Abstract
In this chapter, physiotherapist Roger Kerry explores the relationship between the principles of causal dispositionalism, presented in the first part of this book, and the practice of evidence based healthcare (EBHC) (previously evidence based medicine). EBHC is structured around a framework which, although alluding to the integration of multiple sources of evidence, firmly prioritises data from well-controlled population studies in both clinical and policy decision making, as we saw in Part I. In doing so, EBHC deemphasises the role of ‘lower quality’ information sources, such as observational studies, laboratory studies, clinical experience, etc. The rationale for such prioritisation lies in the way that the evidence based framework conceptualises causation. By examining the EBHC evidence hierarchy, a clear neo-Humean notion of causation is evident at the heart of EBHC. In the CauseHealth project, neo-Humeanism is seen as problematic for clinical practice and dispositionalism offers a causal theory which takes real-world complexity and context-sensitivity as its starting point. Can a new practice framework be offered which is based on evidence, yet underpinned by a dispositional ontology? If so, how would this look?
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
1 Complexity in Practice
When I was a young Junior Physiotherapist, a department I worked for was chosen as a centre to collect data for one of the first multi-centred low back pain trials in the UK. My job was to identify any of my low back pain patients to see if they could be included in the trial. I was keen to be involved, as I was very curious about what might work for people with low back pain. People with low back pain typically struggle to respond well to many interventions, hence the global epidemic status of non-specific low back pain. I was surprised (naively) that the trial criteria excluded people with co-morbidities, poor general health status, and repeated previous treatments – this would be most of my patients. When I had the chance to discuss this with the visiting trial co-investigator, he explained that they were trying to get the conditions of the trial as controlled as possible so that they could get a “good, clear view” of what worked for people with low back pain. The identification of causal associations between two variables is of course the scientific ideal. The removal and control of possible confounders is a hallmark of high-quality health research. Yet this is not what my patients looked like. What was the impact of their co-morbidities? How did their general health affect their painful experience? What were the biological and psychological consequences of repeated previous treatment? It was clear that the trial conditions were not representative of the complex and context-sensitive clinical shop-floor.
My interest in the CauseHealth project stems primarily from questions raised on the shop-floor of clinical healthcare – and specifically physiotherapy. As a clinician, teacher, and researcher in physiotherapy, there has been one question in particular, which I first began thinking about many years ago during the emergence of evidence based healthcare in the early 1990s when I was training as a physiotherapist.
-
Is the sort of causation we establish in population research studies the same sort of causation we are seeking with an individual patient?
Witnessing contradictory results on the shop-floor – for example, a patient not responding to a strongly ‘evidence based’ intervention – is not uncommon and can easily be passed off by considering that person as a “non-responder”. However, is this always the case? Or is there something about the individual context which is not readily represented in population studies? If so, what are the fundamental assumptions about causation in both clinical practice and scientific, systematic research? With all this in mind, my philosophical interest in causation began, and my relationship with CauseHealth was soon cemented.
Causation lies at the heart of healthcare. This is clearly manifest in aspects of healthcare such as causes of disease, but of course it is also the core focus of research methods which try to establish the therapeutic effectiveness of health interventions: what causes someone to get better. Such research methods represent a central feature of the practice framework of evidence based healthcare (EBHC) – that is the proposal that all healthcare practice and decision making should be based on the best available evidence. This evidence is multi-factorial and can in principle emerge from a number of sources, such as systematic clinical research, laboratory research, clinical observations, experience, and so on. The most recent formal iterations of EBHC stems from literature regarding evidence based medicine in the early 1990s (Guyatt 1991; Guyatt et al. 1992; Sackett et al. 1996). This literature sets out specific and detailed structures by which different evidential sources are given different priorities and is still explicitly reflected in the most contemporary re-workings of EBHC, for example the GRADE framework (Mercuri and Baigrie 2018; Guyatt et al. 2011). Philosophically, this is a critical feature of EBHC, as it allows us to understand some fundamental assumptions on which clinical decision making is based. If certain evidential sources are given priority over others, we have an insight into the epistemological and ontological groundings of what we do as healthcare professionals, in both practice and research.
In this chapter I therefore summarise an early and central idea from the CauseHealth project, which served to motivate much of the direction of thought and research within the project. That idea was that the way in which EBHC prioritises its evidential sources demonstrates that the underpinning causal theory of healthcare is essentially Humean (Kerry et al. 2012). To problematise this, we sought to consider what the limitations of practicing healthcare were if a strict Humean notion of causation was assumed. In doing so, it became clear that perhaps what the evidential structuring of EBHC meant by causation was not necessarily the sort of causation which is at play in real-life, complex healthcare decision making. As such, we offered an alternative causal theory, based on dispositionalism. This theory could better account for both the scientific processes (methods) used to establish data from populations, and the context-sensitive, complex mass of information witnessed in individual clinical encounters. Where Hume saw causes as nothing more than regularly occurring events with certain temporal and spatial relationships, while Hume’s opponents argue that, in addition, causes necessitate their effect, we take causes as real features of the world which interact with each other and have only a tendency to manifest in an effect (Kerry et al. 2012). Dispositionalism, I will argue, offers a more real-world account of causation.
2 Evidential Hierarchies Expose Causal Theory
During my formative years as a physiotherapist, I was schooled in the ways of best practice and the limitations created by our human biases. I would often be the first to dismiss any enthusiasm which other ‘lesser’ colleagues might experience when patients responded well to our interventions: for example, a patient claiming they had a huge reduction in pain after some hands-on therapy. My responses would always be along the lines of “you don’t know that it was the treatment that made the difference”, or “there is no RCT-level evidence to support that”, and “you have to be aware of your own perception biases”, and so on.
But what if that patient had been a subject as part of a trial? What if the trial protocol was just the same as what had happened in clinic that day? The improvement seen would then be recorded and added to data from other similar subjects, and then compared to data from subjects who had a different intervention, or whatever. That response would then be considered positive and causally associated to the intervention. But this causal claim would not be made on what had been observed that day, but rather what had happened to other subjects.
This counterfactual reasoning is again part of the essence of our research structures. However, dispositionalism would suggest that the causal process was always a real feature of what happened in that individual case. Can the clinician be their own scientific data collector, ensuring critical analysis, reflection, and a systematic approach to patient care, and in doing so observe real causation? A dispositionalists account of causation would permit this. The reaction from EBHC is that you cannot make generalised claims from such individual observations. We would agree. Dispositionalism takes all causal cases as context-sensitive, so what works in one context is not what would work in another one.
I will now demonstrate how a Humean notion of causation can be read from evidential hierarchies. I explain some of the problems with this and present four key desideratum to highlight how the dispositionalist alternative can address the short-falls of Hume’s approach to causation.
If we take the inaugural papers of Guyatt, Sackett et al. (as above) as the onset of the contemporary working of evidence based healthcare (originally referred to as evidence based medicine), the structuring of evidential sources is clear. Essentially, research methods with a low risk of bias for confounding are given evidential priority. Randomised controlled trials (RCTs) are considered a gold standard method as they are able to control for both known and unknown confounding variables. In doing so they, ideally, isolate the hypothesised causal variables from other possible causes and observe the effect in repeated conditions (large samples, repeated studies, etc.). The data from such trials is then sought, to be synthesised and presented in systematic reviews, which sit at the top of accepted evidential hierarchies. Methods with increasing risk of bias are progressively de-emphasised down the hierarchy. This is in line with what La Caze (2008) refers to as a categorical reading of evidential hierarchies. High quality RCTs and low risk observational studies thus provide confidence in causal claims, whereas de-emphasised sources do not. This structuring is honourable and adheres to fundamental principles of science. It also gives a direct indication of the causal assumptions which healthcare works on.
Consideration of the characteristic differences between ‘causal methods’ (RCTs etc.) and ‘non-causal methods’ (case studies, mechanistic studies, experience, etc.) provides a starting point here. What defines these causal methods is the fact that they first systematically observe the relationship between two events (say, A and B) multiple times whilst controlling for possible confounding, and then, facilitated by statistical modelling based on a frequentist idea of probability (see Rocca, ch. 3, this book), make a judgment on whether causation exists, i.e. whether the intervention (A) causes a desired health improvement (B). The difference between RCTs and observational studies is that the observations within RCTs are then compared to observations in another group which does not include the variable of interest (i.e. A). The de-emphasised methods and evidential sources do not possess these features.
With these characteristics in mind, it is now possible to analyse these processes a little further in order to draw out what ontological background these methods, and the associated causal claims, operate on.
Even with a superficial reading, it is clear to see a Humean essence to the causal ontology: Hume allowed that causation could be wholly represented in fact by adherence to three criteria; temporal priority, contiguity, and constant conjunction:
… we may define a cause to be an object, followed by another, and where all the objects similar to the first are followed by objects similar to the second. (Hume 1748 EUH 7.1.60)
Further,
Every object like the cause, produces always some object like the effect. Beyond these three circumstances of contiguity, priority, and constant conjunction, I can discover nothing in the cause. (Hume 1740: A 9)
So, the cause always precedes the effect (A precedes B in time), the effect is consistently close to the cause (A and B are spatiotemporally contiguous), and the association is repeatedly and constantly observed (events like A are invariably followed by events like B). We can thus claim causation in a Humean sense (A causes B). This is a regularities view of causation, which is typically Humean and satisfies many tenets of conventional scientific principles.
This analysis can now take a short step further if RCTs are considered separately. If we assume that the characteristic difference between RCTs and observational studies is in essence the presence of a comparative group (current treatment, control, placebo), then there is a further aspect of the causal theory which can be considered in a Humean sense. This is the impact of counterfactual dependency, and also identifying the truthmaker of causation.
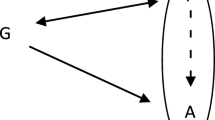
The fundamental set-up of RCTs is represented in Fig. 13.1. This illustrates a typical, simple comparative study. The left-hand group is the intervention group (A). The right hand is the counterfactual (¬A), which is the control in which not-A. In the intervention group a level of outcome is observed, B(x). In the counterfactual control group, outcome B(y) is obtained. The Randomisation and Allocation stages provide the strict counterfactual conditions. If the truthmaker was the counterfactual, then causation is B(x) – B(y). This satisfies that A➔B. Without y, and therefore without the control ¬A, there could be no claim to causation.
So, a comparative group can be thought of as a counterfactual condition. This is a condition wherein the variable of interest (the therapeutic intervention under investigation) does not exist but where as much as possible otherwise remains the same. Neo-Humean philosophers refer to this as the closest possible world (Lewis 1973). In RCTs, the counterfactual acts as the truthmaker to causation. Here’s how: let’s say that in Group 1 (intervention), 62% of all participants achieved a positive outcome. If this were an observational, uncontrolled study, all we could say is that there is some sort of correlation, to the magnitude of 62%, between the variable A and variable B. We would not be confident in drawing causal claims from that because other variables (confounders) could in fact be the cause of B. So, another group is set up which does not include A (the counterfactual), and if there was a similar response rate, we might logically say that the cause of the 62% positive responses was not because of A. Alternatively, if there was a much lower response rate in the counterfactual group, for instance 30%, we might (using statistical methods) say that the difference is sufficiently significant such that we are confident that A was the cause of B, because not half as many participants in Group 2 achieved a positive response to the intervention.
In either of these scenarios, the element of the methodological make-up which gave us confidence in inferring causation from Group 1 was not in fact what happened in Group 1, but rather what happened in Group 2, the counterfactual. It wasn’t until we observed the response rate in the counterfactual group that we were confident to read causation into what happened in Group 1; thus Group 2, the counterfactual, is taken as the real truthmaker of causation. This is in line with the Humean conception of causation, which also has this counterfactual element:
Or in other words where, if the first object had not been, the second never had existed. (Hume 1748 EUH 7.1.60)
We now have two distinctly Humean aspects of causation identified within the hierarchies of evidence for EBHC: a regularities view, and counterfactual dependency.
To complete the Humean picture, note that because causation is drawn from regularly occurring patterns of events and/or counterfactual conditions, any allusion to an actual substance or matter of causation is absent. That is, the processes or mechanisms of how and why A causes B is missing, or at least considered unnecessary on this causal account. Indeed, Hume said as much:
Every object like the cause, produces always some object like the effect. Beyond these three circumstances of contiguity, priority, and constant conjunction, I can discover nothing in the cause. (Hume 1740: A 9)
and,
The impulse of one billiard-ball is attended with motion in the second. This is the whole that appears to the outward senses. The mind feels no sentiment or inward impression from this succession of objects: consequently, there is not, in any single, particular instance of cause and effect, any thing [sic] which can suggest the idea of power or necessary connexion [emphasis added] (Hume 1748 EUH 7.1.50)
In summary, Hume considered causation to be nothing more than observed regularity, supported by observations of the effect not happening in the absence of the cause and irrespective of there being some explanatory mechanism for the events.
This account visibly underpins the desired evidential hierarchies supported by EBHC. We see this as problematic for a discipline which is characterised by complexity and context-sensitivity, as person centred healthcare might be (Miles and Mezzich 2011, 2012).
3 A Dispositionalist Response
I will now outline a dispositionalist’s response to the emergent problems of a Humean account of causation. I will do this in a framework of four desideratum which have been developed from existing commentary on how a causal account for healthcare should look. In order for a causal account for healthcare to be valid, it should:
-
1.
explain the causal role of content from particular research methods;
-
2.
motivate a viable epistemology;
-
3.
account for causal processes in individual level clinical decision making;
-
4.
help understand and assess additional premises and assumptions needed to bridge the inferential gap between population level evidence and clinical decisions.
These can now be taken in turn, with brief attention to the limitations of Humeanism, and an alternative dispositionalist response.
3.1 Explain the Causal Role of Content from Particular Research Methods
For the clinician, this simply means that a research theory which we draw causal claims from (i.e. “does exercise work?”) should be able to satisfactorily explain how and why the data from particular methods relates to such claims. Our examples throughout this chapter have been about data from RCTs, and we have seen that the statistical outcomes of RCTs tell us something about the differences between groups, but they do not meaningfully give us an insight into the real causal explanations of that difference. We suggest that a dispositionalist reading of scientific data better explains how it relates to causation.
A traditional Humean account of causation offers some explanation as to how causal claims are developed from research methods relying on statistical data and comparisons of these. Humeans are able to discuss causal claims in terms of either frequencies of occurrence of events, or the degree of differences between two frequencies, or both. Proponents of the Humean account are satisfied that this sufficiently explains the causal role of research content, specifically highlighting that this avoids unnecessary matters of ontology. The dispositionalist response is straightforward: the content that is being referred to here is not of causation, but of something else. The essence of causation has not been reached, and as such any explanation related to causation cannot be given. The truthmaker of causation within Humean accounts is too far removed from where causation itself is most likely to be found.
What dispositionalism offers is a view that sees causation within the core of the content itself: the properties involved in the causal process. Changes are seen within groups, and these changes occur as a result of the interactions of multiple dispositions tending towards and away from effects. Whereas Humeans consider single causes by proxy of frequently occurring observed events, dispositionalists see various causal factors that may or may not manifest in an effect. The causal role of these events for dispositionalism is the notion of how they manifest and how they may tend towards and away from anticipated thresholds. Dispositionalists are unsatisfied with causal explanations that relate to frequentist interpretations of probability, as probability should be thought of in relation to the propensities held by causal factors (see Rocca, ch. 2, this book). (For those who are interested, Donald Gillies (2017) provides a useful primer on the different interpretations of probability on healthcare.) The response here has allowed some appreciation of the way causal content from research methods might be thought of in relation to different ideas about causation.
3.2 Motivate a Viable Epistemology
Epistemology basically means ‘theory of knowledge’ and allows us to judge on what grounds our beliefs and opinions are made. So when we say “exercise works for low back pain”, we can satisfactorily answer how we know this. In healthcare, we want our beliefs and opinions to be as close to the ‘truth’ as possible. Therefore, any underpinning theory for research and practice must be able provide and encourage an epistemology which any logical, scientifically-minded practitioner could be comfortable with using to justify their beliefs and opinions. We see that there are limitations to a Humean-motivated epistemology which dispositionalism can respond to.
The motivation for a viable and pluralistic epistemology comes from the dispositionalists’ commitment to an ontology of the reality of causes, and the understanding that those causes are the most basic and fundamental features of the world. Although others have spoken about multiple methods, (for example, Williamson 2007 and Howick’s views on mechanisms in Howick et al. 2013), they struggle to conclude with a convincing epistemology due to their Humean commitments. Framed by epistemological matters, these attempts have been instances of identifying the problems of a traditional monistic account, but trying to resolve these with either pluralistic accounts, or epistemologically driven theories. This is unsatisfactory on two counts: one that there is confusion and conflict between competing theories of causation; and two that in refusing to commit to an ontology of causation, it is not even possible to identify what the methods are searching for.
A theory of dispositions has clearly defined what causation is, and is confident that a methodological pluralistic framework, whereby all methods point to the same thing, offers a satisfactory account of its causal epistemology. A common element in the dispositionalist response across these two desiderata has been the primacy of causation in a dispositions account. Causes are assumed as fundamental and real features of the world with dispositions.
That causes are primitive and real has allowed commentary on both how causal content of methods can be explained, and how a viable epistemology can be motivated. Humeans struggle with explaining causal content because they admit to causation being nothing more than accidental regularity, represented through a frequentist interpretation of probability. Dispositionalists on the other hand take causes as real entities and so can describe and explain precisely their content. As causes can only ever tend towards an effect, dispositionalism does not have to represent causes through frequencies. Rather, a probabilistic theory based on individual propensities offers deeper explanation of the causal content.
Dispositionalism is confident that its visible ontology prepares the ground well for talking about and accounting for a reconceptualised causal epistemology. Its reference to methods such as RCTs being symptomatic rather than constitutive of causation facilitates a methodological pluralist stance whereby information from multiple methods and sources may reveal parts of the causal process. These sources can include indicators of causation such as mechanistic science and patient narratives. Dispositionalists do not need to worry about the reconciliation of multiple theories of causation, because causes are only one thing.
3.3 Account for Causal Processes in Individual Level Clinical Decision Making
This is the key issue in science and practice – the problem of induction: how do claims made at a population level relate to individual clinical decision making? Do the outcomes of an RCT relate directly to your patient in front of you? And if so, how do you account for and explain that relationship? A satisfactory theory of causation and research must be able to do just that.
As physiotherapists, we have guidelines which recommend (based on RCT level evidence) that exercise should be considered as an effective intervention for people with lower back pain (LBP) (NICE 2016). This is encouraging on many levels, as there can be many possible co-benefits to exercising, such as improved general fitness and cardio-vascular health. However, a particular patient may have a dispositional make-up which either inhibits them from doing exercise (desire, time, capacity, co-pathologies, etc.), or indeed which tend to make the pain worse during exercise (fear, anxiety, previous experience with exercise, inappropriate loading, etc.). Thus, the person with low back pain is not seen as a discrete and independent variable onto which ‘exercise’ can be put on to. Rather, this person becomes part of a causal process within which the many dispositional traits of both themselves and the undertaking of exercise can be sculpted together to work towards a therapeutically beneficial response to exercise, such as addressing anxieties and fears, coaching on appropriate loading, developing capacity, and so on.
Dispositionalism is a singularist view (Mumford and Anjum 2011: 71–2), and takes particular causal claims and singular instances to be where causation lies (see Anjum, ch. 2, this book). However, the dispositionalist ontology moves quickly beyond a world of discrete events. The relata for causal relations are not discrete events or facts – for example, event C (exercise) and event E (improvement LBP) – but the powers and properties of things – for example, the disposition of exercise and the disposition of a patient with LBP.
At the same time, however, dispositionalism sees general claims as having a role to play in a theory of causation, especially when particular circumstances are not yet known. General claims allow us to be “armed for future actions” (Mumford 2009: 14). However, the truth of any general causal claim is substantiated by the properties or dispositions of such claims, and not associations of discrete events and the statistical facts that relate to such. The particular instance, however, that is able to stand separate from a general claim, allows further insight into what causation is.
If causal relata are the properties of things, then immediately there is a glimpse of the essence of what causation might be. Causation is now something primitive. That is, it is not something that can be analytically reduced to something else, such as non-causal facts about (repeated) observed associations between events, a difference-maker or a raised statistical probability. Particular instances provide a notion that the modality of a dispositionalist account is neither one of contingency (that is, the probability or possibility of an effect happening), nor of necessity (that the effect will (or will not) happen). What dispositions can say about a particular instance is that there is a modality of tendency that is unique – a sui generis (Anjum and Mumford 2018). A cause is something that tends towards its effect in a way that cannot be reduced to accidental regularity or necessity.
3.4 Help Understand and Assess Additional Premises and Assumptions Needed to Bridge the Inferential Gap Between Population Level Evidence and Clinical Decisions
This point continues to work on the challenge of the “inferential gap”. The traditional Humean theory of EBHC can only take things so far and bases its assumptions to cross the gap between general and particular claims on the quality of the research method and frequentist probability. Both are problematic assumptions which are abstract to the world of clinical practice.
Causes are clearly not to be understood as factors that have exactly the same effect in every context in which they appear. Causes that have been identified through RCTs, carried out to perfectly acceptable standards, and clearly suggestive of a certain prediction and clinical intervention, could nevertheless fail to produce their expected effect. When one looks to the ontological matters of causation, one sees that this further consideration, concerning context and composition, can be highly significant. Adding together a combination of drugs, for instance, each of which has been found to have a safe and positive effect in RCTs, could still possibly produce a ‘cocktail effect’ that is unsafe. Again, this explains why causal inferences are fallible. They are based on an assumption of a finite number of operating factors. An unknown factor could effectively be an additive interferer, for some expected effect. Worse still, it might be a factor that composes nonlinearly with the presence of the other factors to produce an antipathetic effect.
The predictive value of such dispositional reasoning might, however, be questioned by those schooled in (probabilistic) deductive necessity – at least robust methods might have some predictive utility within a traditional account, it might be claimed. However, dispositionalism is not relativism and prediction is a feature of dispositionalism. It is not that dispositionalism denies deductivism, although it does judge it to be “over-ambitious” (Mumford and Anjum 2011: 140). The difference is subtle but clear: whereas the traditionalist would say ‘if A, then necessarily B (to a degree of probability)’, the dispositionalist would say ‘if A, then B is disposed or tends to happen’.
The Humean response is simply to assert that if prioritised methods are conducted correctly – without experimental error – then predictions should be forthcoming that are simple, exact and unfailing. We know this to be false. Any account of causal inferences has to respect the obvious datum that predictions are fallible and defeasible. Dispositionalism offers an explanation of prediction and inference within a fallibilist framework in which dispositions tend to produce their effects but might not always do so.
4 Conclusion
We often use interventions with our patients which are based on the best of evidence, yet still see no positive response. The Humean might see this as a normal artefact of frequentist reasoning – on average the intervention works, bad luck in this case. The dispositionalist, however, sees it as an example whereby there are insufficient additive causal factors, or too many subtractive factors than desired and so a therapeutic threshold is not reached. The “intervention” is just one possible causal factor, and its success relies on its manifestation with other causal partners. This is what is characteristic about complex and context-sensitive clinical practice. Neither the intervention nor the patient has ‘failed’, rather, there has not been the anticipated mutual manifestation of variables in this case. Multi-dimensional clinical reasoning frameworks, such as Mitchell et al. (2017), are exemplars of a dispositionalist theory at play. The constantly evolving understanding of how aspects of a person’s biological, psychological, social dimension of their life and experience may dispose them towards either an improvement, or a worsening of their health status.
In this chapter, we have learnt something about the relationship between EBHC and causation, and also between theory and methods. Less-than-perfect correlations can indicate something causal occurring, but are by no means irrefutable evidence of some consistent or generalisable causal trend, however strong the correlation. Prioritised research methods can indicate causal processes. However, the causal work is being done within each group and thus it is the groups themselves, not the regularities or counterfactuals, which act as the truthmakers. Robust population studies may be very good at displaying symptoms of causation, but they are not constitutive of causation.
The greatest causal work can be seen in single instance cases. This is where the real nature of causation is witnessed. The interaction between causal agents, subtractive and additive dispositions tending towards and away from an effect, causal powers being passed from one partner to another. For the dispositionalist, the essence of causation becomes apparent. In a dispositionalist ontology, scientific research should focus on the interaction of causal partners and not be dominated singularly by the pursuit for statistical invariance in large groups. For the clinician, the relationship between research findings and individual clinical decisions becomes clearer.
Despite those who reject the utility of anything other than epistemological analyses, an ontological review allows the notion of EBHC to be re-evaluated from bottom-up. One of the foundational intentions of this chapter was to work towards a philosophical underpinning of EBHC that would better support what already happens in clinical practice. This bottom-up approach relates well to clinical practice. Least of all because a dispositionalist account of causation takes the individual patient and the therapeutic interaction, along with all that is known about the process of disease and interventions, as its starting point for an account of causation.
The ontological locus of dispositionalism allows the theory to escape commitments to – and therefore shortcomings of – proxy truthmakers, universal laws, causal necessity, probabilistic inference, and restrictive logical forms. A causal theory based on causal dispositionalism is well positioned to account for the problems represented by the claims of EBHC, and furthermore provides an appealing commentary on a causal epistemological framework. For the shop-floor clinician, a dispositional ontology for causation far better facilitates a person-centred, evidence-informed clinical reasoning approach to best healthcare practice. If this were the only legacy of the CauseHealth project, then it has been a worthy venture.
References and Further Readings
Anjum RL, Mumford S (2018) What tends to be; the philosophy of dispositional modality. Routledge, London
Gillies D (2017) Frequency and propensity: the interpretation of probability in causal models for medicine. In: Solomon M, Simon JR, Kincaid H (eds) The Routledge companion of philosophy of medicine. Routledge, London, pp 71–81
Guyatt G (1991) Evidence-based medicine. ACP J Club 114. https://doi.org/10.7326/ACPJC-1991-114-2-A16
Guyatt G, Cairns JA, Churchill D et al (1992) Evidence-based medicine. A new approach to teaching the practice of medicine. JAMA 268:2420–2425
Guyatt G, Oxman AD, Akl EA, Kunz R et al (2011) GRADE guidelines: 1. introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 64:383–394
Howick J, Glasziou P, Aronson JK (2013) Problems with using mechanisms to solve the problem of extrapolation. Theor Med Bioeth 34:275–291
Hume D (1740) Abstract of a treatise of human nature. In: Millican P (ed) An enquiry concerning human understanding. Oxford University Press, Oxford, pp 133–145
Hume D (1748) An enquiry concerning human understanding. Oxford University Press, Oxford
Kerry R, Eriksen TE, Lie SAN, Mumford SD, Anjum RL (2012) Causation and evidence-based practice: an ontological review. J Eval Clin Pract 18:1006–1012
La Caze A (2008) Evidence-based medicine can’t be…. Soc Epistemol 22:353–370
Lewis D (1973) Counterfactuals. Oxford University Press, Oxford
Mercuri M, Baigrie BS (2018) What confidence should we have in GRADE? J Eval Clin Pract 24:1240–1246
Miles A, Mezzich JE (2011) Person-centred medicine: advancing methods, promoting implementation. Int J Pers Cent Med 1:423–428
Miles A, Mezzich JE (2012) The care of the patient and the soul of the clinic: person-centered medicine as an emergent model of clinical practice. Int J Pers Cent Med 1:207–222
Mitchell T, Beales D, Slater H, O’Sullivan P (eds) (2017) Multi-dimensional clinical reasoning framework. Curtin University Press, Curtin. https://www.musculoskeletalframework.net/
Mumford SD (2009) Causal powers and capacities. In: Beebee H, Hitchcock C, Menzies P (eds) The Oxford handbook of causation. Oxford University Press, Oxford
Mumford S, Anjum RL (2011) Getting causes from powers. Oxford University Press, Oxford
NICE (2016) Low back pain and sciatica in over 16s: Assessment and management. Nice Guideline [ng59]
Sackett DL, Rosenberg WMC, Gray JAM, Haynes RB, Richardson WS (1996) Evidence based medicine: what it is and what it isn’t – it’s about integrating individual clinical expertise and the best external evidence. Brit Med J 312:71–72
Williamson J (2007) Causal pluralism versus epistemic causality. Philos Mag 77:69–96
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2020 The Author(s)
About this chapter
Cite this chapter
Kerry, R. (2020). Causal Dispositionalism and Evidence Based Healthcare. In: Anjum, R.L., Copeland, S., Rocca, E. (eds) Rethinking Causality, Complexity and Evidence for the Unique Patient. Springer, Cham. https://doi.org/10.1007/978-3-030-41239-5_13
Download citation
DOI: https://doi.org/10.1007/978-3-030-41239-5_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-41238-8
Online ISBN: 978-3-030-41239-5
eBook Packages: Religion and PhilosophyPhilosophy and Religion (R0)