Abstract
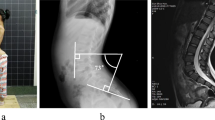
A 3-year-old boy who started walking at 18 months was in your clinic for his 3-year routine visit. His parent suggested that he seemed fine except when he became tired. As he tired, his left leg started to drag slightly. His mother did not notice that he complained of any pain after exercising but the fatigue was reproducible. She felt that the cosmetic appearance of his back looked normal but upon closer inspection, a subtle gluteal asymmetry was detected. Neurologically the child was completely normal except for decreased proprioception and light touch on the left.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Agarwalla PK, Dunn IK, Scott RM, Smith ER. Tethered cord syndrome. Neurosurg Clin N Am. 2007;18:531–47.
Hoffman HJ, Hendrick EB, Humphreys RP. The tethered spinal cord: its protean manifestations, diagnosis and surgical correction. Childs Brain. 1976;2(3):145–55.
Yamada S, Iacono RP. Tethered cord syndrome. In: Pang D, editor. Disorders of the pediatric spine. New York, NY: Raven; 1995. p. 159–73.
Daszkiewicz P, Barszcz S, Roszkowski M, Maryniak A. Tethered cord syndrome in children - impact of surgical treatment on functional neurological and urological outcome. Neurol Neurochir Pol. 2007;41:427–35.
Johnson A. Fatty tumour from the sacrum of a child, connected with the spinal membranes. Trans Pathologic Soc Lond. 1857;8:16–8.
Jones WL. Spina bifida occulta: no paralytic symptoms until seventeen years of age: spine trephined to relieve pressure on the cauda equina: recovery. Br Med J. 1891;1:173–4.
Spiller WG. Congenital and acquired enuresis from spinal lesion: a) myelodysplasia; b) stretching of the cauda equina. Am J Med Sci. 1916;151:469–75.
Brickner WM. Spina bifida occulta: (1) with external signs, with symptoms; (2) with external signs, without symptoms; (3) without external signs, with symptoms; (4) without external signs; without symptoms. Am J Med Sci. 1918;155(4):473–502.
Warf BC. Pathophysiology of tethered cord syndrome. In: McLone DG, editor. Pediatric neurosurgery: surgery of the developing nervous system. 4th ed. Philadelphia, PA: Saunders; 2001. p. 282–8.
Yamada S, Iacono RP, Androde T, Mandybur G, Yamada BS. Pathophysiology of tethered cord syndrome. Neurosurg Clin N Am. 1995;6:311–23.
Yamada S. Tethered cord syndrome in adults and children. Neurol Res. 2004;26:717–8.
Yamada S, Won DJ. What is the true tethered cord syndrome? Childs Nerv Syst. 2007;23:371–5.
Herman JM, McLone DG, Storrs BB, et al. Analysis of 153 patients with myelomeningocele or spinal lipoma reoperated upon for a tethered cord. Presen- tation, management and outcome. Pediatr Neurosurg. 1993;19(5):243–9.
Schoenmakers MA, Gooskens RH, Gulmans VA, et al. Long-term outcome of neurosurgical untethering on neurosegmental motor and ambulation levels. Dev Med Child Neurol. 2003;45(8):551–5.
Hervey-Jumper SL, Garton HJ, Wetjen NM, Maher CO. Neurosurgical management of congenital malformations and inherited disease of the spine. Neuroimaging Clin N Am. 2011;21:719–31.
Muller F, O’Rahilly R. The development of the human brain, the closure of the caudal neuropore, and the beginning of secondary neurulation at stage 12. Anat Embryol (Berl). 1987;176(4):413–30.
Muller F, O’Rahilly R. The primitive streak, the caudal eminence and related structures in staged human embryos. Cells Tissues Organs. 2004;177(1):2–20.
Dias MS, McLone DG. Normal and abnormal early development of the nervous system. In: McLone DG, editor. Pediatric neurosurgery: surgery of the developing nervous system. 4th ed. Philadelphia, PA: Saunders; 2001. p. 31–71.
Wolf S, Schneble F, Troger J. The conus medullaris: time of ascendence to normal level. Pediatr Radiol. 1992;22(8):590–2.
Emans PJ, van Aalst J, van Heurn EL, et al. The Currarino triad: neurosurgical considerations. Neurosurgery. 2006;58(5):924–9.
Iskander BJ, Oakes WJ. Anomalies of the spine and spinal cord. In: McLone DG, editor. Pediatric neurosurgery: surgery of the developing nervous system. 4th ed. Philadelphia, PA: Saunders; 2001. p. 307–23.
Guggisberg D, Hadj-Rabia S, Viney C, et al. Skin markers of occult spinal dysraphism in children: a review of 54 cases. Arch Dermatol. 2004;140(9):1109–15.
McLone DG, Thompson DNP. Lipomas of the spine. In: McLone DG, editor. Pediatric neurosurgery: surgery of the developing nervous system. 4th ed. Philadelphia, PA: Saunders; 2001. p. 289–301.
Sweet J, Kalhorn CG. Spinal dysraphism: a review of clinical manifestations and surgical treatment options. Semin Spine Surg. 2005;17:23–9.
Thompson DNP. Spinal dysraphic anomalies; classification, presentation and management. J Pediatr Child Health. 2010;20:9.
Bowman RM, Mohan A, Ito J, Seibly JM, McLone DG. Tethered cord release: a long-term study in 114 patients. J Neurosurg Pediatr. 2009;3:181–7.
Rajpal S, Tubbs RS, George T, Oakes WJ, Fuchs HE, Hadley MN, et al. Tethered cord due to spina bifida occulta presenting in adulthood: a tricenter review of 61 patients. J Neurosurg Spine. 2007;6:210–5.
Hudgins RJ, Gilreath CL. Tethered spinal cord following re- pair of myelomeningocele. Neurosurg Focus. 2004;16(2):E7.
Giddens JL, Radomski SB, Hirshberg ED, Hassouna M, Fehlings M. Urodynamic findings in adults with the tethered cord syndrome. J Urol. 1999;161:1249–54.
Guerra LA, Pike J, Milks J, Barrowman N, Leonard M. Outcome in patients who underwent tethered cord release for occult spinal dysraphism. J Urol. 2006;176:1729–32.
Naidich TP, McLone DG. Neuroradiology: ultrasonography versus computed tomography. In: Holtzman RNN, Stein BM, editors. The tethered spinal cord. New York, NY: Theime-Stratton; 1985. p. 47–58.
Singh S, Kline-Fath B, Bierbrauer K, Racadio JM, Salisbury S, Macaluso M, Jackson EC, Egelhoff JC. Comparison of standard, prone and cine MRI in the evaluation of tethered cord. Pediatr Radiol. 2012;42:685–91. doi:10.1007/s00247-011-2308-8.
Zugazaga Cortazar A, Martinez M, Feliubadalo D, Bella Cueto MR, Serra L. Magnetic resonance imaging in the prenatal diagnosis of neural tube defects. Insights Imaging. 2013;4:225.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer Science+Business Media New York
About this chapter
Cite this chapter
Torres, M.T.A. (2017). Tethered Cord. In: Greenfield, J., Long, C. (eds) Common Neurosurgical Conditions in the Pediatric Practice. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-3807-0_9
Download citation
DOI: https://doi.org/10.1007/978-1-4939-3807-0_9
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-3805-6
Online ISBN: 978-1-4939-3807-0
eBook Packages: MedicineMedicine (R0)