Abstract
Optimal vascular access insertion and management requires clinicians to have appropriate education and skill on the best procedural techniques or be supervised during the process of acquiring the necessary education. The second quadrant of the Vessel Health and Preservation (VHP) model requires a qualified inserter, a clinician who has undertaken a comprehensive clinical and vascular assessment and is applying the latest evidence and guidelines to select the most appropriate device for patient treatment, leading to the successful insertion of a peripheral or central VAD. Appropriate device selection and number of necessary lumens are a determination made according to lowest risk for patient insertion and potential for infection, in conjunction with the needs of the therapy. Selection of the best vascular access for the patient also requires an understanding of the most appropriate intravascular device to be used, influenced by infusate characteristics to be administered and the length of anticipated dwell, which in turn, influences the most appropriate vessel and anatomical position for device placement.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- VAD training
- VAD education
- Training requirements
- Core competencies for validation
- Training recommendations
- Simulation training
- Checklists
- Rating scales
1 Introduction
Insertion of the right device and the right inserter encompass the second stage of the VHP process. Selection of the inserter and application of infection prevention principles are contributing factors for patient safety. Vascular access specialists and teams’ function to aid in selection and insertion of the most appropriate device. Ensuring the insertion is performed by a trained and qualified clinician with ultrasound skills reduces insertion and post insertional complications. The training, education and competency necessary to become a qualified VAD inserter are discussed throughout the rest of this chapter.
2 The Need for Adequate Education
Insertion of IV devices is a highly technical, high-risk procedure with greater risk to patients when CVADs are inserted and used (Chopra et al. 2015). The successful insertion of vascular devices relies on clinician expertise which is determined by training, credentialing and procedural volume. Historically, clinical expertise was seen as synonymous with the medical profession. Technically advanced vascular access such as central venous catheter (CVC) placement was the domain of the medical practitioner. However, clinical practice is continuously evolving; patient complexity, technology and hospital workload demands have spurred new clinical subspecialties that are changing the boundaries of traditional clinical work, where the medical practitioner is not necessarily at the centre of all clinical procedures (Dowling et al. 1995; Williams et al. 1997; Alexandrou et al. 2010).
According to the US Food and Drug Administration (FDA) in a survey of 1988 and subsequent investigations by a Central Venous Catheter Working group, over 55% of all vascular access-related complications were attributable to healthcare workers (Scott 1988). Whilst these data are dated, this investigation indicated lack of training and validation of competency as a direct cause of complications. In current literature, this concept of training and validation is illustrated in both newer ultrasound practices and with infection reduction methods (Primdahl et al. 2016; Rusche et al. 2001). Insufficient understanding of evidence-based assessment, selection, insertion and management of peripheral and central venous access devices leaves the patient at risk for more serious complications and the added trauma associated with frequent replacement of catheters (Rickard et al. 2013).
Comprehensive education on VAD insertion including competency assessment has shown to reduce procedural complications in comparison to minimal or no education (Alsaad et al. 2017; Evans et al. 2010; Sherertz et al. 2000). Procedural load plays a significant role in successful vascular device insertion, and the number of devices placed is a known modifiable risk factor (Alexandrou et al. 2014; Eisen et al. 2006; Sherertz et al. 2000). The number of devices placed can increase clinician experience and confidence. Studies have reported that experienced CVAD inserters who have inserted more than 50 catheters have half the complication rate of CVAD inserters who have inserted less than 50 catheters (McGee and Gould 2003).
Inadequate training and education on vascular access theory and techniques can expose patients to unnecessary iatrogenic complications (Alexandrou et al. 2010; Castro-Sánchez et al. 2014; Scott 1988). The insertion of central venous access devices (CVADs) by operators with minimal experience or supervision can pose significant risk to patient safety (Alexandrou et al. 2010, 2014; Hamilton 2005). Serious adverse outcomes have been reported from procedural complications related to CVAD insertion that have contributed to patient morbidity and mortality (Carr et al. 2018). These complications can include mechanical and infectious complications as well as thrombotic complications (McGee and Gould 2003). The most critical insertion-related complications include pneumothorax, nerve damage and major artery puncture and may occur in up to one in six catheter insertions (Eisen et al. 2006; Taylor and Palagiri 2007). Patients with previous cannulation attempts, history of surgery at the site of proposed cannulation, obesity and a lack of operator expertise have all been documented as influencing factors for CVAD insertion complication risk (Nayeemuddin et al. 2013).
The right education and training in VAD insertion have a positive impact on reducing central line-associated bloodstream infectious complications (Coopersmith et al. 2002; Sherertz et al. 2000). The primary goal of VHP is to reduce risk associated with the insertion and management of VADs; this can be achieved through infection prevention education. The Centers for Disease Control (CDC) endorse education as a necessary component of infection prevention (O’Grady et al. 2011). Additionally, the CDC recommends that education by specialist teams results in the best outcomes for CVAD insertion and management. An increased risk of device infection is associated with unskilled, inexperienced or unqualified inserters. Successful insertion of VADs relies on operator knowledge, expertise and application of evidence-based guidelines shown to reduce complications (Babu et al. 2016; Mourad et al. 2010).
There has been significant improvement in the health outcomes of patients in recent decades, most notably through the advancements in technology and evidenced-based treatment (Loveday et al. 2014; Teramoto et al. 2017). In contrast, the increasing complexity of patient comorbidity and specialised procedural skills required to treat such patients has also attributed to adverse procedural outcomes and a need for more training (Barach and Johnson 2006; Pronovost et al. 2002). Vascular access device (VAD) placement is one such procedural skill that has become an essential component to many therapies yet carries risks which can lead to serious adverse patient outcomes contributing to morbidity and mortality (Eisen et al. 2006; McGee and Gould 2003; Miliani et al. 2017).
3 The Right Education: Insertion Training
It is worth recognising that people learn in different ways, and having some understanding of these concepts will allow the educator to plan the most effective way to assist learning (Taylor and Hamdy 2013). Significance of patient safety and fairness to novice clinicians has seen the paradigm of “see one, do one, teach one” evolve significantly into models of required educational components for CVAD placement (Davidson et al. 2012; Lenchus 2010; Moureau et al. 2013; Rodriguez-Paz et al. 2009). It is clear that standardized, structured approaches incorporating education, supervision and simulation to teach procedures improve knowledge and skill acquisition, increase learner confidence and reduce complications in clinical practice (Herrmann-Werner et al. 2013).
Comprehensive vascular access training should consist of didactic lectures, skills acquisition in a simulated environment and supervised application with patient insertions (Marschall et al. 2014; Troianos et al. 2011). Competency assessment in VAD insertion in a simulated environment before patient insertion should be a basic patient safety goal in every healthcare facility (Davidson et al. 2012). It is still not uncommon, however, for trainees to undertake invasive procedures with minimum or no supervision as is the case with many ultrasound-guided peripheral catheter insertions. It is also not uncommon for supervisors to be junior and inexperienced with risk mitigating strategies (Lenhard et al. 2008). All of these factors contribute to or reduce the level of risk for the patient requiring vascular access insertion and management.
4 Right Education for PIVC Success
Successfully inserting a PIVC on the first attempt preserves veins and enhances the concept of vessel health and preservation. This immediate success with insertion can impact patient wellbeing and experience, in addition to the probability of concluding treatment without complication. Insertion success and lack of complications are influenced by a variety of clinical variables and include clinician, patient-specific, products and technology as well as ergonomic and environmental factors (Carr et al. 2016a; Chopra et al. 2012).
Many international clinical guidelines include recommendations for various aspects of PIVC insertion and care (Gorski et al. 2016; Loveday et al. 2014; O’Grady et al. 2011). Despite such guidance, PIVC insertion can be difficult (Riker et al. 2011; van Loon et al. 2016; Yen et al. 2008), time consuming, anxiety producing (Dougherty and Lamb 2014) and painful for the patient (Fields et al. 2014). Clinicians are required to be competent (and in some cases, certified) to perform a range of functions regarding the insertion of a PIVC that include assessment of the potential insertion site, proficiency with the insertion procedure and ability to maintain the device post insertion and perform surveillance to detect complications or loss of function (Moureau et al. 2013; Moureau 2017).
Studies report wide-ranging variability of first-time insertion success: between 2 and 81%. Patients may be subjected to two or more attempts when a traditional landmark/palpation-guided insertion approach is used (Aulagnier et al. 2014; Carr et al. 2010; Witting 2012). The use of ultrasound to guide insertion may improve these rates, but as yet, ultrasound is inconsistently used for PIVC insertions. Given the variability in first-time insertion success, there is an opportunity to address this clinical phenomenon and improve outcomes for patients.
The literature suggests some patient factors that increase the risk of insertion failure (Carr et al. 2016b; Fields et al. 2014; Maki and Ringer 1991; Sebbane et al. 2013). Failure within this literature base is attributed to the skill of the inserter; experience and knowledge of ultrasound; catheter length and amount within the vein, depth and size of the vein; ability to guide needle and catheter deeply into the vein; and various patient factors. However, there has been little research on how these risk factors can then potentially be used to assess the degree of insertion difficulty, i.e. the likelihood of PIVC insertion success prior to insertion. Such guidance would be useful in identifying high-risk patients to target with interventions that may prevent insertion failure. The VHP framework incorporates the peripheral vein visual inspection process, identifying anticipated levels of difficulty by the condition of veins (Hallam et al. 2016).
Avoiding scheduled PIVC insertions and opting for clinically indicated removal have been predicted to save tens of millions of dollars for facilities each year (Tuffaha et al. 2014). Furthermore, considering the patient experience and satisfaction with care, improving the patient journey with better vascular access protocols should be a priority for hospital administrators (Moureau et al. 2012). Achieving greater first-time insertion success in addition to increasing the functional dwell time of inserted PIVCs through a standardised vascular access bundle could potentially support such an endeavour, saving money and impacting positively on the patient experience (Cooke et al. 2018; Larsen et al. 2017). In addition, capturing relevant insertion and post insertion data points prospectively in a digital first strategy through a clinical database could conceivably answer a variety of clinical questions and inform local hospitals of their baseline and continuous data points (Davis 2011).
Given that documentation of PIVCs is often not percieved as a clinical concern (Castro-Sánchez et al. 2014), when outcomes are poorly recorded in the medical chart or computer record, greater emphasis is required to stress the usefulness of vascular access data recording. Such a concept, when underpinned by VHP, could revolutionise the decision-making for vascular access science in addition to contributing to a continuous data cycle to inform hospitals of actual and potential outcomes.
5 Approaches to Training
Depending on available resources, an online web-based approach to training may serve to replace or support traditional face-to-face educational lectures and has been proven as an acceptable alternative (Chenkin et al. 2008; Moureau et al. 2013). Online training is potentially advantageous in that it can be standardised and accessible almost anywhere, at any time. Incorporating video as a tool to demonstrate procedures and techniques has been a common inclusion within successful programmes (Evans et al. 2010; Nguyen et al. 2014).
Simulation-based training for teaching procedures is shown to improve skill acquisition, increase learner confidence and reduce complications in clinical practice (Hirvela et al. 2000). Simulators used in vascular access training range from highly technical interactive mannequins, to partial task trainers replicating anatomical structures and to simulators incorporating virtual reality. Whilst equipment like this can be expensive, effective high-fidelity phantoms may be produced with readily accessible items such as poultry breasts fitted with drains for comparatively little cost (Loukas et al. 2011; Moureau et al. 2013; Rippey et al. 2015).
Approaches to training should be based on a curriculum that clearly defines the cognitive knowledge and technical skill required to undertake ultrasound-guided vascular access (Schmidt and Kory 2014; Troianos et al. 2011). An international evidence-based consensus task force established through the World Congress of Vascular Access recommends 6–8 h of didactic education, 4 h hands-on training on inanimate models and 6 h hands-on training on normal human volunteers for appreciation of normal ultrasound anatomy (Moureau et al. 2013). Training is then followed by supervised insertions, guided by experienced clinicians giving feedback for improvement. The number of procedures required to achieve competence in real-time ultrasound-guided vascular access is unspecified due to the variables in knowledge and skill acquisition between individuals (Moureau et al. 2013; Troianos et al. 2011).
Technical performance in vascular access is typically assessed using checklists or global rating scales. Procedures in vascular access are generally comprised of a number of sequential steps, thus making assessment possible using a checklist (Moureau et al. 2013). Although global rating scales can be contentious, they can be a better indicator of procedural competency compared to checklist assessment (Ma et al. 2012; Moureau et al. 2013). Clinicians performing high-risk procedures such as vascular access insertions require periodic competency assessment, determined by each facility, but recommended as part of annual or biennial credentialing.
The following sections reflect core competencies necessary for undertaking catheter insertion safely based on the VHP philosophy and minimal training requirements (Moureau et al. 2013):
-
1.
Anatomy and physiology of relevant body systems
-
2.
Ultrasound for insertion and assessment
-
3.
Central venous device tip location
-
4.
Infection control and ANTT
-
5.
Device selection and indications
-
6.
Insertion procedures, complication prevention, evaluation and management
-
7.
Care and maintenance practices along with needle-free connectors and securement devices
-
8.
Qualification and competency
-
9.
Simulation training
-
10.
Anatomical models
-
11.
Objective grading and proficiency
-
12.
Examination and competency
-
13.
Supervised instruction
-
14.
Didactic or web-based training
-
15.
Developing clinical competence
-
16.
Education for children and neonates
5.1 Anatomy and Physiology
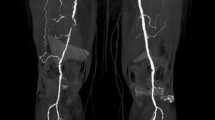
A working knowledge of anatomy and physiology is essential for those undertaking vascular access procedures to minimise complications (Bannon et al. 2011; Moureau et al. 2013). Traditionally, it was the presumed location of a blood vessel, the correlation between surface anatomical landmarks and deep anatomical structures that would guide percutaneously inserted VAD (Bannon et al. 2011). Ultrasound guidance is advantageous in that it provides an “inside view” of deep anatomical structures but requires anatomical knowledge to manipulate both transducer and insertion needle avoiding complications from cannulation of incorrect vessels (Bannon et al. 2011; Troianos et al. 2011). Understanding both normal and variant anatomies enables clinicians to safely complete procedures and identify complications such as misplaced catheters should they occur (Bannon et al. 2011; Moureau et al. 2013).
5.2 Use of Ultrasound
Ultrasound for vascular access is not a new concept and has been used in clinical practice for decades. Over time ultrasound has become widely accepted as a means to improve procedural success rates and reduce associated complications and is now included in many practice guidelines (Moore 2014; Moureau et al. 2013; Troianos et al. 2011). Notwithstanding a multitude of evidence showing the benefit of using ultrasound guidance for vascular access, success is not guaranteed through mere placement of a transducer on the patient (Lamperti et al. 2012; Moore 2014). The clinician must have an understanding of ultrasound physics, mechanisms of image acquisition and optimization and artefacts and ultimately be able to interpret 2D images representing 3D anatomical structures. When novice clinicians first begin to practise using ultrasound and align the ultrasound probe and the needle over the vein of the phantom, it is common to see the probe moving to the side, in the direction that the clinician’s head turns. When using ultrasound, the ultrasound screen should be placed directly in front of the clinician so that only a glance ahead to look at the screen is needed; this placement reduces sideways movement of the probe. Additionally, there are required practical aspects that include hand-eye coordination and manual dexterity to allow manipulation of the transducer and needle according to what is being viewed on the image display (Moureau et al. 2013; Troianos et al. 2011).
To derive the maximum advantage using ultrasound, real-time guidance for vessel access must be preceded by vascular assessment with ultrasound. Ultrasound assessment of vessels allows one to establish the best site for insertion, ensuring the right vessel is chosen, accounting for size, patency and risk minimisation as was discussed in previous chapters. These factors taken together emphasise the need to understand the theory of Virchow’s triad and the effects of catheter to vessel ratio. Ultrasound enables placement and management of VADs for difficult access patients, those morbidly obese, intravenous drug users and other chronically ill patients with limited access. Being a user-dependent technology, specific education and training are required for successful implementation into practice (Lamperti et al. 2012; Moureau et al. 2013; Troianos et al. 2011).
Ultrasound, as an aid to vascular assessment and needle guidance, results in greater success and fewer complications than blind or landmark insertions for both peripheral cannula and central venous catheter insertions (Chinnock et al. 2007; Mahler et al. 2010). Patients with poor vasculature, difficult-to-access peripheral veins and comorbidities that inhibit cannula insertion require technology to reduce the number of attempts required to gain access (Sou et al. 2017). For central venous catheters, GAVeCeLT (Italian Group for Venous Access Devices) recommended the use of US during CVC insertions for six different purposes: (1) US evaluation of all veins available, (2) choice of the vein on the basis of rational US-based criteria, (3) real-time US-guided venipuncture, (4) US-based control of guidewire/catheter orientation during the procedure, (5) US-based control of pleura-pulmonary integrity after axillary or subclavian vein puncture and (6) transthoracic echocardiography for verification of the position of the tip of the catheter at the end of the procedure. Ultrasound, when training and competency is provided, has demonstrated reduced time required to obtain access, greater first-attempt success and increased patient satisfaction (Bauman et al. 2009; Costantino et al. 2005; Mills et al. 2007; Stein et al. 2009; White et al. 2010; Woo et al. 2009).
Doctors and nurses alike have begun to use ultrasound for peripheral and central access of veins. With training specific to ultrasound-guided peripheral cannulae (USGPIV) access, publications support education of 0–3 h and supervised insertions of 0–25 insertions (Blaivas and Lyon 2006; Rose and Norbutas 2008; Schoenfeld et al. 2011; Stein et al. 2009; White et al. 2010; Witting et al. 2010). The literature reflects an increased number of insertion attempts associated with USGPIV when minimal training is received: 6–10 attempts in 3 publications with varying success levels from 0 to 100% (Miles et al. 2012; Stein et al. 2009; Sou et al. 2017). Following USGPIV insertion, failure rates vary within 1 and 24 h and often reflect shorter dwell time than traditionally placed peripheral cannula (Dargin et al. 2010; Keyes et al. 1999; Miles et al. 2015). Education and supervision provided prior to novice attempts coupled with longer catheters and Seldinger-wired insertions report higher success and longer cannula dwell with fewer complications that result in cannula failure (Elia et al. 2012; Harvey and Cave 2011; Mahler et al. 2010). Validation of competency by a supervisor for 5–15 attempts following training resulted in fewer attempts and reduced complications (Adhikari et al. 2010; Moore 2013; Schoenfeld et al. 2011; White et al. 2010).
5.3 Catheter Tip Position
Insertion site selection and final catheter tip position are both influential factors in the incidence of catheter-related complications (Gorski et al. 2016; Loveday et al. 2014). A well-placed centrally inserted device should have its tip reside deep in the SVC, ideally at the cavo-atrial junction (CAJ). Such placement permits parallel positioning of the device to the vessel wall in an area of high blood flow (Babu et al. 2016; Moureau et al. 2013). Catheter tips located in more cephalad regions of the SVC are associated with an increased risk of thrombotic complications (Luciani et al. 2001; Moureau 2013a). Clinicians should be mindful that catheters are subject to movement associated with patient position and respiration and consider this at the time of insertion to ensure optimal tip placement (Babu et al. 2016; Forauer and Alonzo 2000).
5.4 Infection Prevention
A working knowledge of infection prevention practices for device insertion is a critical training requirement. Breaching a patient’s skin to obtain vascular access carries inherent risks including the possibility of infection. Catheter-related bloodstream infection (CRBSI) is a serious, potentially life-threatening complication associated with central venous access device insertion and management. CRBSI can stem from extra-luminal contamination, where organisms migrate from the point of insertion to the catheter, to intraluminal contamination involving direct transfer of organisms to the catheter hub, and contamination may also occur via haematogenous seeding of organisms from other infected sites (Loveday et al. 2014; Moureau 2014; O’Grady et al. 2011). CRBSI contributes to morbidity and mortality as well as burdening healthcare institutions with significant financial costs and increased length of stay as noted in the guidelines. Additional information on infection prevention is provided in subsequent chapters.
5.5 Insertion Technique
Education on insertion of intravenous devices covers direct puncture, Seldinger and modified Seldinger techniques, with incorporation of ultrasound to provide a greater degree of safety, and application of sterile practices with maximal barrier precautions specific to CVAD insertions. Knowledge of procedures specific to each product is part of the educational process in keeping with manufacturer instructions for use. In the chapters that follow, additional details of device insertion, post insertion management and device maintenance are provided for both adults and children.
6 Insertion and Post Insertion Bundles
Once the vascular access device is inserted, the challenge is to maintain it, avoiding failure and complication. Ensuring the VAD does not succumb to failure is a clinical concern as this can lead to a disruption in treatment. Various assessment tools exist to assess VAD failure but are heavily focused on infection or phlebitis as the precursor to infection (Carr et al. 2017). One of the largest clinical observational studies on PIVC has pragmatically classified PIVC failure into three types: (1) infective/phlebitis, (2) occlusion/infiltration and (3) accidental dislodgement (Marsh et al. 2018). In the adult population, it is recognised that at least 25–69% of PIVCs fail before the end of treatment from complications such as occlusion, phlebitis, dislodgement, infection and infiltration (Marsh et al. 2018; Wallis et al. 2014). Device failure can lead to a reduced therapeutic effect of prescribed medicines and an increased length of hospital stay, thus interrupting the patient care processes and clinical pathways (Barton et al. 1998). Complications can be painful and even lead to nerve injury and disability (Stevens et al. 2012). Whilst research has focused on post insertion interventions to avoid failure, there has been little evidence on the link between insertion procedural aspects and future device failure.
Evidence-based recommendations for vascular access procedures and ongoing care and maintenance of devices are abundant in the literature (Chan et al. 2015; Entesari-Tatafi et al. 2015). The use of checklists or “bundles” that record compliance with Surgical-ANTT and infection prevention practices can reduce catheter-associated bloodstream infection (CABSI) (Collaborative 2011; Pronovost et al. 2006). Bundles focus on grouping key principles of practice designed to limit procedural risk and mitigate complications and therefore improve patient care (Collaborative 2011; Moureau 2013b; Pronovost et al. 2006). A collaborative quality improvement project in intensive care units (ICUs) to promote aseptic insertion of central venous lines (CVADs) was performed to identify specific educational needs. A checklist was used to record compliance with all aspects of aseptic CVAD insertion, with maximal sterile barrier precautions for clinicians (“clinician bundle”) and patients (“patient bundle”). Central line-associated bloodstream infections (CLABSI) were identified and reported using a standard surveillance definition. Many ICUs were found lacking in the organisation and staff to support quality improvement and audit. Results demonstrated that compliance with all aspects of aseptic CVAD insertion significantly reduces the risk of CRBSI.
Developing any PIVC insertion bundle requires a stepped process: firstly, to identify the appropriate variables and, secondly, to identify the risk factors for insertion failure. From these, arguments can be made for appropriate device placement. If we assume the data collection strategy includes specific clinician data points, then assumptions on the right clinician can occur. Once evaluated for validity, reliability, clinical utility, clinical acceptability and usability, widespread formal implementation can occur.
Despite the evolution of insertion bundles, better methodological standardised definitions of what constitutes the right device, what ensures insertion success and what reduces post insertion complications will improve the current paucity of high-level evidence for this area of vascular access science. Application of insertion bundles may be enhanced when specialty teams are involved with insertion and care of VADs.
Previous examples of framework or clinical decision strategies, such as bundles and specialised teams for vascular access, have evidenced improved patient experiences with appropriate device placement resulting in longer device function to the end of treatment and reduced length of hospital stay (Barton et al. 1998). However, this approach lacks robust analysis and validation, and evidence is almost 20 years old where replication studies to support these data have not been found. Ideally, prospective and clinically relevant data from a patient group make it generalizable to that population (Hendriksen et al. 2013).
The widely recognised study conducted out of Michigan, known as the Keystone ICU project, tested the impact on CRBSI, the bundle approach for insertion of CVADs with five key interventions in intensive care units: hand hygiene, selection of the lowest risk device for the treatment, skin disinfection with alcoholic chlorhexidine, maximum sterile barriers and procedure for CVAD insertion and evaluation for device necessity daily (Pronovost et al. 2006). Each of the interventions was an evidence-based recommendation of the Center for Disease Control (CDC). The study demonstrated significant reduction of CRBSI across all participating ICUs based on the group of interventions (O’Grady et al. 2011; Pronovost et al. 2006).
Post insertion, devices are accessed frequently for the purposes of administering and monitoring treatment, and each access presents an opportunity for microorganisms to be introduced into the bloodstream (The Joint Commission 2013). It must be acknowledged that poor application of post insertion care often results in complications including device failure and infection (Davis 2011; O’Grady et al. 2011; Wallis et al. 2014). The bundled approach (Table 4.1) has been proven to reduce the rate of CRBSI primarily by the maintenance of sterility during the insertion phase (Burrell et al. 2011; Moureau 2013a).
Bundles are used in a variety of acute specialties and can assist the clinician in improving the safety and quality of healthcare delivery and thus improve clinical and patient outcomes. Defined by the Institute of Healthcare Improvement as “a group of interventions related to a disease process that, when executed together, results in better outcomes than when implemented individually” and a “structured way of improving care processes and patient outcomes, a small, straightforward set of evidence-based practices—generally three to five—that, when performed collectively and reliably, have been proven to improve patient outcomes”.
Examples of bundles of care include the Institute for Healthcare Improvement’s 5 Million Lives Campaign (McCannon et al. 2007) for central venous catheter and ventilator bundles and severe sepsis bundle (Levy et al. 2010). In the absence of an appropriate service delivery for vascular access (i.e. vascular access specialist team), bundles of care for vascular access aim to improve outcomes by promoting best evidence-based interventions. Ideally the components are based on Level 1 evidence, and each component must be performed at point of care.
Is the PIVC clinically indicated? The vascular access literature reveals evidence of inappropriate device selection and one bundle component that, in the pre-insertion phase may be suggested, is a component which asks, is this device clinically indicated or not? (Chopra et al. 2015; Ricard et al. 2013). Examples for PICCs include the MAGIC calculator and app for appropriate PICC use (Michigan MAGIC, www.improvepicc.com). Recently, a systematic scoping review on tools, rules and algorithms for approaches to PIVC insertion identified that few well-validated, reliable tools exist for PIVC insertion, but this is perhaps owing to the variety of clinical disciplines which perform PIVCs (Carr et al. 2017).
Admittedly, VHP could be accused of not being evidence based; however, it is a conceptual framework that underpins a series of relationships with vascular access, similar to the bundle approach, and, as a result, is available for adoption and validation. Equally, there are gaps, or rather opportunities, to develop bundles of care for vascular access that will enhance the concepts of the VHP framework. Ideally, any bundle should represent insertion and post insertional phases of the vascular access device and alert healthcare professionals when clinical concerns occur. This means pre-insertion, insertion and post insertion bundles must be aware of the clinical symptoms that may occur which demand further critique and common sense considerations.
Case Study
A 178 kg female was admitted to acute care with gastritis, nausea and vomiting. Unable to initiate PIVC, a specialist was contacted. An ultrasound-guided PIVC was placed for medication administration. Following the insertion, the laboratory verified an appendicitis and the need for more reliable access for surgery. The vascular access specialist, also trained for midline placement, inserted a midline in the cephalic vein of the right arm.
Summary of Key Points
-
1.
Patients have the right to the most qualified inserter for every insertion.
-
2.
Inserters with training, experience and verified competency have the lowest rate of complications.
-
3.
Minimal education and training requirements are necessary for clinicians who insert central venous access devices (Moureau et al. 2013).
-
4.
Competency assessment is a measure of performance necessary to ensure safe practice and should be performed initially and at scheduled intervals.
References
Adhikari S, Blaivas M, Morrison D, Lander L. Comparison of infection rates among ultrasound-guided versus traditionally placed peripheral intravenous lines. J Ultrasound Med. 2010;29(5):741–7.
Alexandrou E, Spencer TR, Frost SA, Parr MJ, Davidson PM, Hillman KM. A review of the nursing role in central venous cannulation: implications for practice policy and research. J Clin Nurs. 2010;19(11–12):1485–94.
Alexandrou E, Spencer T, Frost S, Mifflin N, Davidson P, Hillman K. Central venous catheter placement by advanced practice nurses demonstrates low procedural complication and infection rates—a report from 13 years service. Crit Care Med. 2014;42(3):536–43. https://doi.org/10.1097/CCM.0b013e3182a667f0.
Alsaad AA, Bhide VY, Moss JL Jr, Silvers SM, Johnson MM, Maniaci MJ. Central line proficiency test outcomes after simulation training versus traditional training to competence. Ann Am Thorac Soc. 2017;14(4):550–4.
Aulagnier J, Hoc C, Mathieu E, Dreyfus JF, Fischler M, Guen M. Efficacy of AccuVein to facilitate peripheral intravenous placement in adults presenting to an emergency department: a randomized clinical trial. Acad Emerg Med. 2014;21(8):858–63.
Babu S, Bennett J, Binks R, Fee P, Fox B, Johnston A, et al. Association of Anaesthetists of Great Britain and Ireland: safe vascular access 2016. Anaesthesia. 2016;71(5):573–85.
Bannon MP, Heller SF, Rivera M. Anatomic considerations for central venous cannulation. Risk Manag Healthc Policy. 2011;4:27.
Barach P, Johnson J. Understanding the complexity of redesigning care around the clinical microsystem. Qual Saf Health Care. 2006;15(Suppl 1):i10–6.
Barton A, Danek G, Johns P, Coons M. Improving patient outcomes through CQI: vascular access planning (the clinical impact of cost reduction). J Nurs Care Qual. 1998;13(2):77–85.
Bauman M, Braude D, Crandall C. Ultrasound-guidance vs. standard technique in difficult vascular access patients by ED technicians. Am J Emerg Med. 2009;27(2):135–40. https://doi.org/10.1016/j.ajem.2008.02.005.
Blaivas M, Lyon M. The effect of ultrasound guidance on the perceived difficulty of emergency nurse-obtained peripheral IV access. J Emerg Med. 2006;31(4):407–10. https://doi.org/10.1016/j.jemermed.2006.04.014.
Burrell A, McLaws M, Murgo M, Calabria E, Pantle A, Herkes R. Aseptic insertion of central venous lines to reduce bacteraemia. Med J Aust. 2011;194(11):583–7.
Carr PJ, Glynn RW, Dineen B, Kropmans TJ. A pilot intravenous cannulation team: an Irish perspective. Br J Nurs. 2010;19(Suppl 10):S19–27.
Carr PJ, Higgins NS, Cooke ML, Mihala G, Rickard CM. Vascular access specialist teams for device insertion and prevention of failure. Cochrane Database Syst Rev. 2018;(3).
Carr PJ, Rippey JC, Budgeon CA, Cooke ML, Higgins N, Rickard CM. Insertion of peripheral intravenous cannulae in the emergency department: factors associated with first-time insertion success. J Vasc Access. 2016a;17(2):182–90.
Carr PJ, Rippey JC, Cooke ML, Bharat C, Murray K, Higgins NS, et al. Development of a clinical prediction rule to improve peripheral intravenous cannulae first attempt success in the emergency department and reduce post insertion failure rates: the Vascular Access Decisions in the Emergency Room (VADER) study protocol. BMJ Open. 2016b;6(2):e009196.
Carr PJ, Higgins NS, Rippey J, Cooke ML, Rickard CM. Tools, clinical prediction rules, and algorithms for the insertion of peripheral intravenous catheters in adult hospitalized patients: a systematic scoping review of literature. J Hosp Med. 2017;12(10):851–8.
Castro-Sánchez E, Charani E, Drumright LN, Sevdalis N, Shah N, Holmes AH. Fragmentation of care threatens patient safety in peripheral vascular catheter management in acute care—a qualitative study. PLoS One. 2014;9(1):e86167. https://doi.org/10.1371/journal.pone.0086167.
Chan M-C, Chang C-M, Chiu Y-H, Huang T-F, Wang C-C. Effectiveness analysis of cross-functional team to implement central venous catheter care bundle. J Microbiol Immunol Infect. 2015;48(2):S90.
Chenkin J, Lee S, Huynh T, Bandiera G. Procedures can be learned on the web: a randomized study of ultrasound-guided vascular access training. Acad Emerg Med. 2008;15(10):949–54.
Chinnock B, Thornton S, Hendey GW. Predictors of success in nurse-performed ultrasound-guided cannulation. J Emerg Med. 2007;33(4):401–5. https://doi.org/10.1016/j.jemermed.2007.02.027.
Chopra V, Anand S, Krein S, Chenoweth C, Saint S. Bloodstream infection, venous thrombosis, and peripherally inserted central catheters: reappraising the evidence. Am J Med. 2012;125(8):733–41. https://doi.org/10.1016/j.amjmed.2012.04.010.
Chopra V, Flanders S, Saint S, Woller S, O’Grady N, Safdar N, et al. The Michigan Appropriateness Guide for Intravenous Catheters (MAGIC): results from a multispecialty panel using the RAND/UCLA appropriateness method. Ann Intern Med. 2015;163(6 Suppl):S1–40. https://doi.org/10.7326/M15-0744.
Collaborative N. Aseptic insertion of central venous lines to reduce bacteraemia. Med J Aust. 2011;194(11):583–7.
Cooke M, Ullman AJ, Ray-Barruel G, Wallis M, Corley A, Rickard CM. Not “just” an intravenous line: consumer perspectives on peripheral intravenous cannulation (PIVC). An international cross-sectional survey of 25 countries. PLoS One. 2018;13(2):e0193436.
Coopersmith CM, Rebmann TL, Zack JE, Ward MR, Corcoran RM, Schallom ME, et al. Effect of an education program on decreasing catheter-related bloodstream infections in the surgical intensive care unit. Crit Care Med. 2002;30(1):59–64.
Costantino TG, Parikh AK, Satz WA, Fojtik JP. Ultrasonography-guided peripheral intravenous access versus traditional approaches in patients with difficult intravenous access. Ann Emerg Med. 2005;46(5):456–61. https://doi.org/10.1016/j.annemergmed.2004.12.026.
Dargin JM, Rebholz CM, Lowenstein RA, Mitchell PM, Feldman JA. Ultrasonography-guided peripheral intravenous catheter survival in ED patients with difficult access. Am J Emerg Med. 2010;28(1):1–7. https://doi.org/10.1016/j.ajem.2008.09.001.
Davidson I, Lok C, Dolmatch B, Gallieni M, Nolen B, Pittiruti M, et al. Virtual reality: emerging role of simulation training in vascular access. Paper presented at the Seminars in Nephrology. 2012.
Davis J. Central line associated bloodstream infection: comprehensive, data-driven prevention. Pennsylvania Patient Safety Authority. Pa Patient Saf Advis. 2011;8(3):100–4.
Dougherty L, Lamb J, editors. Principles of intravenous therapy. Oxford: Wiley; 2014.
Dowling S, Barrett S, West R. With nurse practitioners, who needs house officers? Br Med J. 1995;311(7000):309–13.
Eisen LA, Narasimhan M, Berger JS, Mayo PH, Rosen MJ, Schneider RF. Mechanical complications of central venous catheters. J Intensive Care Med. 2006;21(1):40–6.
Elia F, Ferrari G, Molino P, Converso M, De Filippi G, Milan A, Apra F. Standard-length catheters vs long catheters in ultrasound-guided peripheral vein cannulation. Am J Emerg Med. 2012;30(5):712–6. https://doi.org/10.1016/j.ajem.2011.04.019.
Entesari-Tatafi D, Orford N, Bailey MJ, Chonghaile MNI, Lamb-Jenkins J, Athan E. Effectiveness of a care bundle to reduce central line-associated bloodstream infections. Med J Aust. 2015;202(5):247–9.
Evans LV, Dodge KL, Shah TD, Kaplan LJ, Siegel MD, Moore CL, et al. Simulation training in central venous catheter insertion: improved performance in clinical practice. Acad Med. 2010;85(9):1462–9.
Fields JM, Piela NE, Au AK, Ku BS. Risk factors associated with difficult venous access in adult ED patients. Am J Emerg Med. 2014;32(10):1179–82.
Forauer AR, Alonzo M. Change in peripherally inserted central catheter tip position with abduction and adduction of the upper extremity. J Vasc Interv Radiol. 2000;11(10):1315–8.
Gorski L, Hadaway L, Hagle M, McGoldrick M, Orr M, Doellman D. Infusion therapy: standards of practice. J Infus Nurs. 2016;39(Suppl 1):S1–S159.
Hallam C, Weston V, Denton A, Hill S, Bodenham A, Dunn H, Jackson T. Development of the UK Vessel Health and Preservation (VHP) framework: a multi-organisational collaborative. J Infect Prev. 2016;17(2):65–72. https://doi.org/10.1177/1757177415624752.
Hamilton H. A nurse-led central venous vascular access service in the United Kingdom. J Assoc Vasc Access. 2005;10(2):77–80.
Harvey M, Cave G. Ultrasound-guided peripheral venous cannulation using the Seldinger technique. Emerg Med J. 2011;28(4):338. https://doi.org/10.1136/emj.2010.100602.
Hendriksen J, Geersing G, Moons K, De Groot J. Diagnostic and prognostic prediction models. J Thromb Haemost. 2013;11:129–41.
Herrmann-Werner A, Nikendei C, Keifenheim K, Bosse HM, Lund F, Wagner R, et al. “Best practice” skills lab training vs. a “see one, do one” approach in undergraduate medical education: an RCT on students’ long-term ability to perform procedural clinical skills. PLoS One. 2013;8(9):e76354.
Hirvela E, Parsa C, Aalmi O, Kelly E, Goldstein L. Skills and risk assessment of central line placement using bedside simulation with 3-dimensional ultrasound guidance system. Crit Care. 2000;28:A78.
Keyes LE, Frazee BW, Snoey ER, Simon BC, Christy D. Ultrasound-guided brachial and basilic vein cannulation in emergency department patients with difficult intravenous access. Ann Emerg Med. 1999;34(6):711–4.
Lamperti M, Bodenham AR, Pittiruti M, Blaivas M, Augoustides JG, Elbarbary M, et al. International evidence-based recommendations on ultrasound-guided vascular access. Intensive Care Med. 2012;38(7):1105–17.
Larsen E, Keogh S, Marsh N, Rickard C. Experiences of peripheral IV insertion in hospital: a qualitative study. Br J Nurs. 2017;26(19):S18–25.
Lenchus JD. End of the “see one, do one, teach one” era: the next generation of invasive bedside procedural instruction. J Am Osteopath Assoc. 2010;110(6):340–6.
Lenhard A, Moallem M, Marrie RA, Becker J, Garland A. An intervention to improve procedure education for internal medicine residents. J Gen Intern Med. 2008;23(3):288–93.
Levy MM, Dellinger RP, Townsend SR, Linde-Zwirble WT, Marshall JC, Bion J, et al. The Surviving Sepsis Campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Intensive Care Med. 2010;36(2):222–31.
Loukas C, Nikiteas N, Kanakis M, Georgiou E. Evaluating the effectiveness of virtual reality simulation training in intravenous cannulation. Simul Healthc. 2011;6(4):213–7.
Loveday H, Wilson J, Pratt R, Golsorkhi M, Tingle A, Bak A, et al. EPIC3: national evidence-based guidelines for preventing healthcare-associated infections in NHS Hospitals in England. J Hosp Infect. 2014;86(Suppl 1):S1–70. https://doi.org/10.1016/s0195-6701(13)60012-2.
Luciani A, Clement O, Halimi P, Goudot D, Portier F, Bassot V, et al. Catheter-related upper extremity deep venous thrombosis in cancer patients: a prospective study based on Doppler US. Radiology. 2001;220(3):655–60.
Ma IW, Zalunardo N, Pachev G, Beran T, Brown M, Hatala R, McLaughlin K. Comparing the use of global rating scale with checklists for the assessment of central venous catheterization skills using simulation. Adv Health Sci Educ. 2012;17(4):457–70.
Mahler SA, Wang H, Lester C, Conrad SA. Ultrasound-guided peripheral intravenous access in the emergency department using a modified Seldinger technique. J Emerg Med. 2010;39(3):325–9. https://doi.org/10.1016/j.jemermed.2009.02.013.
Maki D, Ringer M. Risk factors for infusion-related phlebitis with small peripheral venous catheters: a randomized controlled trial. Ann Intern Med. 1991;114(10):845–54.
Marschall J, Mermel L, Fakih M, Hadaway L, Kallen A, O’Grady N. Strategies to prevent central line–associated bloodstream infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35(Suppl 2):S89–107.
Marsh N, Webster J, Larson E, Cooke M, Mihala G, Rickard C. Observational study of peripheral intravenous catheter outcomes in adult hospitalized patients: a multivariable analysis of peripheral intravenous catheter failure. J Hosp Med. 2018;13(2):83–9.
McCannon CJ, Hackbarth AD, Griffin FA. Miles to go: an introduction to the 5 Million Lives Campaign. Jt Comm J Qual Patient Saf. 2007;33(8):477–84.
McGee D, Gould M. Preventing complications of central venous catheterization. N Engl J Med. 2003;348(12):1123–33.
Miles G, Salcedo A, Spear D. Implementation of a successful registered nurse peripheral ultrasound-guided intravenous catheter program in an emergency department. J Emerg Nurs. 2012;38(4):353–6. https://doi.org/10.1016/j.jen.2011.02.011.
Miles G, Newcomb P, Spear D. Comparison of dwell-times of two commonly placed peripheral intravenous catheters: traditional vs. ultrasound-guided. Open J Nurs. 2015;5(12):1082.
Miliani K, Taravella R, Thillard D, Chauvin V, Martin E, Edouard S, et al. Peripheral venous catheter-related adverse events: evaluation from a multicentre epidemiological study in France (the CATHEVAL Project). PLoS One. 2017;12(1):e0168637.
Mills CN, Liebmann O, Stone MB, Frazee BW. Ultrasonographically guided insertion of a 15-cm catheter into the deep brachial or basilic vein in patients with difficult intravenous access. Ann Emerg Med. 2007;50(1):68–72. https://doi.org/10.1016/j.annemergmed.2007.02.003.
Moore C. An emergency department nurse-driven ultrasound-guided peripheral intravenous line program. J Assoc Vasc Access. 2013;18(1):45–51.
Moore CL. Ultrasound first, second, and last for vascular access. J Ultrasound Med. 2014;33(7):1135–42.
Mourad M, Kohlwes J, Maselli J, Auerbach AD, MERN Group. Supervising the supervisors—procedural training and supervision in internal medicine residency. J Gen Intern Med. 2010;25(4):351–6.
Moureau N. Catheter-related infection and thrombosis: a proven relationship. A review of innovative PICC technology to reduce catheter-related infection and thrombosis. 2013a. http://www.chlorhexidinefacts.com/docs/Relationship_of_Catheter_Related_Infection_Thrombosis_WP_2012-1261.pdf.
Moureau N. Safe patient care when using vascular access devices. Br J Nurs. 2013b;22(2):S14, S16, S18 passim. https://doi.org/10.12968/bjon.2013.22.Sup1.S14.
Moureau N. Catheter-associated bloodstream infection prevention: what is missing? Br J Healthc Manag. 2014;20(11):502–10.
Moureau NL. Vessel health and preservation: vascular access assessment, selection, insertion, management, evaluation and clinical education. Doctor of Philosophy by Publication (PhD) Thesis and Exegesis (PhD Doctorate), Griffith University. 2017. https://www120.secure.griffith.edu.au/rch/items/e6aea329-fae8-4c41-aa3f-6b4f80298977/1/ (gu1507011216006).
Moureau N, Trick N, Nifong T, Perry C, Kelley C, Carrico R, et al. Vessel health and preservation (Part 1): a new evidence-based approach to vascular access selection and management. J Vasc Access. 2012;13(3):351–6. https://doi.org/10.5301/jva.5000042.
Moureau N, Lamperti M, Kelly L, Dawson R, Elbarbary M, van Boxtel J, Pittiruti M. Evidence-based consensus on the insertion of central venous access devices: definition of minimal requirements for training. Br J Anaesth. 2013;110(3):333–46.
Nayeemuddin M, Pherwani A, Asquith J. Imaging and management of complications of central venous catheters. Clin Radiol. 2013;68(5):529–44.
Nguyen B-V, Prat G, Vincent J-L, Nowak E, Bizien N, Tonnelier J-M, et al. Determination of the learning curve for ultrasound-guided jugular central venous catheter placement. Intensive Care Med. 2014;40(1):66–73.
O’Grady N, Alexander M, Burns L, Dellinger E, Garland J, Heard S, et al. Centers for Disease Control Guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis. 2011;52(9):e162–93.
Primdahl S, Todsen T, Clemmesen L, Knudsen L, Weile J. Rating scale for the assessment of competence in ultrasound-guided peripheral vascular access—a Delphi Consensus Study. J Vasc Access. 2016;17(5):440–5.
Pronovost P, Wu AW, Dorman T, Morlock L. Building safety into ICU care. J Crit Care. 2002;17(2):78–85.
Pronovost P, Needham D, Berenholtz S, Sinopoli D, Chu H, Cosgrove S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU: keystone project. N Engl J Med. 2006;355(26):2725–32.
Ricard J-D, Salomon L, Boyer A, Thiery G, Meybeck A, Roy C, et al. Central or peripheral catheters for initial venous access of ICU patients: a randomized controlled trial. Crit Care Med. 2013;41(9):2108–15.
Rickard CM, Webster J, Playford EG. Prevention of peripheral intravenous catheter-related bloodstream infections: the need for routine replacement. Med J Aust. 2013;199(11):751–2.
Riker MW, Kennedy C, Winfrey BS, Yen K, Dowd MD. Validation and refinement of the difficult intravenous access score: a clinical prediction rule for identifying children with difficult intravenous access. Acad Emerg Med. 2011;18(11):1129–34.
Rippey JC, Blanco P, Carr PJ. An affordable and easily constructed model for training in ultrasound-guided vascular access. J Vasc Access. 2015;16(5):422–7.
Rodriguez-Paz J, Kennedy M, Salas E, Wu A, Sexton J, Hunt E, Pronovost P. Beyond “see one, do one, teach one”: toward a different training paradigm. Qual Saf Health Care. 2009;18(1):63–8.
Rose JS, Norbutas CM. A randomized controlled trial comparing one-operator versus two-operator technique in ultrasound-guided basilic vein cannulation. J Emerg Med. 2008;35(4):431–5. https://doi.org/10.1016/j.jemermed.2007.11.009.
Rusche J, Besuner P, Partusch S, Berning P. CE test: competency program development across a merged healthcare network. J Nurs Staff Dev. 2001;17(5):241–2.
Schmidt GA, Kory P. Ultrasound-guided central venous catheter insertion: teaching and learning. Intensive Care Med. 2014;40(1):111–3.
Schoenfeld E, Boniface K, Shokoohi H. ED technicians can successfully place ultrasound-guided intravenous catheters in patients with poor vascular access. Am J Emerg Med. 2011;29(5):496–501. https://doi.org/10.1016/j.ajem.2009.11.021.
Scott WL. Complications associated with central venous catheters: a survey. Chest. 1988;94(6):1221–4.
Sebbane M, Claret P-G, Lefebvre S, Mercier G, Rubenovitch J, Jreige R, et al. Predicting peripheral venous access difficulty in the emergency department using body mass index and a clinical evaluation of venous accessibility. J Emerg Med. 2013;44(2):299–305.
Sherertz RJ, Ely EW, Westbrook DM, Gledhill KS, Streed SA, Kiger B, et al. Education of physicians-in-training can decrease the risk for vascular catheter infection. Ann Intern Med. 2000;132(8):641–8.
Sou V, Mcmanus C, Mifflin N, Frost SA, Ale J, Alexandrou E. A clinical pathway for the management of difficult venous access. BMC Nurs. 2017;16:64.
Stein J, George B, River G, Hebig A, McDermott D. Ultrasonographically guided peripheral intravenous cannulation in emergency department patients with difficult intravenous access: a randomized trial. Ann Emerg Med. 2009;54(1):33–40. https://doi.org/10.1016/j.annemergmed.2008.07.048.
Stevens R, Mahadevan V, Moss A. Injury to the lateral cutaneous nerve of forearm after venous cannulation: a case report and literature review. Clin Anat. 2012;25(5):659–62.
Taylor DC, Hamdy H. Adult learning theories: implications for learning and teaching in medical education: AMEE Guide No. 83. Med Teach. 2013;35(11):e1561–72.
Taylor RW, Palagiri AV. Central venous catheterization. Crit Care Med. 2007;35(5):1390.
Teramoto T, Tsuchikane E, Yamamoto M, Matsuo H, Kawase Y, Suzuki Y, et al. Successful revascularization improves long-term clinical outcome in patients with chronic coronary total occlusion. IJC Heart Vasc. 2017;14:28–32.
The Joint Commission. Preventing central line–associated bloodstream infections: useful tools, an international perspective. 2013.
Troianos CA, Hartman GS, Glas KE, Skubas NJ, Eberhardt RT, Walker JD, Reeves ST. Guidelines for performing ultrasound guided vascular cannulation: recommendations of the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2011;24(12):1291–318.
Tuffaha HW, Rickard CM, Webster J, Marsh N, Gordon L, Wallis M, Scuffham PA. Cost-effectiveness analysis of clinically indicated versus routine replacement of peripheral intravenous catheters. Appl Health Econ Health Policy. 2014;12(1):51–8. https://doi.org/10.1007/s40258-013-0077-2.
van Loon FH, Puijn LA, Houterman S, Bouwman AR. Development of the A-DIVA scale: a clinical predictive scale to identify difficult intravenous access in adult patients based on clinical observations. Medicine. 2016;95(16):e3428.
Wallis M, McGrail M, Webster J, Marsh N, Gowardman J, Playford E, Rickard C. Risk factors for peripheral intravenous catheter failure: a multivariate analysis of data from a randomized controlled trial. Infect Control Hosp Epidemiol. 2014;35(1):63–8. https://doi.org/10.1086/674398.
White A, Lopez F, Stone P. Developing and sustaining an ultrasound-guided peripheral intravenous access program for emergency nurses. Adv Emerg Nurs J. 2010;32(2):173–88.
Williams S, Dale J, Glucksman E, Wellesley A. Senior house officers’ work related stressors, psychological distress, and confidence in performing clinical tasks in accident and emergency: a questionnaire study. BMJ. 1997;314(7082):713.
Witting MD. IV access difficulty: incidence and delays in an urban emergency department. J Emerg Med. 2012;42(4):483–7.
Witting MD, Schenkel SM, Lawner BJ, Euerle BD. Effects of vein width and depth on ultrasound-guided peripheral intravenous success rates. J Emerg Med. 2010;39(1):70–5. https://doi.org/10.1016/j.jemermed.2009.01.003.
Woo M, Frank J, Lee A, Thompson C, Cardinal P, Yeung M, Beecker J. Effectiveness of a novel training program for emergency residents in ultrasound-guided insertion of central venous catheters. Can J Emerg Med (CJEM/JCMU). 2009;11(4):343–8.
Yen K, Riegert A, Gorelick MH. Derivation of the DIVA score: a clinical prediction rule for the identification of children with difficult intravenous access. Pediatr Emerg Care. 2008;24(3):143–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2019 The Author(s)
About this chapter
Cite this chapter
Alexandrou, E., Mifflin, N., Carr, P.J. (2019). Training and Education. In: Moureau, N. (eds) Vessel Health and Preservation: The Right Approach for Vascular Access. Springer, Cham. https://doi.org/10.1007/978-3-030-03149-7_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-03149-7_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-03148-0
Online ISBN: 978-3-030-03149-7
eBook Packages: MedicineMedicine (R0)