodilator only happens when a susceptible patient is dehydrated…
Let’s be very broad-minded about what new value we can find in the multiplicity of big real-life data sets we can utilise to examine benefit and risk and thereby improve therapy. (Edwards 2018: 28–29)
6 To Sum Up…
In this chapter we have argued that a genuine revision of the norms and practices in clinical work needs to start from a revision of the way we think about the world, and in particular the way we think about the most foundational concepts, such as causality. We have presented the dispositionalist theory of causality and explained why this theory is better suited for the clinic than the orthodox Humean theory which motivated the EBM framework. We have argued that causality ought to be understood as something singular and intrinsic rather than as a pattern of regularity across different contexts. From a dispositionalist perspective, causal knowledge ought to start from the single case. In the clinic, this means that the more we know about the multiple dispositions that are involved and how they interact in this specific context, the better equipped we will be to make good and relevant explanations, predictions and decisions for the individual seeking care.
References and Further Readings
Anjum RL, Mumford S (2017) Emergence and demergence. In: Paoletti M, Orilia F (eds) Philosophical and scientific perspectives on downward causation. Routledge, London, pp 92–109
Anjum RL, Mumford S (2018a) What tends to be. The philosophy of dispositional modality. Routledge, London
Anjum RL, Mumford S (2018b) Causation in science and the methods of scientific discovery. Oxford University Press, Oxford
Cartwright N (1989) Nature’s capacities and their measurements. Oxford University Press, Oxford
Edwards R (2018) Living with complexity and big data. Uppsala Rep 78:28–29
Gillies D (2018) Causality, probability, and medicine. Routledge, London
Howick J (2011) Exposing the vanities – and a qualified defense – of mechanistic reasoning in health care decision making. Philos Sci 78:926–940
Hume D (1739) A treatise of human nature. In: Selby-Bigge LA (ed) Clarendon Press, Oxford, 1888
Lewis D (1973) Causation. In: Lewis D (ed) Philosophical papers ii. Oxford University Press, Oxford 1986:159–213
Low M (2017) A novel clinical framework: the use of dispositions in clinical practice. A person centred approach. J Eval Clin Pract 23:1062–1070
Low M (2018) Managing complexity in musculoskeletal conditions: reflections from a physiotherapist. In Touch 164:22–28
Martin CB (2008) The mind in nature. Oxford University Press, Oxford
Mumford S (1998) Dispositions. Oxford University Press, Oxford
Mumford S (2004) Laws in nature. Routledge, London
Mumford S, Anjum RL (2010) A powerful theory of causation. In: Marmodoro A (ed) The metaphysics of powers: their grounding and their manifestations. Routledge, London, pp 143–159
Mumford S, Anjum RL (2011) Getting causes from powers. Oxford University Press, Oxford
Rocca E (2018) The judgements that evidence based medicine adopts. J Eval Clin Pract 24:1184–1190
Rocca E, Copeland S, Edwards IR (2019) Pharmacovigilance as scientific discovery: an argument for trans-disciplinarity. Drug Saf 42:1115–1124
Rocca E, Anjum RL, Mumford S (2020) Causal insights from failure. Post-marketing risk assessment of drugs as a way to uncover causal mechanisms. In: La Caze A, Osimani B (eds) Uncertainty in pharmacology: epistemology, methods and decisions, Boston series for the history and philosophy of science, Springer, Dordrecht
Russo F, Williamson J (2007) Interpreting causality in the health sciences. Int Stud Philos Sci 21:157–170
Woodward J (2003) Making things happen: a theory of causal explanation. Oxford University Press, Oxford
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2020 The Author(s)
About this chapter
Cite this chapter
Anjum, R.L. (2020). Dispositions and the Unique Patient. In: Anjum, R.L., Copeland, S., Rocca, E. (eds) Rethinking Causality, Complexity and Evidence for the Unique Patient. Springer, Cham. https://doi.org/10.1007/978-3-030-41239-5_2
Download citation
DOI: https://doi.org/10.1007/978-3-030-41239-5_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-41238-8
Online ISBN: 978-3-030-41239-5
eBook Packages: Religion and PhilosophyPhilosophy and Religion (R0)