Abstract
Obesity has become an epidemic, leading to increased interest in bariatric surgery as a treatment option. Many bariatric patients have had multiple failed attempts at weight loss and are looking for longer-lasting results. Although there is consensus for many surgical procedures, optimal preoperative management is more debated. Preoperative weight loss (PWL) has been proposed as a screening tool for predicting success in surgical candidates. It has also been mandated by many surgeons and insurers. This chapter will discuss the strategy of PWL and review the available evidence for and against PWL.
Similar content being viewed by others
Keywords
FormalPara Chapter Objectives-
1.
To explain the principles of preoperative weight loss
-
2.
To review the data supporting and refuting the benefits of preoperative weight loss
Introduction
Obesity has become an epidemic in the USA and around the world, leading to increased interest in bariatric surgery as a treatment option. Many bariatric patients have had multiple failed attempts at weight loss and are looking for longer-lasting results. Although there is consensus for many surgical procedures, optimal preoperative management is more debated. Preoperative weight loss (PWL) has been proposed as a screening tool for predicting success in surgical candidates. It has also been mandated by many surgeons and insurers [1]. This chapter will discuss the strategy of PWL and review the available evidence.
Principle Behind the Support of Preoperative Weight Loss
It is an accepted concept that patients who weigh less have decreased risk with surgery and less weight-related comorbidity. Thinner patients generally require less rigorous preoperative clearance than their heavier counterparts due to a lower burden of obesity-related disease [2]. In addition, it is technically easier to operate on someone who is thinner due to improved exposure and accessibility [3]. Preoperative programs to decrease body mass index (BMI) would theoretically result in decreased perioperative and postoperative complications such as bleeding, wound infection, etc. In addition, shorter operative times and hospital stays could occur. In addition to the hypothetical risk improvement with preoperative weight loss, many medical providers theorized that patients who are able to demonstrate PWL are more motivated and serious about adhering to postoperative diet and exercise recommendations. Based on these theoretical advantages, many physicians have supported PWL [4]. In addition, over the last several years, many insurance companies added attempted PWL as a prerequisite for surgery [1]. Many surgeons have questioned, however, if it is truly appropriate to exclude patients from definitive therapy if they prove that medical management is ineffective [5].
Most PWL programs include several meetings with nutritionists and physicians, as well as psychiatric assessments and weigh-ins at these appointments. If the patients are unable to show adequate weight loss or if they miss appointments, they are forced to start over or are even refused surgery. The guidelines used by some surgeons and insurance carriers originated with the National Institutes of Health (NIH) Consensus Development Conference on Gastrointestinal Surgery for Severe Obesity [6] convened in 1995 and published in 1998 [7]. This consensus group based the recommendation for attempted weight loss on a review of Medline queryable published reports. They supported attempted medical weight loss as some patients may be successful with diet and exercise alone; however, no data was presented to demonstrate differences with outcomes after weight loss surgery with or without pre-op diet attempts. In fact, the NIH panel concluded that less than 20% of patients have long-term success with diet and exercise alone, bringing into question the legitimacy of the proposed 6-month PWL requirement .
Since the NIH consensus panel, many authors have studied the impact of mandated PWL on eventual surgery. Jamal and colleagues compared two groups of patients: 72 undergoing a mandated 13-week dietary counseling program and 252 without this requirement. Both groups were similar preoperatively except for a slight difference in sleep apnea. The PWL group had a 50% higher dropout rate before surgery (28% versus 19%), lower percentage of excess weight loss (%EWL), and higher BMI and weight following surgery. Other tracked outcomes were equivalent [8].
Sadhasivam and colleagues performed a retrospective review of their bariatric surgery candidates from 2001 to 2005 and looked at reasons patients did not undergo surgery. They reviewed 1054 patients and found that only 519 (49%) underwent bariatric surgery and that 29.7% were denied due to insurance denial. Major denial reasons were that patients could not meet the strict preoperative prerequisites established, such as 5–10% reduction in BMI, documented prior weight loss attempts, multiple meetings with nutritionist, etc. Other reasons patients did not undergo surgery were because of frustration with the rigorous requirements and long waiting time. From 2001 to 2005, the authors demonstrated an increase in insurance denials from 9.9% to 19.9% [9]. This study is important in showing that insurance company mandates are resulting in increasing denials for bariatric surgery coverage.
Review of the Data Supporting and Refuting the Benefit of Preoperative Weight Loss
Postoperative Weight Loss
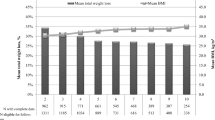
The Obesity Surgery Mortality Risk Score has been used as a strategy to predict perioperative mortality risk [2]. It is a multivariable analysis used to identify BMI >50, hypertension (HTN), male gender, elevated pulmonary embolism risk, and age >45 years as independent risk variables for bariatric surgery [2]. Among those variables, BMI is the only one that can be modified preoperatively, potentially supporting mandated PWL for higher-risk patients. However, several studies addressing PWL as a means for risk reduction have failed to demonstrate a benefit. Harnisch and colleagues compared two groups of patients undergoing Roux-en-Y gastric bypass (RYGB), those achieving greater than 10 lbs. weight loss (88 patients) before surgery and those that instead gained at least 10 lb. (115 patients). The authors failed to find a difference in perioperative complications, comorbidity resolution, or weight loss at 12 months compared to the immediate preoperative weight [10]. Alami and colleagues completed a rare randomized controlled trial study comparing 26 patients completing the required PWL versus 35 with no preoperative diet requirements [11]. Although excess weight loss was noted to be greater in the PWL group compared to the non-PWL at 6 weeks and 3 months, there was no change in 6-month follow-up visit and 1-year postoperative weight loss. In addition, the groups showed no difference in intraoperative complications or conversions, complication rates, blood loss, or hospital stay. In the 12-month follow-up reported by Solomon, there was also no difference in BMI or comorbidity resolution at 1 year in the population as a whole. A small benefit in %EWL at 1 year was seen, however, in the subgroup able to lose more than 5%EWL preoperatively [12].
In 2011, Cassie, Menezes, and Birch reviewed 17 studies, including 4611 patients that showed PWL beneficial, and 20 studies with 2075 patients showing no benefits to PWL [13]. This analysis includes the studies previously discussed in this chapter (Table 10.1). Most reviewed analyses focused on the 12-month follow-up point. Combining all studies reporting 12-month data, the non-preoperative weight loss groups had an estimated weight loss of 70.7 ± 5.7% versus the preoperative weight loss group of 69.0 ± 7.1%. At 2 years, there was still no significant difference in both weight groups with the PWL showing 66.7 ± 2.7% estimated weight loss and the non-preoperative weight loss group at 72 ± 6.3%. The authors concluded that there was inadequate data to support mandated PWL based on the outcome of postoperative weight loss [1, 2].
Livhits and colleagues performed a meta-analysis of 15 articles including 3404 patients. Only two of the included cohorts were excluded from the Cassie review . Not surprisingly, the authors drew similar conclusions. Of the 15 articles analyzed, 5 studies had positive effects for PWL, 2 studies showed positive short-term effects, 5 studies showed no difference, and 1 study showed a negative effect. Overall no significant heterogeneity was seen among the studies with results of postoperative weight loss [3].
Operative Time
One of the hypothesized benefits of PWL includes shorter operative times, so looking at the studies that analyzed, this is important in determining if PWL is needed. In the Alami study, total operating time was greater in the non-preoperative weight loss group (257.6 ± 27.8 min versus 220.2 ± 31.5 min) as compared with the preoperative weight loss group [4]. Harnisch and colleagues also found a slight benefit in OR time with PWL (119.7 versus 104.9 min, P = 0.02) [5]. The savings of 12.5–23 min with PWL are consistent in other studies as well [1, 3]. The problem with these papers is that it is not properly distinguished how operating time is measured, so there could be a discrepancy in what is a standardized operating time. Also, there is no study so far that has demonstrated that the time saved has contributed to improved patient safety and outcomes.
Operative Complications
Livhits and colleagues proposed that meta-analysis of complications is difficult due to the lack of consistency in definition. However, they concluded that there was no significant difference between groups [3]. Cassie noted decreased complications with PWL in 2 of 11 studies. However, when the data from the reviewed papers were pooled, the complication rates for the preoperative weight loss group were 18.8 ± 10.6% versus 21.4 ± 13.1% in the non-preoperative weight loss group showing that there was no real difference in the two groups [1].
Hospital Stay
Decreased length of stay is one benefit that would also result in cost-reducing measures, but again there are inadequate data to support a length of stay benefit with PWL. Cassie reported on five studies with the length of stay ranging from 2.2 to 4.3 days for the PWL versus 2.3–6.0 days for the non-preoperative weight loss group. The mean from pooled studies was 3.34 ± 0.83 for the PWL versus 3.98 ± 1.49 days for the non-preoperative weight loss group [1]. Although there was a trend in support of PWL, the data are inconclusive.
Liver Reduction and VLED
Many bariatric surgeons have recognized variability in fatty liver intraoperatively and attribute reduced liver size to preoperative weight loss. Some surgeons have specifically implemented a very-low-energy diet (VLED) for weight loss and liver volume reduction. Colles investigated the actual changes in liver volume and the pattern of this change with VLED, the relative change in liver volume, body weight and visceral and subcutaneous adipose tissue (VAT/SAT) areas, the clinical and biochemical risk factors that may predict an enlarged pretreatment liver or predict the total change in liver volume after treatment, patient acceptability and compliance, and treatment side effects. Patients with BMI between 40 and 50 were chosen based on the fact that surgeons find that patients in this range posed the greatest surgical difficultly. The diet itself consisted of three shakes/day providing 456 kcal, 52 g protein, 7 g fat, and 45 g carbohydrate plus the recommended daily allowance of vitamins, minerals, and trace elements. This diet took place over 12 weeks. The changes in the liver were assessed by computed tomography (CT) scan and magnetic resonance imaging (MRI) during the 12-week interval (Fig. 10.1). At the end of the diet, the average decrease in liver size was 18.7%. Also, this study showed that the larger the initial liver volume, the better the decrease in liver volume. The authors reported no hepatomegaly in the study patients and a low perioperative risk, although the study was not powered for complications. The most important pattern noted is that the majority of the volume reduction occurred within the first 2 weeks [6]. This data supports potential benefit with PWL; however, a short 2-week time course may be adequate.
Single cross-sectional images of the liver performed by computed tomography at baseline and week 12 of a very-low-energy diet. The images, taken from within a series of contiguous 8-mm slices used to calculate total liver volume, illustrate the extent of the change in liver volume with weight loss in a 35-year-old man with an initial liver volume of 3.7 L and final liver volume of 2.4 L. A 35% reduction in liver size and a weight loss of 18 kg were observed
Super Obese
Characteristics that put patients at a higher level of risk for bariatric surgery include BMI >50, male gender, and a lower socioeconomic status. The Veterans Affairs Pittsburgh Healthcare System became a great source for evaluating this specific type of population. Collins and colleagues looked at changes in liver volume and adipose tissue in patients with BMI >50 [7]. The authors felt these patients in theory would benefit most from a reduction in liver volume and adipose tissue to facilitate surgery and decrease complication rates. The comorbidities with increased prevalence in the super obese include all those associated with obesity: type II diabetes mellitus, hypertension, obstructive sleep apnea, congestive heart failure, and so on. The technical difficulties related to this population of patients include thick abdominal wall, excess visceral adipose tissue, a relatively short mesentery, and an enlarged fatty liver. Altering these characteristics should in theory decrease complication rates and shorten operative times.
To achieve acute preoperative weight loss, Collins employed a liquid low-calorie diet consisting of 800 kcal/day, nutritional and behavioral counseling, and education with the goal of a 10% weight loss reduction. The goal of this study was to evaluate change in obesity-related comorbidities, liver volume, and subcutaneous adipose tissue over several weeks. Since the weight loss and methods were drastic, the patients were required to have multiple assessments during their preoperative course. The authors also tracked changes in mediations, weekly laboratory tests, and weekly physical exams because of the aggressive nature of the weight loss. At baseline and after the completion of the diet program, computed tomography (CT) scans of the abdomen were compared. A total of 30 patients underwent the program with a mean BMI at baseline of 56, mean age 53. The program lasted a total of 9 weeks, and the patients had an average body weight loss of 12.1%. After the low-calorie diet was completed, the mean BMI decreased to 49. They recognized an 18% decrease in liver volume over 9 weeks in patients enrolled in the study. They did not, however, compare complications or outcomes to patients not completing the diet. Their final conclusion is that a preoperative diet is safe to decrease liver volume for bariatric surgery in an effort to improve perioperative and postoperative course, especially for those with a BMI >50. As with Colles and Collins, other studies have supported this finding as well [8].
Additional Considerations with PWL
Most bariatric patients gain some portion of their weight back after their postoperative nadir. It is supported by most surgeons that weight regain and weight loss failure are largely tied to behavioral and psychosocial causes, although recent research suggests that the root cause of weight regain may be due to the genetic predisposition [9] or from alteration of the physiological mechanisms by which metabolic operations appear to work [10,11,12].
The psychosocial benefit of PWL may have the most dramatic results on maintaining postoperative weight loss in the long term. Sarwer analyzed the relationship between preoperative eating behavior and postoperative dietary adherence [13]. The goal of this study was to look at the relationship of postoperative weight loss to preoperative psychosocial variables such as self-esteem and mood, as well as preoperative eating behaviors, dietary intake, and patients’ self-reported adherence to the postoperative diet over a 92-week period. Approximately 200 patients participated in the study, with the initial evaluation at 4 weeks before surgery. The participants completed a psychosocial/behavioral evaluation to assess their appropriateness for surgery followed by a packet of questionnaires. They were again asked to fill out the questionnaires at 20, 40, 66, and 92 weeks after surgery. The packet included the following measures: Rosenberg Self-Esteem Scale, Beck Depression Inventory-II, Positive and Negative Affect Scale, Eating Inventory, Block 98 Food Frequency Questionnaire, dietary adherence, and weight. Approximately 2 weeks prior to surgery, the participants met with a dietician and were instructed on dietary and behavioral changes that the authors felt would give them the best postoperative outcome, followed by dietary instructions postoperatively to help maintain the weight loss. From the variables that were looked at, the ones that were significant predictors for success (measured by percentage of weight loss over time) included gender, baseline cognitive restraint, and self-reported dietary adherence. Those patients who were able to show cognitive restraint preoperatively also did well at 20 weeks postoperatively, when the patients were advanced back to a regular diet. Those individuals who scored greater in the dietary adherence experienced a weight loss that was 2.4% points greater at postoperative week 40 and 3.8% points greater at week 66 compared to those patients with a lower score on the dietary adherence. By week 92, both groups had regained some of their weight, but the group that scored in the high adherence group still had achieved a weight loss that was 4.5% points greater than those in the low adherence group, representing a 28% greater weight loss. This study was able to demonstrate improvements in psychosocial status postoperatively. They had improved self-esteem, increased positive affect, and decreased negative affect and depressive symptoms, as well as had changes in their eating habits [13]. These results suggest that there is a positive psychosocial benefit to nutritional and behavioral education, although not necessarily PWL. Teaching better eating habits not only helps the patients maintain postoperative weight loss but also improves their self-esteem. All these translate to patients who participate in a preoperative educational program and may be better equipped to help keep off weight postoperatively. As a result, Sarwer supports that PWL should be encouraged but not used as a way to screen for surgical candidates who would obtain the most from bariatric surgery.
Study Limitations
The studies reviewed in this chapter have some limitations to address. Only one study is available with a prospective, randomized study design [4]; however, even in this analysis, fewer than 100 patients were available. The other studies are primarily retrospective studies with significant variability in data collection. Larger-scale, prospective randomized trials would need to support a benefit in PWL before this should be mandated. The Sarwer study was limited due to the high number of attrition, which is typical for these types of studies, and only a 2-week educational period prior to surgery. Only 56% of the patients completed the study, impacting the significance of the paper by decreasing the population size. Another limitation to this paper was that the data was based on self-analysis, which is difficult to interpret [13].
ASMBS Position Statement
The American Society for Metabolic and Bariatric Surgery (ASMBS) issued a position statement due to questions raised to the society by physicians, hospitals, patients, and insurance companies regarding preoperative weight loss [14]. (This statement is reviewed in Chap. 11.) The final summary and recommendations, as also demonstrated by the studies reviewed here, are that there is a low level of evidence supporting the need for preoperative weight loss. Class I or evidence-based studies currently are not available to support the request for mandated PWL. Lower levels of evidence do exist, but the data and results are not consistent. Although there is some evidence in the Class II–IV range for acute preoperative weight loss, the studies are not consistent, and some are conflicting, leaving us with no clear answers. There is some low level of evidence to suggest that preoperative weight loss can help with evaluating a patient’s adherence to the new lifestyle, but this should be judged by each individual situation. The studies so far have shown no difference in comorbidity improvement, postoperative complications, or postoperative weight loss to justify the need for PWL. The current recommendation is that insurance companies and physicians should reevaluate the need for PWL. Thus far, it contributes to higher attrition rates, increases frustration among patients, and blocks certain patients from obtaining a life-altering and beneficial surgery.
Conclusion
The only evidence-based support for preoperative education and encouraging PWL is that these tools may help patients prepare for surgery and understand techniques to maintain a healthier lifestyle postoperatively. The data so far is inconsistent and inconclusive with regard to the benefits of PWL, but the majority of the studies show no difference in complication rates or morbidities in patients undergoing PWL versus no PWL. If considering PWL, the data supports the notion that shorter-term preoperative diets (i.e., 2 weeks) may also reduce liver volume and reduce operative time, without significant reduction in risk. Mandated programs in excess of this are a barrier to our patients and without supportive evidence.
Question Section
-
1.
Studies have shown that a very-low-energy diet has been beneficial and should be started preoperatively. What is the optimal timing for starting the diet?
-
A.
2 weeks
-
B.
6 weeks
-
C.
8 weeks
-
D.
12 weeks
-
A.
-
2.
The ASMBS position statement was issued to clarify the validity of PWL by reviewing the current literature and evidence. The statement’s final conclusion is that there is a strong level of evidence to justify the use of PWL.
-
A.
True
-
B.
False
-
A.
References
Cassie S, Menezes C, Birch DW, Shi X, Karmali S. Effect of preoperative weight loss in bariatric surgical patients: a systematic review. Surg Obes Relat Dis. 2011;7(6):760–7.
Ray EC, Nickels MW, Sayeed S, Sax HC. Predicting success after gastric bypass: the role of psychosocial and behavioral factors. Surgery. 2003;134(4):555–63.. discussion 563–4
Livhits M, Mercado C, Yermilov I, Parikh JA, Dutson E, Mehran A, et al. Does weight loss immediately before bariatric surgery improve surgical outcomes: a systematic review. Surg Obes Relat Dis. 2009;5(6):713–21.
Alami RS, Morton JM, Schuster R, Lie J, Sanchez BR, Peters A, et al. Is there a benefit to preoperative weight loss in gastric bypass patients? A prospective randomized trial. Surg Obes Relat Dis. 2007;3(2):141–5.. discussion 145–6
Harnisch MC, Portenier DD, Pryor AD, Prince-Petersen R, Grant JP, DeMaria EJ. Preoperative weight gain does not predict failure of weight loss or co-morbidity resolution of laparoscopic roux-en-y gastric bypass for morbid obesity. Surg Obes Relat Dis. 2008;4(3):445–50.
Colles SL, Dixon JB, Marks P, Strauss BJ, O’Brien PE. Preoperative weight loss with a very-low-energy diet: quantitation of changes in liver and abdominal fat by serial imaging. Am J Clin Nutr. 2006;84(2):304–11.
Collins J, McCloskey C, Titchner R, Goodpaster B, Hoffman M, Hauser D, et al. Preoperative weight loss in high-risk superobese bariatric patients: a computed tomography-based analysis. Surg Obes Relat Dis. 2011;7(4):480–5.
Fris RJ. Preoperative low energy diet diminishes liver size. Obes Surg. 2004;14(9):1165–70.
Matzko ME, Argyropoulos G, Wood GC, Chu X, McCarter RJ, Still CD, et al. Association of ghrelin receptor promoter polymorphisms with weight loss following Roux-en-Y gastric bypass surgery. Obes Surg. 2012;22(5):783–90.
Liou AP, Paziuk M, Luevano JM Jr, Machineni S, Turnbaugh PJ, Kaplan LM. Conserved shifts in the gut microbiota due to gastric bypass reduce host weight and adiposity. Sci Transl Med. 2013;5(178):178ra41.
Angelakis E, Armougom F, Million M, Raoult D. The relationship between gut microbiota and weight gain in humans. Future Microbiol. 2012;7(1):91–109.
Frazier TH, DiBaise JK, McClain CJ. Gut microbiota, intestinal permeability, obesity-induced inflammation, and liver injury. JPEN J Parenter Enteral Nutr. 2011;35(5 Suppl):14S–20.
Sarwer DB, Wadden TA, Moore RH, Baker AW, Gibbons LM, Raper SE, et al. Preoperative eating behavior, postoperative dietary adherence and weight loss after gastric bypass surgery. Surg Obes Relat Dis. 2008;4(5):640–6.
Brethauer S. ASMBS position statement on preoperative supervised weight loss requirements. Surg Obes Relat Dis. 2011;7(3):257–60.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Wakily, H., Pryor, A.D. (2020). Evaluation of Preoperative Weight Loss. In: Nguyen, N., Brethauer, S., Morton, J., Ponce, J., Rosenthal, R. (eds) The ASMBS Textbook of Bariatric Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-27021-6_10
Download citation
DOI: https://doi.org/10.1007/978-3-030-27021-6_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-27020-9
Online ISBN: 978-3-030-27021-6
eBook Packages: MedicineMedicine (R0)