Abstract
Transcranial magnetic stimulation (TMS) is increasingly used as a diagnostic and therapeutic tool for neuropsychiatric disorders. TMS for treatment of depression during pregnancy is an appealing alternative to fetus-threatening drugs. However, there are no studies to date that evaluate the safety of TMS for a pregnant mother and her fetus. Two scenarios are possible in practice: (i) pregnant woman as a patient and (ii) pregnant woman as an operator. The goal of the present study is to estimate maximum field exposures for the fetus in both scenarios. A full-body finite element method (FEM) compatible model of a pregnant woman with about 100 tissue parts has been developed for the present study. This model allows detailed computations of induced current/electric field in every tissue given different locations of a figure-eight coil, a biphasic pulse, common TMS pulse durations, and using different values of the TMS intensity measured in standard motor threshold (SMT) units. Along with the numerical simulations, we use a simple analytical estimation model; both approaches confirm and augment each other. Our simulation/analytical results estimate the maximum peak values of the electric field in the fetal area and beyond in 48 (operator/patient) representative cases, for every fetal tissue separately and for a TMS intensity of one SMT unit. This study provides the first detailed data on risk to fetal exposure to induced fields by TMS in pregnant patients and pregnant operators. It is expandable to any patient/operator configuration by applying a simple analytical upper estimate of field strength/eddy current density.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Brain stimulation
- Transcranial magnetic stimulation
- Safety
- Pregnancy
- Human phantom
- Finite element analysis
1 Introduction
Recent studies confirm the efficacy of transcranial magnetic stimulation (TMS) as a noninvasive treatment of medication-resistant depression [1, 2]. Four different devices, the Neuronetics Neurostar Stimulator, Brainsway H-Coil system, Magstim Magnetic Stimulator, and MagVenture Stimulator, have been cleared by the U.S. Food and Drug Administration (FDA) for the treatment of medication-resistant depression [3, 4].
Even though TMS coil holders, and even robots, have been developed that might make the application of TMS more spatially precise and efficient, to date, TMS is often applied by an operator who manually positions and retains the TMS coil over the subject’s head. A potential safety concern is thus generated when the operator is a woman and is pregnant. There are no studies to date that assess the safety of TMS for a fetus. In the case of a pregnant woman as a TMS operator, we must consider two possibilities:
-
Standard operation with the TMS coil held at distances of approximately 1–2 ft from the belly
-
Accidental TMS coil discharge when the coil is in direct contact with the belly or in its immediate vicinity
In addition to the scenario of a pregnant woman as a TMS operator, the possibility of a pregnant woman as a TMS patient is also important to consider. TMS can cause a generalized tonic seizure, which can pose a significant risk for the integrity of a pregnancy. Therefore, in most instances, pregnancy will be an exclusion criterion for TMS. However, a considerable percentage of women experience symptoms of depression during pregnancy and develop clinical depression requiring medical intervention. TMS has been proposed as a method to treat maternal depression while avoiding fetal exposure to drugs [5, 6]. So while the risk-benefit profile is argued to be better for TMS than for medications, one must consider that TMS may cause fetal exposure to high induced currents.
In estimating acceptable levels of induced currents, we refer to guidelines from the International Commission on Non-Ionizing Radiation Protection (ICNIRP) [7, 8]. The 2010 ICNIRP basic restrictions for occupational exposure to time-varying electric and magnetic fields for frequencies in the band 1 Hz–100 kHz [8] recommend that the exposure should be limited to electric fields in the head and body of less than 800 mV/m in order to avoid peripheral and central myelinated nerve stimulation. ICNIRP also recommends that the restrictions on electric or magnetic fields including transient or very short-term peak fields (which are encountered during TMS) be regarded as instantaneous values which should not be time averaged.
We assume that the estimate of 0.8 V/m maximum peak field should also apply to the fetal brain, body, and trunk.
2 Methods and Materials
2.1 Existing Computational Models of a Pregnant Woman
Induction currents in the entire human body (or bodies) of a pregnant subject caused by a TMS coil can be established in every particular case via numerical electromagnetic modeling. One of the primary investigated concerns has been a significant electric current density, which may develop in the highly conducting amniotic fluid surrounding the fetus and subject to an external time-varying magnetic field [9, 10]. Table 3.1 lists computational models of a pregnant woman and/or a fetus currently available for electromagnetic and radiological simulations.
These models (except for Refs. [10, 11], which are highlighted in the table) are based on insertion of a fetus into an existing nonpregnant female model. Meanwhile, the models developed from scans of pregnant females include the abdominal region only [10, 11].
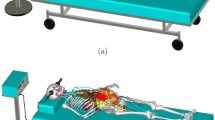
All models in Table 3.1 are voxel models, except for Ref. [11] which used B-splines or NURBS, while some parts of the body are adapted from the Visible Human Project [12, 13]. Figure 3.1 shows a NURBS model from Ref. [11], while Fig. 3.2 shows the voxel model family from Ref. [14].
NURBS model of a pregnant woman [11]
Voxel model of a pregnant woman [16]
2.2 Construction of FEM (CAD) Full-Body Pregnant Woman Model and Model Topology
The voxel models listed in Table 3.1 are perfectly fine for radiation dosimetry studies [10, 11, 18] and for high-frequency and RF simulation studies of specific absorption rates [14,15,16, 18] based on the finite-difference time-domain (FDTD) approach. However, they are not suitable for the finite element method (FEM), which is generally employed by the TMS community [23,24,25,26,27,28,29,30,31,32,33]. This method more accurately captures complicated coil geometry(s) and curved boundaries between tissues. The NURBS surfaces [11] also have limited value for an FEM solver, which internally operates with geometry primitives: triangular facets and tetrahedra. A conversion from NURBS surfaces to triangular surfaces may require (very) significant additional meshing time.
To enable FEM analysis, a full-body CAD model of a pregnant female in the form of triangular surface meshes has been developed. As an initial dataset, we have chosen the detailed voxel model of a pregnant female by Nagaoka [14, 17, 18]; see second row of Table 3.1. We received the voxel model after signing a licensing agreement with the National Institute of Information and Communications Technology, Japan. This model is based on a 22-year-old pregnant Japanese female (26th week or second trimester) [17]. The original pregnant female voxel model was developed from MRI data collected on a nonpregnant Japanese woman who was 160 cm tall and weighed 53 kg. Further, abdominal MR images of a 26-week pregnant woman were segmented and inserted into this full-body model.
We converted this voxel model into an FEM CAD model using isosurface extraction in ITK-SNAP [35] and MATLAB. Mesh decimation, healing, and smoothing were performed using custom MATLAB scripts and ANSYS SpaceClaim. Standard mesh intersection approaches [36,37,38,39,40,41] typically result in a large number of triangles close to intersection chains and loops. Furthermore, they leave coincident faces, which might create compatibility problems. Resulting object intersections (which are usually “shallow” intersections) were resolved by locally moving intersecting surfaces in their respective normal directions with a step size of 0.2 mm or so until the intersection was no longer present [42, 43].
A well-known problem with FEM models is object matching in a contact region. Usually, the contact region is not explicitly defined in an imported CAD model and has to be discovered separately by testing for face-to-face overlaps and matching CAD faces/edges [44]. This circumstance may lead to problems for certain CAD kernels such as ACIS. To prevent CAD import errors, a thin gap was introduced between all tissue objects and was filled with “average body properties” of an outer enclosing shell. In some sense, this gap represents membranes separating different tissues. If the gap is reasonably small, it provides a close approximation to reality for different physical processes.
In order to construct the fetus model representing a pregnant female during the first and third trimester, we used the base data for the second trimester and the deformation approach described in Refs. [14, 18].
Figure 3.3 shows three variations of the CAD model constructed for the present study. The corresponding tissue mesh inventory is summarized in Supplement I. To our knowledge, this is the only detailed FEM-compatible model of a pregnant female currently available. The current model contains approximately 100 individual parts. Its distinct feature is a continuous CSF shell around the gray matter for both the mother and the fetus. Creation and testing required about 12 man months and continues as a work in progress. Figure 3.4 illustrates the corresponding fetal volume (second trimester) on a larger scale.
Other biomechanical CAD models of pregnant women having different degrees of approximation have also been constructed [45,46,47,48]. However, these models do not include detailed geometry of the fetus suitable for EM simulation [47,48,49,50]. Figure 3.4 demonstrates the corresponding fetal volume (second trimester) on a larger scale.
2.3 Tissue Properties
Most tissues were assigned material properties (conductivity and dielectric constant) following the Gabriel & Gabriel database [49], which is further replicated in the IT’IS database [50]. Fetal properties follow Refs. [11, 51] and are outlined in Table 3.2. The conductivity and permittivity of fetal brain are comparable to that of the fetus and also behave similarly. Hence, the fetal brain is assigned scaled fetus material properties; the scaling factor is obtained from the available dataset. The material property values assigned to all tissues are also provided in the supplement.
3 Study Design
3.1 TMS Coil
Similar to Ref. [26], the base coil is a figure-eight straight coil with a loop radius of 35 mm. However, instead of a stranded conductor, a solid conductor (copper) with a diameter of 8 mm was used.
3.2 Pulse Form and Duration
TMS pulse forms vary widely in shape and duration [52,53,54,55]. Table 3.3 summarizes the data for four common FDA-approved TMS machines.
In order to take the majority of cases into consideration, we have chosen a simple biphasic harmonic coil pulse current:
The derivative of the coil current, I, is proportional to the induced electric field/induced electric current in the body. In order to include the majority of cases from Table 3.3, the total pulse duration or length τ was evaluated for two limiting values:
Please note that the equivalent frequency of the biphasic harmonic pulse given by (3.1) is
Other more elaborate pulse forms have also been studied [62].
3.3 Coil Current
For every pulse duration and coil position, the coil current amplitude I0 in (3.1) has been found from the condition of one standard motor threshold (SMT) unit [61, 62]. One SMT means that the electric field at a point 2 cm from the surface of the head beneath the coil center reaches the motor threshold value of approximately 130 V/m [61, 62]. Motor threshold, a measure of the TMS intensity necessary to evoke a peripheral motor response, is variable across individuals but is also remarkably constant in a given individual [63]. For example, the peak coil current for a 0.1-ms-long pulse was found to be approximately 9000 A·turns magnetomotive force (mmf) at 1 SMT unit.
3.4 Coil Positions
Two coil positions for a pregnant patient have been considered (see Fig. 3.5). In the first case (Fig. 3.5a), the straight coil is located 10 mm above the top of the head. In the second case (Fig. 3.5b), the straight coil is translated and then tilted by 60 degrees. The first case might represent a standard TMS coil placement for studies aimed at evaluating central motor conduction, though a circular TMS coil would be generally used in such instances. The second case aims to approximate the position of the TMS for the treatment of depression.
A coil positioning map for the pregnant operator is shown in Fig. 3.6 for the second trimester. The closest distance from the coil center to the body is 115 mm. We consider three representative polarizations of the major current dipole of the coil:
-
A.
In the coronal plane (z-polarization in Fig. 3.6, Config. A, labeled as A1-A6)
-
B.
In the sagittal plane (y-polarization in Fig. 3.6, Config. B, labeled as B1-B6)
-
C.
In the transverse plane (x-polarization in Fig. 3.6, Config. C, labeled as C1-C4)
For every polarization type, four to six representative coil locations have been tested in the sagittal plane as shown in Fig. 3.6. The operator could achieve any of these positions by moving their right arm along with the coil holder. This results in a total of 16 test cases. For each test case, the eddy current density and the corresponding electric field everywhere in the body were computed. Each test case is conducted for the first, second, and third trimesters. For the first trimester, the closest distance from the coil center to the body is 45 mm (B) or 80 mm (C), 115 mm (B) and (C) for the second, and for the third – 40 mm (B) and 80 mm (C). The remaining topology is the same.
3.5 Accidental Coil Discharge
Two extreme cases have also been considered, which are not shown in Fig. 3.6. These are when the coil is moved in the xy-plane until it is as close to the body as possible. These cases will be labeled as B7, B8 and C5, C6, respectively.
3.6 Frequency-Domain Computations
All simulations were performed in the frequency domain using ANSYS Maxwell 3D FEM software (v. 16). ANSYS Maxwell 3D is a commercial FEM software package with adaptive mesh refinement and has been extensively used for eddy current computations, similar to the earlier studies [24,25,26]. The software takes into account both conduction and displacement currents (as well as free and polarization charges), and solves the full-wave Maxwell equation for the magnetic field, H, in the frequency domain
where σ is the local medium conductivity, and ε and μ are the local permittivity and permeability, respectively. The major difference from the full-wave case is that the phase is assumed to be constant over the volume of interest. Although Maxwell 3D also has a transient FEM solver, this solver does not take into account the displacement currents and was therefore not used.
All simulations made use of the automated adaptive meshing technology available in Maxwell to iteratively refine the mesh. Five adaptive meshing passes were performed during the calculation, with the final meshes approaching about 2 M tetrahedra. Details of the adaptive mesh refinement procedure have been discussed previously [60].
3.7 Time-Domain Computations
Frequency-domain results (coil excitation with a sinusoidal waveform) for fields and currents have been collected for multiple frequencies (a logarithmic frequency sweep) over the band from 300 Hz to 3 MHz in order to generate the required pulse forms via the fast Fourier transform (FFT) and inverse FFT (IFFT) as described in Ref. [60]. The corresponding method has been described in the same reference; it is time-consuming but accurate. The time-domain solution is required for any pulse form including the harmonic pulses given by (3.1) since they are distorted quite differently from the harmonic wave of the same frequency. This solution is also important for other (nonharmonic) pulse forms [60].
3.8 Finding Maximum Peak Current Density/Electric Field Strength in Individual Tissues
A uniform 5 × 5 × 5 mm grid of observation points was introduced within a rectangular box, which covers the abdominal area only. This resulted in approximately 150,000 observation points within the body, where the induced current and the electric field are evaluated. For every such point, the pulse form has been restored via IFFT. Then, interpolation of peak pulse values onto a finer 2 × 2 × 2 mm grid was performed, followed by averaging over each small tissue volume as recommended in Ref. [8]. Finally, the absolute maximum peak current/field has been evaluated for every all tissues.
4 Results: Pregnant Patient
4.1 Qualitative Behavior of Induced Currents in the Body of a Pregnant Patient at Different Frequencies (Pulse Durations)
Figure 3.7 shows eddy current amplitude distribution in a coronal plane of a pregnant patient for three representative frequencies: 3 kHz, 30 kHz, and 300 kHz. The coil current amplitude is 10,000 A (10,000 A·turns mmf). Note that the color scale has been multiplied by the factor of 10 for every subsequent figure.
Eddy current amplitude distribution in a coronal plane for three representative frequencies: 3 kHz, 30 kHz, and 300 kHz (second trimester model). The coil current amplitude is 10,000 A (10,000 A·turns mmf). Note that the color scale was increased by a factor of 10 and 100 for the middle and right-hand figures, respectively
We observe that the peak current in the fetal area does not exceed 0.1 mA/m2, 1 mA/m2, and 40 mA/m2. Comparing Fig. 3.7a, b, the induced current initially appears to behave as a linear function of frequency. However, the behavior becomes nonlinear after 30 kHz or so as seen in Fig. 3.7c.
We also observe that the bulk of the induced current at any frequency is primarily excited in the amniotic fluid, but not in the fetus. This is to be expected due the very high conductivity of the amniotic fluid.
4.2 Quantitative Results for Maximum Peak Electric Field at One SMT Unit
In the subsequent study, the excitation is always given by a biphasic pulse from Eqs. (3.1)–(3.3) and the TMS intensity is always equal to one SMT unit. Figure 3.8 presents the results for the maximum peak electric field (maximum magnitude of the electric field vector, E(t)) for the two coil configurations in Fig. 3.5, respectively, and for every involved tissue. The first, second, and third trimester models were used in this study.
4.3 Comparison with the Recommended Safe Value of Electric Field
According to the safety requirements discussed in the Introduction, the peak electric field throughout the fetal volume (including fetus, placenta, uterus, and amniotic fluid) shall not exceed 800 mV/m. This condition is certainly met for all cases given in Fig. 3.8, even using a reduction factor of 10. One obvious reason is that the magnetic field from the coil decays very rapidly far from the head, being approximately proportional to the inverse third power of the distance [64].
4.4 Observations from the Quantitative Solution
The following observations follow from the analysis of the results given in Fig. 3.8:
-
Values of the peak electric field obtained using the condition of one STM unit weakly depend on the pulse duration. This is in contrast to the results shown in Fig. 3.7, where the dependence on frequency is paramount. The reason is the normalization condition of one SMT unit, which means, for example, that the amplitude of the coil current is significantly increased for the 1.0 ms pulse.
-
The largest fields are observed in the placenta/uterus.
-
The smallest fields are observed in the fetal brain.
-
Peak values for two different coil orientations are quite similar.
-
The third trimester is characterized by somewhat larger values of the maximum peak electrical field as compared to the first and second trimesters.
These observations suggest that the results given in Fig. 3.8 are rather general and should be valid for a wide variety of coil orientations and pulse durations.
4.5 Comparison with Upper Analytical Estimate for Electric Fields/Eddy Currents
Using a simplified upper analytical estimate for eddy current/induced electric field in the human body [60], the local electric field anywhere within the body is expressed directly through a time-varying lumped coil current, I0f(t), in the following form
This estimate does not depend on the specific human model under study. We first apply eq. (3.5) to the coil setup from Fig. 3.5a, assuming an observation point located beneath the coil center and at a distance of 62 mm from the coil (representing the distance from the coil center to the top of the uterus for the present model). The resulting upper electric field estimate is obtained as 90 mV/m at any pulse duration (when normalized to one SMT unit). Neither of the maximum peak values in Fig. 3.8 for the coil from Fig. 3.5a exceeds this value. For the coil from Fig. 3.5b, the same or a more elaborate estimate (with spatial averaging to undo a loci effect) [60] can be applied. Again, neither of the maximum peak values in Fig. 3.8 for the coil from Fig. 3.5b exceeds the value of 90 mV/m. Hence, the upper analytical estimate given by (3.5) is justified for all considered cases.
4.6 Using the Analytical Estimate for Predicting Maximum Fields for Different Patients
To provide results which may be expected for different patients, we apply the upper analytical estimate of Eq. (3.5) to different distances from the coil center to the top (or a closest point in the general case) of the uterus. The corresponding data rounded to within ±3 mV/m is summarized in Table 3.4. Although the present results are given for one specific coil type, similar estimates may be expected for other coil geometries according to the study performed in Ref. [60].
5 Results: Pregnant Operator and Accidental Coil Discharge
5.1 Quantitative Results for Maximum Peak Electric Field at One SMT Unit
All coil configurations shown in Fig. 3.6 have been studied for three stages of pregnancy and for different pulse durations. Figure 3.9 presents typical data for the second trimester and for the biphasic pulse of 0.1 ms duration. The following observations can be made from these and other relevant computations:
-
For coil positions in close proximity to the belly (A-1, A-2, C-1), the peak electric field in the fetal volume may exceed the safe limit of 800 mV.
-
When the distance from the coil center to the nearest point of the uterus is less than 60 cm, the maximum peak values in excess of 100 mV/m may be observed (this number is adopted from Table 3.4).
-
When the distance from the coil center to the nearest point of the uterus is greater than 60 cm, the upper estimate from Table 3.4 can be applied.
Maximum peak electric field values for the second trimester for all coil configurations/positions depicted in Fig. 3.6
Coil polarization B in Fig. 3.6 creates the smallest values of the peak electric field. This result is to be expected since the equivalent dipole of the figure-eight coil is essentially perpendicular to the abdominal surface.
5.2 Accidental Coil Discharge
In the two extreme cases (polarization B and C in Fig. 3.6), the coil is placed as close to the body as possible by moving it in the xy-plane. The corresponding cases for polarization B and C in Fig. 3.6 have been labeled as B7, B8 and C5, C6, respectively. The corresponding maximum peak field values for the entire fetal volume are shown in Fig. 3.10. For these cases, the suggested limit of 800 mV/m may be exceeded by a factor of ten or higher. Similar results were obtained for polarization A for similar extreme coil placements.
Maximum peak electric field values for all trimesters and for all coil positions listed in Fig. 3.6
6 Conclusion
At present, safe limits of fetal exposure to TMS electric and magnetic fields are an open subject. This study aimed to perform both numerical and analytical analyses of this important issue.
As a limit of the maximum peak electric field observed in the fetal volume, we have chosen the value of 800 mV/m, which allows us to avoid peripheral and central myelinated nerve stimulation [8].
Our numerical and analytical estimates for biphasic TMS pulses of different durations provide similar safety estimates. They reveal that:
-
1.
For the TMS intensity of one SMT unit and when the closest distance between the center of the coil and the uterus is greater than or equal to 60 cm (2 ft.), the maximum peak electric field in the fetal volume (including fetus, placenta, uterus, amniotic fluid) is expected to be less than or equal to 100 mV/m. This value is significantly lower than the recommended safe limit of 800 mV/m.
-
2.
The estimate given above was shown for any stage of pregnancy, for two realistic pulse durations, and for pregnant woman either as a patient or an operator.
-
3.
This estimate appears to scale linearly with TMS intensity. For example, at the TMS intensity of 1.5 SMT unit, the peak field in the fetal volume is less than or equal to 100 × 1.5 = 150 mV/m when the closest distance between the coil center and the uterus is still 60 cm or greater.
-
4.
This estimate is scaled approximately proportional to the inverse third power of the distance. For example, at the TMS intensity of one SMT unit, the peak field in the fetal volume is less than 100 × (6/5)3 ~ 170 mV/m when the closest distance between the coil center and the uterus is 50 cm or greater.
-
5.
The following approximate equation for the maximum peak electric field E in the fetal volume is suggested
where d is the closest distance between the coil center and the uterus in cm and I is the TMS intensity in SMT units. We expect (3.6) to hold at the distances d gretater than 30 cm.
-
6.
FDA-cleared TMS devices employ a TMS coil holder. A pregnant operator can (and should) maintain a larger – and thus safer – distance when using a coil holder during TMS treatment. However, the possibility of accidental TMS coil discharge close to the belly has to be considered. In this case, the suggested limit of 800 mV/m may be exceeded by a factor of ten or greater.
-
7.
Given the unknown biological consequences of a large number of pulses in a typical treatment sequence, the decision of whether to use TMS for treatment of depression (the only currently approved indication) should be based on a risk-benefit analysis. In considering the risk-benefit balance, it is important to contemplate the fetal risks posed by pharmacologic treatments for depression in pregnant patients [65, 66]. For more experimental and less evidence-supported indications, a prudent course of action would be to avoid the use of TMS in pregnant women. In any case, appropriate informed consent is critical.
The content of this chapter is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University, and its affiliated academic health care centers, the National Institutes of Health, or the Sidney R. Baer Jr. Foundation.
References
Rossi, S., et al.; Safety of TMS Consensus Group. (2009). Safety ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research. Clinical Neurophysiology, 120(12), 2008–2039.
Fox, M. D., et al. (2013). Identification of reproducible individualized targets for treatment of depression with TMS based on intrinsic connectivity. NeuroImage, 66, 151–160.
DeNoon, D. J. (2008, October). Brain-stimulating device cleared for depression treatment after 1 drug failure. WebMD. [Online]. Available: http://www.webmd.com/depression/news/20081008/fda-oks-tms-depression-device
Brainsway. (2013, Jan.) gets FDA approval for anti-depression device. Reuters. [Online]. Available: http://www.reuters.com/article/2013/01/09/brainsway-fda-idUSL5E9C99OU20130109
Kim, D. R., et al. (2011). An open label pilot study of transcranial magnetic stimulation for pregnant women with major depressive disorder. Journal of Women’s Health, 20(2), 255–261.
Kim, D. R., et al. (2011). A survey of patient acceptability of repetitive transcranial magnetic stimulation (TMS) during pregnancy. Journal of Affective Disorders, 129(1–3), 385–390.
ICNIRP. (1998). Guidelines for limiting exposure to time-varying electric, magnetic and electromagnetic fields (up to 300 GHz). Health Physics, 74(4), 494–522.
ICNIRP. (2010). Guidelines for limiting exposure to time-varying electric and magnetic fields (1 Hz – 100 kHz). Health Physics, 99(6), 818–836.
Dimbylow, P. (2006). Development of pregnant female, hybrid voxel-mathematical models and their application to the dosimetry of applied magnetic and electric fields at 50 Hz. Physics in Medicine and Biology, 51(10), 2383–2394.
Cech, R., et al. (2007). Fetal exposure to low frequency electric and magnetic fields. Physics in Medicine and Biology, 52(4), 879–888; Shi, C. Y., & Xu, X. G. (2004). Development of a 30-week-pregnant female tomographic model from computed tomography (CT) images for Monte Carlo organ dose calculations. Medical Physics, 31(9), 2491–2497.
Hand, J. W., et al. (2006). Prediction of specific absorption rate in mother and fetus associated with MRI examinations during pregnancy. Magnetic Resonance in Medicine, 55(4), 883–893; Xu, X. G., et al. (2007). A boundary-representation method for designing whole-body radiation dosimetry models: pregnant females at the ends of three gestational periods--RPI-P3, -P6 and -P9. Physics in Medicine and Biology, 52(23), 7023–7044.
Ackerman, M. J. (1998). The visible human project. Proceedings of the IEEE, 86(3), 504–511.
Ackerman, M. J. (2016). The visible human project®: From body to bits. Orlando: EMBC 2016.
Nagaoka, T., et al. (2015). SAR calculation in semi-homogeneous human models of pregnancy for RF exposure. Asia-Pacific International Symposium on Electromagnetic Compatibility. Taipei, pp. 444–447.
The Virtual Population. (2016, April). High-resolution anatomical models for computational life sciences. IT’IS Foundation/FDA Flyer, European Conference on Antennas and Propagation.
Gosselin, M. C., et al. (2014). Development of a new generation of high-resolution anatomical models for medical device evaluation: The Virtual Population 3.0. Physics in Medicine and Biology, 59(18), 5287–5303.
Nagaoka, T., et al. (2007). An anatomically realistic whole-body pregnant-woman model and specific absorption rates for pregnant-woman exposure to electromagnetic plane waves from 10 MHz to 2 GHz. Physics in Medicine and Biology, 52(22), 6731–6745.
Nagaoka, T., et al. (2008). Estimating specific absorption rates in pregnant women by using models at 12-, 20-, and 26-weeks’ gestation for plane wave exposures. International Symposium on Electromagnetic Compatibility – EMC Europe, Hamburg, pp. 1–4.
Becker, J., et al. (2008). Katja – the 24th week of virtual pregnancy for dosimetric calculations. Polish Journal of Medical Physics and Engineering, 14(1), 13–19.
Christ, A., et al. (2001). The Virtual Family – development of surface-based anatomical models of two adults and two children for dosimetric simulations. Physics in Medicine and Biology, 55(2), 23–38.
Dimbylow, P. J. (2005). Development of the female voxel phantom, NAOMI, and its application to calculations of induced current densities and electric fields from applied low frequency magnetic and electric fields. Physics in Medicine and Biology, 50(6), 1047–1070.
Nagaoka, T., et al. (2004). Development of realistic high resolution whole-body voxel models of Japanese adult male and female of average height and weight, and application of models to radio-frequency electromagnetic-field dosimetry. Physics in Medicine and Biology, 49(1), 1–15.
Starzynski, J., et al. (2002). Simulation of magnetic stimulation of the brain. IEEE Transactions on Magnetics, 38(2), 1237–1240.
Wagner, T. A., et al. (2004). Three-dimensional head model simulation of transcranial magnetic stimulation. IEEE Transactions on Biomedical Engineering, 51(9), 1586–1598.
Wagner, T. A., et al. (2006). Transcranial magnetic stimulation and stroke: A computer-based human model study. NeuroImage, 30(3), 857–870.
Wagner, T. A., et al. (2014). Impact of brain tissue filtering on neurostimulation fields: A modeling study. NeuroImage, 85(3), 1048–1057.
Miranda, P. C., et al. (2003). The electric field induced in the brain by magnetic stimulation: A 3-D finite-element analysis of the effect of tissue heterogeneity and anisotropy. IEEE Transactions on Biomedical Engineering, 50(9), 1074–1085.
Miranda, P. C., et al. (2016). Computational models of non-invasive brain and spinal cord stimulation. EMBC 2016, Orlando.
Wenger, C., et al. (2015). The electric field distribution in the brain during TTFields therapy and its dependence on tissue dielectric properties and anatomy: A computational study. Physics in Medicine and Biology, 60, 7339–7357.
Chen, M., & Mogul, D. J. (2009). A structurally detailed finite element human head model for simulation of transcranial magnetic stimulation. Journal of Neuroscience Methods, 179(1), 111–120.
Opitz, A., et al. (2013). Physiological observations validate finite element models for estimating subject-specific electric field distributions induced by transcranial magnetic stimulation of the human motor cortex. NeuroImage, 81, 253–264.
Bottauscio, O., et al. (2014). Evaluation of electromagnetic phenomena induced by transcranial magnetic stimulation. IEEE Transactions on Magnetics, 50(2), 1033–1036.
Deng, Z. D. (2013). Electromagnetic field modeling of transcranial electric and magnetic stimulation: Targeting, individualization, and safety of convulsive and subconvulsive applications. Ph.D. dissertation, Department of Electrical Engineering, Columbia University, Ithaca, New York.
Lee, W. H. (2014). Noninvasive neuromodulation: Modeling and analysis of transcranial brain stimulation with applications to electric and magnetic seizure therapy. Ph.D. dissertation, Department of Biomedical Engineering, Columbia University, Ithaca, New York.
Yushkevich, P. A., et al. (2016). ITK-SNAP: An interactive tool for semi-automatic segmentation of multi-modality biomedical images. Orlando: EMBC.
Lo, S. H. (1995). Automatic mesh generation over intersecting surfaces. International Journal for Numerical Methods in Engineering, 38, 943–954.
Lo, S. H., & Wang, W. X. (2004). A fast robust algorithm for the intersection of triangulated surfaces. Engineering with Computers, 20, 11–21.
Elsheikh, A. H., & Elsheikh, M. (2014). A reliable triangular mesh intersection algorithm and its application in geological modelling. Engineering with Computers, 30, 143–157.
Coelho, L. C., et al. (2000). Intersecting and trimming parametric meshes on finite-element shells. International Journal for Numerical Methods in Engineering, 47, 777–800.
Lira, W.M., et al. (2002). Multiple intersections of finite-element surface meshes. 11th International Meshing Roundtable, Ithaca, New York.
Lindenbeck, C. H., et al. (2002). TRICUT: A program to clip triangle meshes using the rapid and triangle libraries and the visualization toolkit. Computers & Geosciences, 28, 841–850.
Yanamadala, J., et al. (2014, October 1–5). Segmentation of the visible human project® (VHP) female cryosection images within MATLAB® environment. 23rd International Meshing Roundtable (IMR23), London.
Noetscher, G.M., et al. (2015, October 12–14). VHP-Female v3.0 FEM/BEM computational human phantom. 24th International Meshing Roundtable (IMR24), Austin.
Gammon, M. (2014, October 12–15). CAD clean-up for meshing. What could possibly go wrong?” Short Course. 23rd International Meshing Roundtable, London, pp. 1–70.
Moorcroft, M. D., et al. (2003). Computational model of the pregnant occupant: Predicting the risk of injury in automobile crashes. American Journal of Obstetrics and Gynecology, 189(2), 540–544.
Duma, S.M., et al. (2006). Analysis of pregnant occupant crash exposure and the potential effectiveness of four-point seatbelts in far side crashes. The Proceedings of the 50th Association for the Advancement of Automotive Medicine Conference, 50.
Duma, S.M., et al. (2005). A computational model of the pregnant occupant: Effects of restraint usage and occupant position on fetal injury risk. Proceedings. of the 19th International Conference for the Enhanced Safety Vehicles, Washington, D.C.
Kitagawa, Y., & Yasuki, T. (2010). Development of pregnant FE model and prediction of kinematics in frontal impact. CiNii. [Online]. Available: http://ci.nii.ac.jp/naid/130004515562/.
Gabriel, C., & Gabriel, S. (1997). Compilation of the dielectric properties of body tissues at RF and microwave frequencies. [Online]. Available: http://niremf.ifac.cnr.it/docs/DIELECTRIC/Report.html.
Hasgall, P. A., et al. (2015). IT’IS Database for thermal and electromagnetic parameters of biological tissues. In Version 2.6, January 13th. www.itis.ethz.ch/database.
Schepps, J. L., & Foster, K. R. (1980). The UHF and microwave dielectric properties of normal and tumour tissues: Variation in dielectric properties with tissue water content. Physics in Medicine and Biology, 25, 1149–1159.
Peterchev, A. V., et al. (2008). A transcranial magnetic stimulator inducing near-rectangular pulses with controllable pulse width (cTMS). IEEE Transactions on Biomedical Engineering, 55(1), 257–266.
Thielscher, A. Transcranial magnetic stimulation [Online], Available: ftp://ftp.kyb.mpg.de/kyb/chaimow/For%20Me/TMS/Thielscher_Lecture_Session1.pdf
Peterchev, A. V., et al. (2011). Repetitive transcranial magnetic stimulator with controllable pulse parameters. Journal of Neural Engineering, 8(3), 1–24.
Peterchev, A. V., et al. (2014). Controllable pulse parameter transcranial magnetic stimulator with enhanced circuit topology and pulse shaping. Journal of Neural Engineering, 11(5), 1–12.
Brainsway Deep TMS System, Brainsway Ltd., Jerusalem, Israel, 2013, pp. 5–8.
MAGSTIM 2002 P/N 3001-23-04, The Magstim Company Ltd., Whitland SA34 0HR, United Kingdom, 2005, pp. 27–28.
MagVita TMS Therapy System, Tonica Elektronik A/S, Farum, Denmark, 2015, pp. 5–4.
NeuroStar TMS Therapy System, Neuronetics, Inc., Malvern, PA, 2014, pp. 1–30.
Makarov, S. N., et al. (2016). Preliminary upper estimate of peak currents in transcranial magnetic stimulation at distant locations from a TMS coil. IEEE Transactions on Biomedical Engineering, 63(9), 1944–1955.
Epstein, C. M., et al. (2008). The Oxford handbook of transcranial stimulation. New York: Oxford University Press.
Guidance for Industry and Food and Drug Administration Staff. (2011, July 26). Class II Special Controls Guidance Document: Repetitive Transcranial Magnetic Stimulation (rTMS) Systems. Center for Devices and Radiological Health, FDA.
Herbsman, T., et al. (2009). Motor threshold in transcranial magnetic stimulation: the impact of white matter Fiber orientation and skull-to-cortex distance. Human Brain Mapping, 30(7), 2044–2055.
Makarov, S. N., et al. (2015). Modeling of low frequency electromagnetic fields in electrical and biological systems. New York: Wiley.
Pearlstein, T. (2008). Perinatal depression: Treatment options and dilemmas. Journal of Psychiatry & Neuroscience, 33(4), 302–318.
Divya, M. P., et al. (2016). Depression in pregnancy-consequences and treatment modalities. International Journal of Pharmacy and Pharmaceutical Sciences, 8(3).
Acknowledgements
The authors thank Dr. Gregory Noetscher, Mr. Matthew W. Piazza, Ms. Tsering Dolma, Ms. Mariya Zagalskaya, Mr. Edward Burnham, Mr. Harshal Tankaria, Mr. Goutham Kodumudi Srichandhru, Mr. Anh Le Tran, and Mr. David Kelly, all of Worcester Polytechnic Inst., MA for their help in development and improvement of the pregnant female CAD computational human model and in performing multiple simulations in ANSYS Maxwell 3D. The authors also thank Dr. Swarnalatha Gummadi of St. Vincent De Paul Hospital, Thrissur, India, for her feedback in the development of the pregnant models.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Japanese Virtual Model (JVM) Finite-Element Model Version 1.1 (6 months)
Japanese Virtual Model (JVM) Finite-Element Model Version 1.1 (6 months)
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2019 The Author(s)
About this chapter
Cite this chapter
Yanamadala, J., Borwankar, R., Makarov, S., Pascual-Leone, A. (2019). Estimates of Peak Electric Fields Induced by Transcranial Magnetic Stimulation in Pregnant Women as Patients or Operators Using an FEM Full-Body Model. In: Makarov, S., Horner, M., Noetscher, G. (eds) Brain and Human Body Modeling. Springer, Cham. https://doi.org/10.1007/978-3-030-21293-3_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-21293-3_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-21292-6
Online ISBN: 978-3-030-21293-3
eBook Packages: EngineeringEngineering (R0)