Abstract
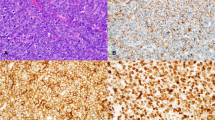
Among all mature B-cell neoplasms, the group of small B-cell lymphomas with or without plasmacytic differentiation encompasses several subtypes in which the neoplastic cells constitute a clonal population of predominantly small lymphocytes. Depending on the specific subtype, these lymphomas may show varying degrees of plasmacytic differentiation. Each subtype in this group is characterized by distinct clinical, morphologic, immunophenotypic, and genetic features which are important for precise diagnosis and classification. The majority of these lymphomas are lymph node based; however, extranodal sites such as bone marrow, peripheral blood, and spleen are frequently involved. Precise classification is crucial given their distinct clinical behavior. For example, mantle cell lymphoma is an aggressive disease that often requires therapy, whereas patients with other small B-cell lymphoma subtypes generally have an indolent clinical course and may survive for many years without therapy. With recent advances in molecular genetics, new knowledge about the biology of these diseases has contributed to the development of more refined diagnostic, prognostic, and therapeutic schemes, many of which have been incorporated in the 2017 revised 4th edition of the World Health Organization’s (WHO) classification of hematopoietic tumors. This chapter will focus on the common small mature B-cell lymphomas providing a practical approach for diagnosis and classification.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Wang HY, Zu Y. Diagnostic algorithm of common mature B-cell lymphomas by immunohistochemistry. Arch Pathol Lab Med. 2017;141(9):1236–46.
Jaso JM, Yin CC, Wang SA, Miranda RN, Jabcuga CE, Chen L, et al. Clinicopathologic features of CD5-positive nodal marginal zone lymphoma. Am J Clin Pathol. 2013;140(5):693–700.
Gimeno E, Salido M, Sole F, Florensa L, Granada I, Domingo A, et al. CD5 negative and CD5 positive splenic marginal B-cell lymphomas have differential cytogenetic patterns. Leuk Res. 2005;29(8):981–2.
Swerdlow S, Campo E, Harris N, Jaffe E, Pileri S, Stein H, et al. WHO classification of tumours of haematopoietic and lymhoid tissues. Revised 4th ed. Lyon: IARC; 2017.
Hunter ZR, Branagan AR, Manning R, Patterson CJ, Santos DD, Tournilhac O, et al. CD5, CD10, and CD23 expression in Waldenstrom’s macroglobulinemia. Clin Lymphoma. 2005;5(4):246–9.
Dong HY, Gorczyca W, Liu Z, Tsang P, Wu CD, Cohen P, et al. B-cell lymphomas with coexpression of CD5 and CD10. Am J Clin Pathol. 2003;119(2):218–30.
Molina TJ, Lin P, Swerdlow SH, Cook JR. Marginal zone lymphomas with plasmacytic differentiation and related disorders. Am J Clin Pathol. 2011;136(2):211–25.
Marti GE, Rawstron AC, Ghia P, Hillmen P, Houlston RS, Kay N, et al. Diagnostic criteria for monoclonal B-cell lymphocytosis. Br J Haematol. 2005;130(3):325–32.
Hallek M, Cheson BD, Catovsky D, Caligaris-Cappio F, Dighiero G, Dohner H, et al. Guidelines for the diagnosis and treatment of chronic lymphocytic leukemia: a report from the International Workshop on Chronic Lymphocytic Leukemia updating the National Cancer Institute-Working Group 1996 guidelines. Blood. 2008;111(12):5446–56.
Rawstron AC, Shanafelt T, Lanasa MC, Landgren O, Hanson C, Orfao A, et al. Different biology and clinical outcome according to the absolute numbers of clonal B-cells in monoclonal B-cell lymphocytosis (MBL). Cytometry B Clin Cytom. 2010;78(Suppl 1):S19–23.
Kostopoulos IV, Paterakis G, Papadimitriou K, Pavlidis D, Tsitsilonis OE, Papadhimitriou SI. Immunophenotypic analysis reveals heterogeneity and common biologic aspects in monoclonal B-cell lymphocytosis. Genes Chromosomes Cancer. 2015;54(4):210–21.
Fazi C, Scarfo L, Pecciarini L, Cottini F, Dagklis A, Janus A, et al. General population low-count CLL-like MBL persists over time without clinical progression, although carrying the same cytogenetic abnormalities of CLL. Blood. 2011;118(25):6618–25.
Rawstron AC, Bennett FL, O’Connor SJ, Kwok M, Fenton JA, Plummer M, et al. Monoclonal B-cell lymphocytosis and chronic lymphocytic leukemia. N Engl J Med. 2008;359(6):575–83.
Shanafelt TD, Kay NE, Rabe KG, Call TG, Zent CS, Maddocks K, et al. Brief report: natural history of individuals with clinically recognized monoclonal B-cell lymphocytosis compared with patients with Rai 0 chronic lymphocytic leukemia. J Clin Oncol. 2009;27(24):3959–63.
Gibson SE, Swerdlow SH, Ferry JA, Surti U, Dal Cin P, Harris NL, et al. Reassessment of small lymphocytic lymphoma in the era of monoclonal B-cell lymphocytosis. Haematologica. 2011;96(8):1144–52.
Morton LM, Wang SS, Devesa SS, Hartge P, Weisenburger DD, Linet MS. Lymphoma incidence patterns by WHO subtype in the United States, 1992-2001. Blood. 2006;107(1):265–76.
Noone AM, Howlader N, Krapcho M, Miller D, Brest A, Yu M, et al. SEER cancer statistics review, 1975–2015. Bethesda: National Cancer Institute; 2018.
Deegan MJ, Abraham JP, Sawdyk M, Van Slyck EJ. High incidence of monoclonal proteins in the serum and urine of chronic lymphocytic leukemia patients. Blood. 1984;64(6):1207–11.
Gine E, Martinez A, Villamor N, Lopez-Guillermo A, Camos M, Martinez D, et al. Expanded and highly active proliferation centers identify a histological subtype of chronic lymphocytic leukemia (“accelerated” chronic lymphocytic leukemia) with aggressive clinical behavior. Haematologica. 2010;95(9):1526–33.
Ciccone M, Agostinelli C, Rigolin GM, Piccaluga PP, Cavazzini F, Righi S, et al. Proliferation centers in chronic lymphocytic leukemia: correlation with cytogenetic and clinicobiological features in consecutive patients analyzed on tissue microarrays. Leukemia. 2012;26(3):499–508.
Falchi L, Keating MJ, Marom EM, Truong MT, Schlette EJ, Sargent RL, et al. Correlation between FDG/PET, histology, characteristics, and survival in 332 patients with chronic lymphoid leukemia. Blood. 2014;123(18):2783–90.
Menter T, Trivedi P, Ahmad R, Flora R, Dirnhofer S, Tzankov A, et al. Diagnostic utility of lymphoid enhancer binding factor 1 immunohistochemistry in small B-cell lymphomas. Am J Clin Pathol. 2017;147(3):292–300.
Tandon B, Peterson L, Gao J, Nelson B, Ma S, Rosen S, et al. Nuclear overexpression of lymphoid-enhancer-binding factor 1 identifies chronic lymphocytic leukemia/small lymphocytic lymphoma in small B-cell lymphomas. Mod Pathol. 2011;24(11):1433–43.
Palumbo GA, Parrinello N, Fargione G, Cardillo K, Chiarenza A, Berretta S, et al. CD200 expression may help in differential diagnosis between mantle cell lymphoma and B-cell chronic lymphocytic leukemia. Leuk Res. 2009;33(9):1212–6.
Espinet B, Ferrer A, Bellosillo B, Nonell L, Salar A, Fernandez-Rodriguez C, et al. Distinction between asymptomatic monoclonal B-cell lymphocytosis with cyclin D1 overexpression and mantle cell lymphoma: from molecular profiling to flow cytometry. Clin Cancer Res. 2014;20(4):1007–19.
Zhou Y, Wang H, Fang W, Romaguer JE, Zhang Y, Delasalle KB, et al. Incidence trends of mantle cell lymphoma in the United States between 1992 and 2004. Cancer. 2008;113(4):791–8.
Samaha H, Dumontet C, Ketterer N, Moullet I, Thieblemont C, Bouafia F, et al. Mantle cell lymphoma: a retrospective study of 121 cases. Leukemia. 1998;12(8):1281–7.
Fernandez V, Salamero O, Espinet B, Sole F, Royo C, Navarro A, et al. Genomic and gene expression profiling defines indolent forms of mantle cell lymphoma. Cancer Res. 2010;70(4):1408–18.
Orchard J, Garand R, Davis Z, Babbage G, Sahota S, Matutes E, et al. A subset of t(11;14) lymphoma with mantle cell features displays mutated IgVH genes and includes patients with good prognosis, nonnodal disease. Blood. 2003;101(12):4975–81.
Bea S, Valdes-Mas R, Navarro A, Salaverria I, Martin-Garcia D, Jares P, et al. Landscape of somatic mutations and clonal evolution in mantle cell lymphoma. Proc Natl Acad Sci U S A. 2013;110(45):18250–5.
Jares P, Colomer D, Campo E. Molecular pathogenesis of mantle cell lymphoma. J Clin Invest. 2012;122(10):3416–23.
Ondrejka SL, Lai R, Smith SD, Hsi ED. Indolent mantle cell leukemia: a clinicopathological variant characterized by isolated lymphocytosis, interstitial bone marrow involvement, kappa light chain restriction, and good prognosis. Haematologica. 2011;96(8):1121–7.
Majlis A, Pugh WC, Rodriguez MA, Benedict WF, Cabanillas F. Mantle cell lymphoma: correlation of clinical outcome and biologic features with three histologic variants. J Clin Oncol. 1997;15(4):1664–71.
Young KH, Chan WC, Fu K, Iqbal J, Sanger WG, Ratashak A, et al. Mantle cell lymphoma with plasma cell differentiation. Am J Surg Pathol. 2006;30(8):954–61.
Pinyol M, Hernandez L, Cazorla M, Balbin M, Jares P, Fernandez PL, et al. Deletions and loss of expression of p16INK4a and p21Waf1 genes are associated with aggressive variants of mantle cell lymphomas. Blood. 1997;89(1):272–80.
Ott G, Kalla J, Hanke A, Muller JG, Rosenwald A, Katzenberger T, et al. The cytomorphological spectrum of mantle cell lymphoma is reflected by distinct biological features. Leuk Lymphoma. 1998;32(1–2):55–63.
Bea S, Ribas M, Hernandez JM, Bosch F, Pinyol M, Hernandez L, et al. Increased number of chromosomal imbalances and high-level DNA amplifications in mantle cell lymphoma are associated with blastoid variants. Blood. 1999;93(12):4365–74.
Bosch F, Lopez-Guillermo A, Campo E, Ribera JM, Conde E, Piris MA, et al. Mantle cell lymphoma: presenting features, response to therapy, and prognostic factors. Cancer. 1998;82(3):567–75.
Herrero-Vicent C, Machado I, Illueca C, Avaria A, Salazar C, Hernandez A, et al. Diagnostic and therapeutic update of mantle cell lymphoma (MCL): analysis of seven cases treated in a centre in one year. Ecancermedicalscience. 2016;10:627.
Yamaguchi M, Seto M, Okamoto M, Ichinohasama R, Nakamura N, Yoshino T, et al. De novo CD5+ diffuse large B-cell lymphoma: a clinicopathologic study of 109 patients. Blood. 2002;99(3):815–21.
Al-Kawaaz M, Mathew S, Liu Y, Gomez ML, Chaviano F, Knowles DM, et al. Cyclin D1-positive diffuse large B-cell lymphoma with IGH-CCND1 translocation and BCL6 rearrangement. a report of two cases Am J Clin Pathol. 2015;143(2):288–99.
Chuang WY, Chang H, Chang GJ, Wang TH, Chang YS, Wang TH, et al. Pleomorphic mantle cell lymphoma morphologically mimicking diffuse large B cell lymphoma: common cyclin D1 negativity and a simple immunohistochemical algorithm to avoid the diagnostic pitfall. Histopathology. 2017;70(6):986–99.
Bermudez G, Gonzalez de Villambrosia S, Martinez-Lopez A, Batlle A, Revert-Arce JB, Cereceda Company L, et al. Incidental and isolated follicular lymphoma in situ and mantle cell lymphoma in situ lack clinical significance. Am J Surg Pathol. 2016;40(7):943–9.
Carvajal-Cuenca A, Sua LF, Silva NM, Pittaluga S, Royo C, Song JY, et al. In situ mantle cell lymphoma: clinical implications of an incidental finding with indolent clinical behavior. Haematologica. 2012;97(2):270–8.
Jegalian AG, Eberle FC, Pack SD, Mirvis M, Raffeld M, Pittaluga S, et al. Follicular lymphoma in situ: clinical implications and comparisons with partial involvement by follicular lymphoma. Blood. 2011;118(11):2976–84.
Carbone A, Santoro A. How I treat: diagnosing and managing “in situ” lymphoma. Blood. 2011;117(15):3954–60.
Gradowski JF, Sargent RL, Craig FE, Cieply K, Fuhrer K, Sherer C, et al. Chronic lymphocytic leukemia/small lymphocytic lymphoma with cyclin D1 positive proliferation centers do not have CCND1 translocations or gains and lack SOX11 expression. Am J Clin Pathol. 2012;138(1):132–9.
Sherman MJ, Hanson CA, Hoyer JD. An assessment of the usefulness of immunohistochemical stains in the diagnosis of hairy cell leukemia. Am J Clin Pathol. 2011;136(3):390–9.
Teixeira Mendes LS, Peters N, Attygalle AD, Wotherspoon A. Cyclin D1 overexpression in proliferation centres of small lymphocytic lymphoma/chronic lymphocytic leukaemia. J Clin Pathol. 2017;70(10):899–902.
Hoechtlen-Vollmar W, Menzel G, Bartl R, Lamerz R, Wick M, Seidel D. Amplification of cyclin D1 gene in multiple myeloma: clinical and prognostic relevance. Br J Haematol. 2000;109(1):30–8.
Chen YH, Gao J, Fan G, Peterson LC. Nuclear expression of sox11 is highly associated with mantle cell lymphoma but is independent of t(11;14)(q13;q32) in non-mantle cell B-cell neoplasms. Mod Pathol. 2010;23(1):105–12.
Narurkar R, Alkayem M, Liu D. SOX11 is a biomarker for cyclin D1-negative mantle cell lymphoma. Biomark Res. 2016;4:6.
Muller AM, Ihorst G, Mertelsmann R, Engelhardt M. Epidemiology of non-Hodgkin’s lymphoma (NHL): trends, geographic distribution, and etiology. Ann Hematol. 2005;84(1):1–12.
Freedman A. Follicular lymphoma: 2018 update on diagnosis and management. Am J Hematol. 2018;93(2):296–305.
Montoto S, Davies AJ, Matthews J, Calaminici M, Norton AJ, Amess J, et al. Risk and clinical implications of transformation of follicular lymphoma to diffuse large B-cell lymphoma. J Clin Oncol. 2007;25(17):2426–33.
Hans CP, Weisenburger DD, Vose JM, Hock LM, Lynch JC, Aoun P, et al. A significant diffuse component predicts for inferior survival in grade 3 follicular lymphoma, but cytologic subtypes do not predict survival. Blood. 2003;101(6):2363–7.
Katzenberger T, Kalla J, Leich E, Stocklein H, Hartmann E, Barnickel S, et al. A distinctive subtype of t(14;18)-negative nodal follicular non-Hodgkin lymphoma characterized by a predominantly diffuse growth pattern and deletions in the chromosomal region 1p36. Blood. 2009;113(5):1053–61.
Siddiqi IN, Friedman J, Barry-Holson KQ, Ma C, Thodima V, Kang I, et al. Characterization of a variant of t(14;18) negative nodal diffuse follicular lymphoma with CD23 expression, 1p36/TNFRSF14 abnormalities, and STAT6 mutations. Mod Pathol. 2016;29(6):570–81.
Wang SA, Wang L, Hochberg EP, Muzikansky A, Harris NL, Hasserjian RP. Low histologic grade follicular lymphoma with high proliferation index: morphologic and clinical features. Am J Surg Pathol. 2005;29(11):1490–6.
Koster A, Tromp HA, Raemaekers JM, Borm GF, Hebeda K, Mackenzie MA, et al. The prognostic significance of the intra-follicular tumor cell proliferative rate in follicular lymphoma. Haematologica. 2007;92(2):184–90.
Cong P, Raffeld M, Teruya-Feldstein J, Sorbara L, Pittaluga S, Jaffe ES. In situ localization of follicular lymphoma: description and analysis by laser capture microdissection. Blood. 2002;99(9):3376–82.
Eshoa C, Perkins S, Kampalath B, Shidham V, Juckett M, Chang CC. Decreased CD10 expression in grade III and in interfollicular infiltrates of follicular lymphomas. Am J Clin Pathol. 2001;115(6):862–7.
Yegappan S, Schnitzer B, Hsi ED. Follicular lymphoma with marginal zone differentiation: microdissection demonstrates the t(14;18) in both the follicular and marginal zone components. Mod Pathol. 2001;14(3):191–6.
Lai R, Arber DA, Chang KL, Wilson CS, Weiss LM. Frequency of bcl-2 expression in non-Hodgkin’s lymphoma: a study of 778 cases with comparison of marginal zone lymphoma and monocytoid B-cell hyperplasia. Mod Pathol. 1998;11(9):864–9.
Pezzella F, Tse AG, Cordell JL, Pulford KA, Gatter KC, Mason DY. Expression of the bcl-2 oncogene protein is not specific for the 14;18 chromosomal translocation. Am J Pathol. 1990;137(2):225–32.
Schraders M, de Jong D, Kluin P, Groenen P, van Krieken H. Lack of Bcl-2 expression in follicular lymphoma may be caused by mutations in the BCL2 gene or by absence of the t(14;18) translocation. J Pathol. 2005;205(3):329–35.
Menter T, Gasser A, Juskevicius D, Dirnhofer S, Tzankov A. Diagnostic utility of the germinal center-associated markers GCET1, HGAL, and LMO2 in hematolymphoid neoplasms. Appl Immunohistochem Mol Morphol. 2015;23(7):491–8.
Ferreri AJ, Zucca E. Marginal-zone lymphoma. Crit Rev Oncol Hematol. 2007;63(3):245–56.
Khalil MO, Morton LM, Devesa SS, Check DP, Curtis RE, Weisenburger DD, et al. Incidence of marginal zone lymphoma in the United States, 2001-2009 with a focus on primary anatomic site. Br J Haematol. 2014;165(1):67–77.
Chacon JI, Mollejo M, Munoz E, Algara P, Mateo M, Lopez L, et al. Splenic marginal zone lymphoma: clinical characteristics and prognostic factors in a series of 60 patients. Blood. 2002;100(5):1648–54.
Berger F, Felman P, Thieblemont C, Pradier T, Baseggio L, Bryon PA, et al. Non-MALT marginal zone B-cell lymphomas: a description of clinical presentation and outcome in 124 patients. Blood. 2000;95(6):1950–6.
Traverse-Glehen A, Bertoni F, Thieblemont C, Zucca E, Coiffier B, Berger F, et al. Nodal marginal zone B-cell lymphoma: a diagnostic and therapeutic dilemma. Oncology (Williston Park). 2012;26(1):92-9, 103-4.
Campo E, Miquel R, Krenacs L, Sorbara L, Raffeld M, Jaffe ES. Primary nodal marginal zone lymphomas of splenic and MALT type. Am J Surg Pathol. 1999;23(1):59–68.
Mollejo M, Camacho FI, Algara P, Ruiz-Ballesteros E, Garcia JF, Piris MA. Nodal and splenic marginal zone B cell lymphomas. Hematol Oncol. 2005;23(3–4):108–18.
Castillo JJ, Olszewski AJ, Kanan S, Meid K, Hunter ZR, Treon SP. Overall survival and competing risks of death in patients with Waldenström macroglobulinaemia: an analysis of the Surveillance, Epidemiology and End Results database. Br J Haematol. 2015;169(1):81–9.
Sekhar J, Sanfilippo K, Zhang Q, Trinkaus K, Vij R, Morgensztern D. Waldenstrom macroglobulinemia: a surveillance, epidemiology, and end results database review from 1988 to 2005. Leuk Lymphoma. 2012;53(8):1625–6.
Banwait R, Aljawai Y, Cappuccio J, McDiarmid S, Morgan EA, Leblebjian H, et al. Extramedullary Waldenstrom macroglobulinemia. Am J Hematol. 2015;90(2):100–4.
Lin P, Bueso-Ramos C, Wilson CS, Mansoor A, Medeiros LJ. Waldenstrom macroglobulinemia involving extramedullary sites: morphologic and immunophenotypic findings in 44 patients. Am J Surg Pathol. 2003;27(8):1104–13.
Cesana C, Barbarano L, Miqueleiz S, Lucchesini C, Ricci F, Varettoni M, et al. Clinical characteristics and outcome of immunoglobulin M-related disorders. Clin Lymphoma. 2005;5(4):261–4.
Dimopoulos MA, Gertz MA, Kastritis E, Garcia-Sanz R, Kimby EK, Leblond V, et al. Update on treatment recommendations from the Fourth International Workshop on Waldenstrom’s Macroglobulinemia. J Clin Oncol. 2009;27(1):120–6.
Merlini G, Baldini L, Broglia C, Comelli M, Goldaniga M, Palladini G, et al. Prognostic factors in symptomatic Waldenstrom’s macroglobulinemia. Semin Oncol. 2003;30(2):211–5.
Nobile-Orazio E, Marmiroli P, Baldini L, Spagnol G, Barbieri S, Moggio M, et al. Peripheral neuropathy in macroglobulinemia: incidence and antigen-specificity of M proteins. Neurology. 1987;37(9):1506–14.
Silberman J, Lonial S. Review of peripheral neuropathy in plasma cell disorders. Hematol Oncol. 2008;26(2):55–65.
Gertz MA, Kyle RA, Noel P. Primary systemic amyloidosis: a rare complication of immunoglobulin M monoclonal gammopathies and Waldenstrom’s macroglobulinemia. J Clin Oncol. 1993;11(5):914–20.
Cao X, Medeiros LJ, Xia Y, Wang X, Thomas SK, Loghavi S, et al. Clinicopathologic features and outcomes of lymphoplasmacytic lymphoma patients with monoclonal IgG or IgA paraprotein expression. Leuk Lymphoma. 2016;57(5):1104–13.
Minnema MC, Kimby E, D’Sa S, Fornecker LM, Poulain S, Snijders TJ, et al. Guideline for the diagnosis, treatment and response criteria for Bing-Neel syndrome. Haematologica. 2017;102(1):43–51.
Policepatil SM, Go RS, Zeng GG. Floral variant of follicular lymphoma. Am J Hematol. 2011;86(6):503.
Kojima M, Yamanaka S, Yoshida T, Shimizu K, Murayama K, Ohno Y, et al. Histological variety of floral variant of follicular lymphoma. APMIS. 2006;114(9):626–32.
Younes SF, Beck AH, Lossos IS, Levy R, Warnke RA, Natkunam Y. Immunoarchitectural patterns in follicular lymphoma: efficacy of HGAL and LMO2 in the detection of the interfollicular and diffuse components. Am J Surg Pathol. 2010;34(9):1266–76.
Nathwani BN, Anderson JR, Armitage JO, Cavalli F, Diebold J, Drachenberg MR, et al. Clinical significance of follicular lymphoma with monocytoid B cells. Non-Hodgkin’s Lymphoma Classification Project. Hum Pathol. 1999;30(3):263–8.
Muller-Hermelink HK, Zettl A, Pfeifer W, Ott G. Pathology of lymphoma progression. Histopathology. 2001;38(4):285–306.
Keith TA, Cousar JB, Glick AD, Vogler LB, Collins RD. Plasmacytic differentiation in follicular center cell (FCC) lymphomas. Am J Clin Pathol. 1985;84(3):283–90.
Matsuda I, Shimizu Y, Okamoto T, Hirota S. Follicular lymphoma mimicking marginal zone lymphoma in lymph node: a case report. Int J Clin Exp Pathol. 2014;7(10):7076–81.
Vago JF, Hurtubise PE, Redden-Borowski MM, Martelo OJ, Swerdlow SH. Follicular center-cell lymphoma with plasmacytic differentiation, monoclonal paraprotein, and peripheral blood involvement. Recapitulation of normal B-cell development. Am J Surg Pathol. 1985;9(10):764–70.
Lai R, Weiss LM, Chang KL, Arber DA. Frequency of CD43 expression in non-Hodgkin lymphoma. A survey of 742 cases and further characterization of rare CD43+ follicular lymphomas. Am J Clin Pathol. 1999;111(4):488–94.
van den Brand M, van Krieken JH. Recognizing nodal marginal zone lymphoma: recent advances and pitfalls. A systematic review. Haematologica. 2013;98(7):1003–13.
Seegmiller AC, Xu Y, McKenna RW, Karandikar NJ. Immunophenotypic differentiation between neoplastic plasma cells in mature B-cell lymphoma vs plasma cell myeloma. Am J Clin Pathol. 2007;127(2):176–81.
Lin P, Hao S, Handy BC, Bueso-Ramos CE, Medeiros LJ. Lymphoid neoplasms associated with IgM paraprotein: a study of 382 patients. Am J Clin Pathol. 2005;123(2):200–5.
Evans HL, Polski JM, Deshpande V, Dunphy CH. CD5+ true SLL/CLL with plasmacytic differentiation and an unusual 1p36 translocation: case report and review of the literature. Leuk Lymphoma. 2000;39(5–6):625–32.
Lin P, Molina TJ, Cook JR, Swerdlow SH. Lymphoplasmacytic lymphoma and other non-marginal zone lymphomas with plasmacytic differentiation. Am J Clin Pathol. 2011;136(2):195–210.
Rosado FG, Morice WG, He R, Howard MT, Timm M, McPhail ED. Immunophenotypic features by multiparameter flow cytometry can help distinguish low grade B-cell lymphomas with plasmacytic differentiation from plasma cell proliferative disorders with an unrelated clonal B-cell process. Br J Haematol. 2015;169(3):368–76.
Cozzolino I, Vigliar E, Sosa Fernandez LV, Selleri C, Pepe S, Vitale M, et al. Non lymphomatous clonal B-cell populations in enlarged lymph nodes in acquired immunodeficiency syndrome. Infez Med. 2012;20(Suppl 2):35–42.
Jordan RC, Masaki Y, Takeshita S, Speight PM, Sugai S. High prevalence of B-cell monoclonality in labial gland biopsies of Japanese Sjogren’s syndrome patients. Int J Hematol. 1996;64(1):47–52.
Kussick SJ, Kalnoski M, Braziel RM, Wood BL. Prominent clonal B-cell populations identified by flow cytometry in histologically reactive lymphoid proliferations. Am J Clin Pathol. 2004;121(4):464–72.
Matsubayashi S, Tamai H, Morita T, Fukata S, Matsuzuka F, Suzuki T, et al. Hashimoto’s thyroiditis manifesting monoclonal lymphocytic infiltration. Clin Exp Immunol. 1990;79(2):170–4.
Locker J, Nalesnik M. Molecular genetic analysis of lymphoid tumors arising after organ transplantation. Am J Pathol. 1989;135(6):977–87.
Pelicci PG, Knowles DM, Arlin ZA, Wieczorek R, Luciw P, Dina D, et al. Multiple monoclonal B cell expansions and c-myc oncogene rearrangements in acquired immune deficiency syndrome-related lymphoproliferative disorders. Implications for lymphomagenesis. J Exp Med. 1986;164(6):2049–60.
Lu C, He Q, Zhu W, Fu C, Zhou J, Tao Y, et al. The value of detecting immunoglobulin gene rearrangements in the diagnosis of B-cell lymphoma. Oncotarget. 2017;8(44):77009–19.
Dohner H, Stilgenbauer S, Benner A, Leupolt E, Krober A, Bullinger L, et al. Genomic aberrations and survival in chronic lymphocytic leukemia. N Engl J Med. 2000;343(26):1910–6.
Arcaini L, Lucioni M, Boveri E, Paulli M. Nodal marginal zone lymphoma: current knowledge and future directions of an heterogeneous disease. Eur J Haematol. 2009;83(3):165–74.
Ayyappan S, William BM. Marginal zone lymphoma: clinicopathologic variations and approaches to therapy. Curr Oncol Rep. 2018;20(4):33.
Leich E, Salaverria I, Bea S, Zettl A, Wright G, Moreno V, et al. Follicular lymphomas with and without translocation t(14;18) differ in gene expression profiles and genetic alterations. Blood. 2009;114(4):826–34.
Treon SP, Xu L, Yang G, Zhou Y, Liu X, Cao Y, et al. MYD88 L265P somatic mutation in Waldenstrom’s macroglobulinemia. N Engl J Med. 2012;367(9):826–33.
Gachard N, Parrens M, Soubeyran I, Petit B, Marfak A, Rizzo D, et al. IGHV gene features and MYD88 L265P mutation separate the three marginal zone lymphoma entities and Waldenstrom macroglobulinemia/lymphoplasmacytic lymphomas. Leukemia. 2013;27(1):183–9.
Ngo VN, Young RM, Schmitz R, Jhavar S, Xiao W, Lim KH, et al. Oncogenically active MYD88 mutations in human lymphoma. Nature. 2011;470(7332):115–9.
Nakamura T, Tateishi K, Niwa T, Matsushita Y, Tamura K, Kinoshita M, et al. Recurrent mutations of CD79B and MYD88 are the hallmark of primary central nervous system lymphomas. Neuropathol Appl Neurobiol. 2016;42(3):279–90.
Kraan W, Horlings HM, van Keimpema M, Schilder-Tol EJ, Oud ME, Scheepstra C, et al. High prevalence of oncogenic MYD88 and CD79B mutations in diffuse large B-cell lymphomas presenting at immune-privileged sites. Blood Cancer J. 2013;3:e139.
Pham-Ledard A, Beylot-Barry M, Barbe C, Leduc M, Petrella T, Vergier B, et al. High frequency and clinical prognostic value of MYD88 L265P mutation in primary cutaneous diffuse large B-cell lymphoma, leg-type. JAMA Dermatol. 2014;150(11):1173–9.
Landgren O, Tageja N. MYD88 and beyond: novel opportunities for diagnosis, prognosis and treatment in Waldenstrom’s Macroglobulinemia. Leukemia. 2014;28(9):1799–803.
Cheah CY, Seymour JF, Wang ML. Mantle cell lymphoma. J Clin Oncol. 2016;34(11):1256–69.
Damle RN, Wasil T, Fais F, Ghiotto F, Valetto A, Allen SL, et al. Ig V gene mutation status and CD38 expression as novel prognostic indicators in chronic lymphocytic leukemia. Blood. 1999;94(6):1840–7.
Durig J, Naschar M, Schmucker U, Renzing-Kohler K, Holter T, Huttmann A, et al. CD38 expression is an important prognostic marker in chronic lymphocytic leukaemia. Leukemia. 2002;16(1):30–5.
Ibrahim S, Keating M, Do KA, O’Brien S, Huh YO, Jilani I, et al. CD38 expression as an important prognostic factor in B-cell chronic lymphocytic leukemia. Blood. 2001;98(1):181–6.
Jelinek DF, Tschumper RC, Geyer SM, Bone ND, Dewald GW, Hanson CA, et al. Analysis of clonal B-cell CD38 and immunoglobulin variable region sequence status in relation to clinical outcome for B-chronic lymphocytic leukaemia. Br J Haematol. 2001;115(4):854–61.
Bulian P, Shanafelt TD, Fegan C, Zucchetto A, Cro L, Nuckel H, et al. CD49d is the strongest flow cytometry-based predictor of overall survival in chronic lymphocytic leukemia. J Clin Oncol. 2014;32(9):897–904.
Hamblin TJ, Davis Z, Gardiner A, Oscier DG, Stevenson FK. Unmutated Ig V(H) genes are associated with a more aggressive form of chronic lymphocytic leukemia. Blood. 1999;94(6):1848–54.
Rosenwald A, Alizadeh AA, Widhopf G, Simon R, Davis RE, Yu X, et al. Relation of gene expression phenotype to immunoglobulin mutation genotype in B cell chronic lymphocytic leukemia. J Exp Med. 2001;194(11):1639–47.
Durig J, Nuckel H, Cremer M, Fuhrer A, Halfmeyer K, Fandrey J, et al. ZAP-70 expression is a prognostic factor in chronic lymphocytic leukemia. Leukemia. 2003;17(12):2426–34.
Bakke AC, Purtzer Z, Leis J, Huang J. A robust ratio metric method for analysis of Zap-70 expression in chronic lymphocytic leukemia (CLL). Cytometry B Clin Cytom. 2006;70(4):227–34.
Gibbs G, Bromidge T, Howe D, Hopkins J, Johnson S. Comparison of flow cytometric methods for the measurement of ZAP-70 expression in a routine diagnostic laboratory. Clin Lab Haematol. 2005;27(4):258–66.
Chen YH, Peterson LC, Dittmann D, Evens A, Rosen S, Khoong A, et al. Comparative analysis of flow cytometric techniques in assessment of ZAP-70 expression in relation to IgVH mutational status in chronic lymphocytic leukemia. Am J Clin Pathol. 2007;127(2):182–91.
Dal-Bo M, Del Giudice I, Bomben R, Capello D, Bertoni F, Forconi F, et al. B-cell receptor, clinical course and prognosis in chronic lymphocytic leukaemia: the growing saga of the IGHV3 subgroup gene usage. Br J Haematol. 2011;153(1):3–14.
Crespo M, Bosch F, Villamor N, Bellosillo B, Colomer D, Rozman M, et al. ZAP-70 expression as a surrogate for immunoglobulin-variable-region mutations in chronic lymphocytic leukemia. N Engl J Med. 2003;348(18):1764–75.
Rosenquist R, Rosenwald A, Du MQ, Gaidano G, Groenen P, Wotherspoon A, et al. Clinical impact of recurrently mutated genes on lymphoma diagnostics: state-of-the-art and beyond. Haematologica. 2016;101(9):1002–9.
Malcikova J, Smardova J, Rocnova L, Tichy B, Kuglik P, Vranova V, et al. Monoallelic and biallelic inactivation of TP53 gene in chronic lymphocytic leukemia: selection, impact on survival, and response to DNA damage. Blood. 2009;114(26):5307–14.
Zenz T, Eichhorst B, Busch R, Denzel T, Habe S, Winkler D, et al. TP53 mutation and survival in chronic lymphocytic leukemia. J Clin Oncol. 2010;28(29):4473–9.
Stilgenbauer S, Furman RR, Zent CS. Management of chronic lymphocytic leukemia. Am Soc Clin Oncol Educ Book. 2015:164–75.
Hoster E, Dreyling M, Klapper W, Gisselbrecht C, van Hoof A, Kluin-Nelemans HC, et al. A new prognostic index (MIPI) for patients with advanced-stage mantle cell lymphoma. Blood. 2008;111(2):558–65.
Geisler CH, Kolstad A, Laurell A, Raty R, Jerkeman M, Eriksson M, et al. The Mantle Cell Lymphoma International Prognostic Index (MIPI) is superior to the International Prognostic Index (IPI) in predicting survival following intensive first-line immunochemotherapy and autologous stem cell transplantation (ASCT). Blood. 2010;115(8):1530–3.
Determann O, Hoster E, Ott G, Wolfram Bernd H, Loddenkemper C, Leo Hansmann M, et al. Ki-67 predicts outcome in advanced-stage mantle cell lymphoma patients treated with anti-CD20 immunochemotherapy: results from randomized trials of the European MCL Network and the German Low Grade Lymphoma Study Group. Blood. 2008;111(4):2385–7.
Mozos A, Royo C, Hartmann E, De Jong D, Baro C, Valera A, et al. SOX11 expression is highly specific for mantle cell lymphoma and identifies the cyclin D1-negative subtype. Haematologica. 2009;94(11):1555–62.
Halldorsdottir AM, Lundin A, Murray F, Mansouri L, Knuutila S, Sundstrom C, et al. Impact of TP53 mutation and 17p deletion in mantle cell lymphoma. Leukemia. 2011;25(12):1904–8.
Zhang J, Jima D, Moffitt AB, Liu Q, Czader M, Hsi ED, et al. The genomic landscape of mantle cell lymphoma is related to the epigenetically determined chromatin state of normal B cells. Blood. 2014;123(19):2988–96.
Bernard M, Gressin R, Lefrere F, Drenou B, Branger B, Caulet-Maugendre S, et al. Blastic variant of mantle cell lymphoma: a rare but highly aggressive subtype. Leukemia. 2001;15(11):1785–91.
Louie DC, Offit K, Jaslow R, Parsa NZ, Murty VV, Schluger A, et al. p53 overexpression as a marker of poor prognosis in mantle cell lymphomas with t(11;14)(q13;q32). Blood. 1995;86(8):2892–9.
Wotherspoon AC, Doglioni C, Diss TC, Pan L, Moschini A, de Boni M, et al. Regression of primary low-grade B-cell gastric lymphoma of mucosa-associated lymphoid tissue type after eradication of Helicobacter pylori. Lancet. 1993;342(8871):575–7.
Liu H, Ye H, Ruskone-Fourmestraux A, De Jong D, Pileri S, Thiede C, et al. T(11;18) is a marker for all stage gastric MALT lymphomas that will not respond to H. pylori eradication. Gastroenterology. 2002;122(5):1286–94.
Ye H, Liu H, Raderer M, Chott A, Ruskone-Fourmestraux A, Wotherspoon A, et al. High incidence of t(11;18)(q21;q21) in Helicobacter pylori-negative gastric MALT lymphoma. Blood. 2003;101(7):2547–50.
Hunter ZR, Xu L, Yang G, Zhou Y, Liu X, Cao Y, et al. The genomic landscape of Waldenstrom macroglobulinemia is characterized by highly recurring MYD88 and WHIM-like CXCR4 mutations, and small somatic deletions associated with B-cell lymphomagenesis. Blood. 2014;123(11):1637–46.
Treon SP, Cao Y, Xu L, Yang G, Liu X, Hunter ZR. Somatic mutations in MYD88 and CXCR4 are determinants of clinical presentation and overall survival in Waldenstrom macroglobulinemia. Blood. 2014;123(18):2791–6.
Treon SP, Tripsas CK, Meid K, Warren D, Varma G, Green R, et al. Ibrutinib in previously treated Waldenstrom’s macroglobulinemia. N Engl J Med. 2015;372(15):1430–40.
Chang CC, Osipov V, Wheaton S, Tripp S, Perkins SL. Follicular hyperplasia, follicular lysis, and progressive transformation of germinal centers. A sequential spectrum of morphologic evolution in lymphoid hyperplasia. Am J Clin Pathol. 2003;120(3):322–6.
Arber DA, George TI. Bone marrow biopsy involvement by non-Hodgkin’s lymphoma: frequency of lymphoma types, patterns, blood involvement, and discordance with other sites in 450 specimens. Am J Surg Pathol. 2005;29(12):1549–57.
Zhang QY, Foucar K. Bone marrow involvement by Hodgkin and non-Hodgkin lymphomas. Hematol Oncol Clin North Am. 2009;23(4):873–902.
Viswanatha D, Foucar K. Hodgkin and non-Hodgkin lymphoma involving bone marrow. Semin Diagn Pathol. 2003;20(3):196–210.
Schmidt B, Kremer M, Gotze K, John K, Peschel C, Hofler H, et al. Bone marrow involvement in follicular lymphoma: comparison of histology and flow cytometry as staging procedures. Leuk Lymphoma. 2006;47(9):1857–62.
Strati P, Shanafelt TD. Monoclonal B-cell lymphocytosis and early-stage chronic lymphocytic leukemia: diagnosis, natural history, and risk stratification. Blood. 2015;126(4):454–62.
Inamdar KV, Medeiros LJ, Jorgensen JL, Amin HM, Schlette EJ. Bone marrow involvement by marginal zone B-cell lymphomas of different types. Am J Clin Pathol. 2008;129(5):714–22.
Kent SA, Variakojis D, Peterson LC. Comparative study of marginal zone lymphoma involving bone marrow. Am J Clin Pathol. 2002;117(5):698–708.
Engels K, Oeschger S, Hansmann ML, Hillebrand M, Kriener S. Bone marrow trephines containing lymphoid aggregates from patients with rheumatoid and other autoimmune disorders frequently show clonal B-cell infiltrates. Hum Pathol. 2007;38(9):1402–11.
Franco V, Florena AM, Aragona F, Campesi G. Immunohistochemical evaluation of bone marrow lymphoid nodules in chronic myeloproliferative disorders. Virchows Arch A Pathol Anat Histopathol. 1991;419(4):261–6.
Johnston A, Brynes RK, Naemi K, Reisian N, Bhansali D, Zhao X, et al. Differentiating benign from malignant bone marrow B-cell lymphoid aggregates: a statistical analysis of distinguishing features. Arch Pathol Lab Med. 2015;139(2):233–40.
Sovani V, Harvey C, Haynes AP, McMillan AK, Clark DM, O’Connor SR. Bone marrow trephine biopsy involvement by lymphoma: review of histopathological features in 511 specimens and correlation with diagnostic biopsy, aspirate and peripheral blood findings. J Clin Pathol. 2014;67(5):389–95.
Johl A, Lengfelder E, Hiddemann W, Klapper W. Core needle biopsies and surgical excision biopsies in the diagnosis of lymphoma-experience at the Lymph Node Registry Kiel. Ann Hematol. 2016;95(8):1281–6.
Frederiksen JK, Sharma M, Casulo C, Burack WR. Systematic review of the effectiveness of fine-needle aspiration and/or core needle biopsy for subclassifying lymphoma. Arch Pathol Lab Med. 2015;139(2):245–51.
Zhang QY, Chabot-Richards D, Evans M, Spengel K, Andrews J, Kang H, et al. A retrospective study to assess the relative value of peripheral blood, bone marrow aspirate and biopsy morphology, immunohistochemical stains, and flow cytometric analysis in the diagnosis of chronic B cell lymphoproliferative neoplasms. Int J Lab Hematol. 2015;37(3):390–402.
Gujral S, Polampalli SN, Badrinath Y, Kumar A, Subramanian PG, Nair R, et al. Immunophenotyping of mature B-cell non Hodgkin lymphoma involving bone marrow and peripheral blood: critical analysis and insights gained at a tertiary care cancer hospital. Leuk Lymphoma. 2009;50(8):1290–300.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Gómez-Gélvez, J.C., Inamdar, K.V. (2020). Small B-Cell Lymphomas With and Without Plasmacytic Differentiation. In: Wang, E., Lagoo, A.S. (eds) Practical Lymph Node and Bone Marrow Pathology. Practical Anatomic Pathology. Springer, Cham. https://doi.org/10.1007/978-3-030-32189-5_5
Download citation
DOI: https://doi.org/10.1007/978-3-030-32189-5_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-32188-8
Online ISBN: 978-3-030-32189-5
eBook Packages: MedicineMedicine (R0)