Abstract
Hallucinations occur in a great variety of neurological conditions and are facilitated by sensory loss. The common end pathway of their pathophysiology involves the activation of cortical sensory areas implicated in normal sensory processing. Based on the presumed pathophysiology, we here classify the hallucinations in four main groups. In migraine aura and epilepsy, hallucinations result from spontaneous intrinsic overactivity in hyperexcitable sensory cortical areas. Deafferentation, i.e. the loss or impairment of sensory input, facilitates hallucinations in the corresponding sensory modality, probably by leading to chronic hyperexcitability of the corresponding cortical areas. The archetypal example of this mechanism is the Charles Bonnet syndrome, where hallucinations are associated with visual impairment. A third mechanism relies on the dissociation of dream and sleep mechanism, as illustrated by hypnagogic and hypnopompic hallucinations. Finally, in the course of neurodegenerative diseases such as Parkinson’s disease and dementia with Lewy bodies, hallucinations are frequent and probably result from a combination of factors, including dysfunction of both bottom–up sensory processing and top–down modulatory mechanisms, as well as dream intrusion phenomena and facilitating pharmacological factors.
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
In a survey of more than 13,000 members of the general population aged 15 years or more, about one-quarter of respondents reported having daytime hallucinatory experiences at least once a month in 6% of cases (Ohayon 2000). Considering the point prevalence of schizophrenia (around 0.5%) and other psychotic disorders, this means that hallucinations occur in the non-psychiatric population. This chapter, devoted to hallucinations associated with neurological disorders and sensory loss, focuses on the phenomenological characteristics of hallucinations and some related phenomena, and on the possible underlying mechanisms.
1 Definitions and Methodological Considerations
1.1 Definitions
Definitions of hallucinations have previously been provided (see, e.g. Chaps. 1 and 3, this volume). Some related terms are commonly used in the context of neurological diseases. The term pseudo-hallucinations has received various definitions (e.g. hallucinations with preserved insight, or vivid internal images), none of which is universally accepted (van der Zward and Polak 2001). The same is true of the term hallucinosis, which is often used as an equivalent for hallucinations associated with neurological diseases or sensory impairment. However, the meanings of this term have varied over time, and hallucinosis is now variously defined. It first designated, after Wernicke, predominantly hallucinatory syndromes, as observed in heavy drinkers (Berrios 1985). Later, Lhermitte (1932), in his work on peduncular hallucinosis, referred to “hallucinatory states which do not drive the development of delusions”. Others emphasized the preservation of insight, and (or) the link with sensory impairment. This fuzzy concept is useless in practice and should be discarded. As hallucinations reported in neurological settings fit the general definitions of hallucinations, only this latter term will be used here. Finally, in the context of neurological disorders, the term psychosis usually refers to a mental state characterized by hallucinations and/or delusions. However, definitions have varied over the years and may encompass other related phenomena.
1.2 Phenomenology of Hallucinations
Hallucinations, generally defined as perceptions that occur without external stimulation of the relevant sensory organ, may be auditory, visual, somatosensory (tactile or somatic), olfactory, gustatory or multi-modal. Visual hallucinations may be elementary/simple (lines, dots, geometrical patterns) or complex (objects, animals, people, landscapes, etc.). Auditory hallucinations may also be simple (knocks, rings) or complex (music, voices). When auditory verbal hallucinations are present in the context of a brain disease or sensory loss, they are usually neutral (or incomprehensible) and clearly different from the pejorative or threatening auditory hallucinations characteristic of schizophrenia.
Hallucinations are distinguished from illusions, which are misperceptions or misinterpretations of a real external stimulus. The misperception may concern the physical characteristics of the object (such as size, colour, motion or orientation) or its identification (e.g. a cushion is misperceived as a cat or a trunk as a person). The frontier between hallucinations and illusions may be tenuous, and their mechanisms are probably similar. In addition, hallucinations and illusions may both occur in a number of pathological situations. Another phenomenon related to hallucinations is the feeling of presence, i.e. the vivid sensation that somebody (distinct from oneself) is present nearby, when no-one is actually there, in the absence of sensory clues suggesting a presence. Although the feeling of presence is not a sensory perception, projection of the sensation into the extrapersonal space, along with the frequent association with visual hallucinations or illusions, support its hallucinatory nature (Fénelon et al. 2011).
The person may or may not have insight into the fact he or she is having a hallucination. Although “insight” in psychiatry is commonly viewed as a multi-dimensional construct incorporating awareness of illness, symptoms and the need for treatment (Cooke et al. 2010), insight refers, when applied to hallucinating subjects, to awareness of the hallucinatory nature of the percept.
1.3 Evaluation
To identify and rate hallucinations, the examiner relies on the patient’s and/or caregiver’s accounts. Many patients do not spontaneously report their hallucinations, either because they are brief and non-frightening, or because of fears of being considered insane. Hallucinations therefore have to be sought with specific questions or scales. There is no “gold-standard” assessment tool in the setting of neurological disorders. Single items from scales have been used to identify psychosis, as well as self-developed questionnaires or inventories. The latter are useful for recording the variety of psychotic symptoms but do not allow quantitative assessment, as needed for example in therapeutic trials or follow-up studies. In neurology, scales for rating hallucinations and other psychotic symptoms have been taken from the fields of psychiatry and dementia (e.g. the Neuropsychiatric Inventory). Specific scales have also been devised for use in some disorders (particularly Parkinson’s disease), but they are poorly validated and none is widely used (Fernandez et al. 2008).
2 Epidemiology and Overview of Mechanisms
2.1 Prevalence
The prevalence of hallucinations in the overall neurological population is unknown. Table 4.1 shows the estimated prevalence of hallucinations in certain frequent conditions. The wide range of pathological conditions and of brain areas potentially involved suggests that the underlying mechanisms are heterogeneous. Visual hallucinations are the most prevalent type in patients with neurological or sensory diseases.
2.2 The Cortical Origin of Hallucinations
Pioneering work following the first world war established that occipital stimulation generated visual hallucinations and that hallucinations became more complex when stimulation shifted from the primary visual cortex to association visual cortices (e.g. see the review by Lhermitte 1951). It was also shown that seizures secondary to occipital lesions were often preceded by a visual aura. The role of the cortex in generating hallucinations was further demonstrated by Penfield and Perot (1963), who triggered complex auditory and visual hallucinations by stimulating the auditory and visual cortices of patients undergoing surgery for epilepsy. More recently, the role of specific areas of the cortex has been demonstrated by functional imaging. Using functional magnetic resonance imaging (fMRI) in patients with Charles Bonnet syndrome (CBS) (patients experiencing hallucinations associated with eye disease, see below), it has been shown that various types of visual hallucination correlate with cerebral activity in the ventral extrastriate visual cortex, that the content of the hallucinations reflects the functional specialization of the region, and that patients who hallucinate have increased ventral extrastriate activity, which persists between hallucinations (ffytche et al. 1998). To summarize, hallucinations in a given sensory modality result from activation of cortical areas normally involved in the processing of sensory stimuli in the same modality. Simple (elementary) hallucinations result from primary sensory cortex activation, while complex hallucinations result from activation of associated sensory areas (Fénelon and Hamdani 2010). Finally, focal brain lesions that cause isolated hallucinations in a single sensory modality are practically always located in the brain pathway of this sensory modality (Braun et al. 2003). Importantly, the crucial role of sensory cortical areas in the production of hallucinations does not rule out a role, at least in some cases, of subcortical structures connected to these areas, e.g. thalamus nuclei or amygdala (for review, see Aleman and Larøi 2008).
2.3 Overview of Potential Mechanisms
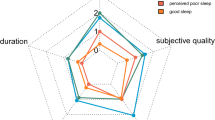
The cortical activation underlying hallucinations may result from various mechanisms (reviews in Manford and Andermann 1998; Braun et al. 2003; Aleman and Larøi 2008; Fénelon and Hamdani 2010), as summarized in Fig. 4.1. In the simplest case, hallucinations result from spontaneous intrinsic overactivity in hyperexcitable sensory cortical areas. This mechanism is generally considered to account for the auras in migraine and epilepsy. Deafferentation, i.e. the loss or impairment of sensory input, facilitates hallucinations in the corresponding sensory modality. General disinhibition theories of hallucinations were first forwarded by Jackson: “hallucinations (…) are due to action of centers which, except for overexcitement from loss of control, are healthy” (Jackson 1931). In the perceptual release theory of West (1962), hallucinations arise when the constant flow of sensory inputs is impaired, allowing the emergence of earlier perceptions or “traces” into consciousness. More specifically, the “release” theory was applied by Cogan (1973) to visual hallucinations associated with impaired visual input. The core hypothesis is that stimulus-driven, bottom–up visual processing inhibits the spontaneous activity of visual cortical areas and facilitates the release of stored images. More recent concepts suggest that the lack of input leads to chronic hyperexcitability. However, the extent to which top–down mechanisms are involved in deafferentation-associated hallucinations is unknown. A third mechanism involves dissociation between dream and sleep mechanisms. The relation between dreams and hallucinations has long been debated. Maury (1861) stressed the relationship between dreams and the hypnagogic hallucinations he described. Later, Lhermitte, in the 1920s, suggested that hallucinations secondary to a lesion of the upper brainstem (“peduncular hallucinosis”) resulted from a dissociation of dream and sleep mechanisms (Lhermitte 1932). Finally, in some conditions, such as Parkinson’s disease, prevalent models suggest that a combination of factors result in the onset of hallucinations, including dysfunction of both bottom–up sensory processing and top–down modulatory mechanisms, as well as dream intrusion phenomena and facilitating pharmacological factors. A general model of recurrent complex visual hallucinations occurring during the course of a variety of conditions was proposed by Collerton et al. (2005), based on cognitive models of scene perception. In their “Perception and Attention Deficit” model, a combination of impaired attentional binding and poor sensory activation of a correct “proto-object” (or template), in conjunction with a relatively intact scene representation, bias perception to allow the intrusion of a hallucinatory proto-object into a scene perception.
Schematic representation of possible mechanisms of hallucinations in neurological diseases. This simplified representation of the possible mechanisms of hallucinations is based on general schemes of perception. Hallucinations in a given sensory modality are associated with aberrant activity in the sensory cortices involved in normal processing of external stimuli in the same modality. Hallucinations may arise from: 1 primary abnormal activation of sensory cortices; 2 deafferentation leading to activation of sensory cortices; 3 internal input (dream) occurring while conscious and interpreted as an external stimulus; 4 deregulation of top–down modulations. These mechanisms may occur simultaneously and potentiate one another, leading to aberrant activation of sensory cortices and hallucinatory experiences. Pharmacological factors (not represented) may facilitate hallucinatory experiences, probably by acting at various levels
3 Primary Excitation of Cortical Areas or Networks
3.1 Migraine Aura
With a cumulative lifetime incidence of 43% in women and 18% in men, migraine is the most common neurological disorder (Charles 2009). Headache is its most characteristic feature but other symptoms may occur, such as aura, which, according to the International Headache Society, is “a recurrent disorder consisting in episodes of reversible focal neurological symptoms that usually resolve gradually after 5–20 min and last less than 1h” (Aleci and Liboni 2009). Visual aura is the most frequent form of migraine aura, followed by sensory, aphasic and motor aura (Russel and Olesen 1996). Although the aura typically precedes a headache, it may also occur in isolation. Typically, the visual aura consists of a flickering bright uncoloured (white or silver) unilateral zigzag line (fortification pattern, or teichopsia) in the centre of the visual field, which progresses towards the periphery, leaving a scotoma. Interestingly, complex hallucinations of people or objects have almost never been reported in migraine auras (Wilkinson 2004). The neural basis for the migraine aura is thought to be cortical spreading depression, a phenomenon first described by Leão in rodents and consisting in a wave of neuronal and glial depolarization, followed by long-lasting suppression of neural activity (Tfelt-Hansen 2010). The metabolic wavefront would sequentially trigger the cortical receptive field cells tuned to orientation discrimination, thus leading to the hallucinatory perception of segments with specific orientations forming the typical zigzag pattern (Aleci and Liboni 2009). fMRI studies have identified propagated waves of blood flow and brain activity during migraine visual aura, with temporal and spatial characteristics remarkably similar to those seen in cortical spreading depression, including transient hyperperfusion followed by sustained hypoperfusion (Hadjikhani et al. 2001).
Sensory aura (usually paresthesia progressively affecting the hand and ipsilateral face), may be considered as a form of elementary somatosensory hallucination. More complex hallucinatory phenomena are occasionally reported, such as the “Alice in Wonderland” syndrome, a term coined by Todd in 1955, after the syndrome was first described by Lippman in 1952 (Evans and Rolak 2004). In its narrow definition, the syndrome refers to a distortion (shrinking or enlargement) of the body image, involving all or part of the body. Although first described in this setting, Alice in Wonderland syndrome is not specific to migraine and may occur in patients with epilepsy, intoxication and hypnagogic states, and in children with viral encephalitis (Weidenfeld and Borusiak 2011).
3.2 Epilepsy
3.2.1 General Aspects
In a large series of partial epilepsy, hallucinations were part of the aura in 13% of cases (Mauguière 1999). They were more often simple than complex, and involved the following sensory modalities in decreasing order of frequency: visual, somatosensory, auditory, olfactory and gustatory. However, the precise prevalence and phenomenology of hallucinations in partial epilepsy is difficult to determine, as published series are commonly based on the lobar topography of the seizures rather than on the phenomenology. Moreover, hallucinations rarely occur in isolation during the course of a partial seizure, and patients may not recall a sensory symptom, meaning that the prevalence of sensory aura may be underestimated. Simple hallucinations probably reflect epileptic discharges in a primary sensory cortex. When they constitute the initial ictal symptoms, they can provide localizing information (Kasper et al. 2010). However, other mechanisms have been proposed for epileptic complex hallucinations, relying on the Jacksonian concept of dissolution, or on the concept of activation of specific circuits by a focal discharge (Mauguière 1999).
3.2.2 Ictal Sensory Phenomena
Visual hallucinations and illusions are common during occipital seizures, although their prevalence has been diversely appreciated, with values ranging from 8 to 72% (Eliott et al. 2009a). Typically, elementary visual hallucinations consist of multiple bright-coloured small circular spots or circles, appearing in a temporal hemifield often moving contralaterally or in the centre where they may be flashing (Panayiotopoulos 1999). The phenomenon lasts for seconds and may progress to other non-visual ictal symptoms. Negative symptoms (scotoma, hemianopia, blindness) may be associated and the seizure may be followed by headache. Although elementary visual hallucinations are typically different in the two disorders, occipital seizures may be difficult to distinguish from migraine with visual aura, especially in children. Simple illusions associated with occipital seizures include seeing objects or persons changing in size (macropsia and micropsia), shape (metamorphopsia) or colour (dyschromatopsia and achromatopsia). Illusory movements (kinetopsia) have also been reported (Eliott et al. 2009a; Kasper et al. 2010). Elementary visual hallucinations and illusions may occur in patients with occipito-temporal and anteromedial temporal seizure onset, as well as complex visual hallucinations (mainly persons or animals) (Bien et al. 2000). The “dreamy state”, first described by Jackson, refers to a sensation of déjà vécu and/or complex visual hallucinations (scenes, faces or people). Hallucinations may consist of a replaying of past experience, hence the term “experiential hallucinations” coined by Penfield (Penfield and Perot 1963), and they may also have an affective component. Stereoelectroencephalographic recordings and stimulation studies performed during presurgical assessment suggest that dreamy states involve the activation of a network including the hippocampus, amygdala and rhinal cortex (Vignal et al. 2007).
Ictal auditory hallucinations may be elementary (tones, sounds or noises), in which case they are associated with discharges in the primary auditory cortex (Heschl’s gyrus). Complex auditory hallucinations consist of hearing voices or music, and involve activation of more extensive and lateral parts of the superior temporal gyrus. Auditory hallucinations may be combined with visual or olfactory hallucinations. Voice hallucinations can arise from both dominant and non-dominant epileptic foci (Eliott et al. 2009a). Importantly, hallucinatory voices during partial seizures only rarely take the form of commanding or threatening voices talking in the third person (Kasper et al. 2010). However, psychotic states, including auditory hallucinations and typically lasting hours, may occur in temporal lobe complex partial status (Eliott et al. 2009b).
Contrary to a generally accepted idea, olfactory and gustatory hallucinations are rare in epilepsy. Olfactory hallucinations (pleasant or unpleasant) usually involve mesial temporal structures, including the amygdala. Gustatory hallucinations involve temporal and/or parietal cortices.
The most frequent somatosensory seizure symptoms are lateralized paresthesia; pain and thermal perceptions are less frequent (Mauguière 1999; Eliott et al. 2009a, b; Kasper et al. 2010). Somatosensory symptoms are associated with activation of parietal and/or insular cortices. Somatosensory illusions include image distortions of all or part of the body, illusions of displacement of a stationary limb and, exceptionally, the sensation of an extra limb.
3.2.3 Autoscopic Phenomena
Partial seizures may result in illusory own-body perceptions, which have been extensively studied in recent years and have provided new insights into body perception and self-consciousness (reviews in Blanke and Mohr 2005; Blanke and Metzinger 2009). Three related phenomena have been described (see Fig. 4.2): (a) autoscopic hallucinations, where the subject sees an image of him/herself in the external space, viewed from his/her own physical body; (b) out-of-body experiences, where subjects locate their self outside their body and see their body from this (generally elevated) disembodied location; (c) heautoscopy, which is an intermediate form between autoscopy and out-of-body experience: the subject sees a double of her or himself in the extrapersonal space but finds it difficult to decide whether the self is situated within the physical body or the autoscopic virtual body. Some forms of feeling of presence, where the subject feels the presence of an illusory self nearby, belong to the same spectrum of phenomena. Blanke et al. (2004) suggested that these phenomena are related to a failure to integrate proprioceptive, tactile and visual information with respect to one’s own body, and to vestibular dysfunction leading to additional disintegration between the personal and extrapersonal spaces (Blanke et al. 2004). Neuroanatomical analyses and stimulation studies in patients with epilepsy suggest that autoscopic phenomena are related to damage or dysfunction of focal regions of the brain, namely the right parieto-occipital or temporo-occipital cortices for autoscopy, the left temporo-parietal cortex for heautoscopy and the right temporo-parietal cortex for out-of-body experiences. Finally, it should be emphasized that autoscopic phenomena may arise from a variety of non-epileptic causes, including migraine (Blanke and Mohr 2005).
Phenomenology of autoscopy and related phenomena. Reprinted from Blanke and Mohr (2005), with permission from Elsevier
4 Deafferentation
4.1 Hallucinations and Visual Impairment
4.1.1 Charles Bonnet Syndrome
The CBS commonly refers to visual hallucinations occurring in the course of eye disease. However, this term, coined by G. de Morsier in the 1930s, first referred to visual hallucinations in cognitively intact elderly subjects, but was later used to denote visual hallucinations with preserved insight, irrespectively of their cause (ffytche 2009). Thus, depending on the definition and/or diagnostic criteria, eye disease may either be mandatory or a simple risk factor for the syndrome. The prevalence of complex visual hallucinations in visually impaired populations has been estimated at between 11 and 15% (Menon 2003), but reached 63% in one series (Menon 2005). The prevalence of elementary visual phenomena is higher, at an estimated 41–59%.
Positive visual symptoms associated with eye disease consist of hallucinations (simple or complex) and illusions. Simple hallucinations include very elementary percepts such as simple shapes or flashes, and more elaborate geometrical patterns such as brickwork, grid-like, lattice or network patterns, named tesselopsia (a term referring to mosaics) by ffytche and Howard (1999). Illusions include modifications of size (micropsia or macropsia) or colour (dyschromatopsia) and distortion of faces. The different varieties of palinopsia may be considered as illusions, and include visual perseveration or temporal palinopsia (a percept persists as the patient moves the eyes to successive fixation points); illusory visual spread, where a pattern extends beyond its true boundaries to cover neighbouring objects, and polyopia, in which a percept becomes multiplied (ffytche and Howard 1999). Complex visual hallucinations have been systematically investigated by Teunisse et al. (1996) and are highly varied: they can include people or faces, animals, objects and, less frequently, complete scenes. For ffytche (2007), the prototypical hallucinatory subsyndromes of CBS consist of a range of simple phenomena (see above), palinopsia, faces (typically grotesque with cartoon-like quality), and lilliputian figures (small people). In most cases, the hallucinations are colourful, lack a personal meaning and last from seconds to minutes. They tend to recur and are rarely stereotyped. They are more frequent in the evening, at night or in low-light conditions. The emotional response to the hallucinations is negative in about one-third of patients. Insight into the unreal nature of the experience is typically preserved (Teunisse et al. 1996), and is mandatory in the diagnostic criteria of Gold and Rabins (1989). However, as stressed by Menon (2003), insight is not an all-or-none phenomenon: it may be delayed, fluctuating or partial. Finally, hallucinations in CBS are solely visual.
Few studies have examined the natural history of CBS. Recovery or improvement of vision may lead to cessation of the hallucinations. If the visual impairment persists, the course seems to be variable. In a cross-sectional study, 36% of subjects with CBS said they had had visual hallucinations for more than 2 years (Khan et al. 2008). In a prospective study of only 10 patients, 4 patients still had hallucinations at 3 years (Holroyd and Rabins 1996).
In patients with eye disease, the main factors associated with hallucinations are lower visual acuity, lower contrast sensitivity and older age (ffytche 2009). The nature of the eye disease is not relevant. One important issue is the role of cognitive impairment. As previously stated, the absence of cognitive impairment is sometimes included in the definition of CBS. However, in patients with cognitive impairment, during the course of Alzheimer’s disease for example, coincident eye disease is a risk factor for visual hallucinations (Holroyd and Sheldon-Keller 1995).
The neurophysiological sequence of events from deafferentation to hallucinations is unclear. As stated above, the traditional view is that a loss of visual input diminishes cortical inhibition and “releases” visual hallucinations. However, activation of the cortical areas that generate hallucinations does not follow the interruption of inhibitory inputs, as previously hypothesized, but could rather depend on biochemical and molecular changes in the deafferented neurons, leading to hyperexcitability and increased spontaneous activity (for a review, see Burke 2002). Burke (2002) has stressed that the presence of high-frequency bursts of activity rather than the absolute level of activity may be a critical feature of spontaneous activity. Such bursts could explain the paroxysmal temporal pattern of the hallucinations. Taking induced hallucinations in normal-sighted individuals as a model, ffytche (2008) proposed that hallucinations in eye disease might result from a shift from tonic to burst firing in the thalamocortical circuitry.
4.1.2 Hallucinations Associated with Lesions of Retrochiasmal Visual Pathways
Hemianospia, quadrantanopsia and cortical blindness (resulting from bilateral lesions of the visual cortices) may be associated with positive phenomena within the field defect. Positive spontaneous visual phenomena in the hemianopic field occur in up to 40% of patients with hemianopia of ischemic origin (Vaphiades et al. 1996; Baier et al. 2010). Positive phenomena consist of hallucinations (either simple—phosphenes or geometric figures—or complex), illusions or palinopsia. When associated with stroke, they appear after a latent period (hours or days) and usually disappear within a few days or weeks (Kolmel 1985). In a series of patients with ischemic lesions, hallucinations were associated with circumscribed, occipital ischemic lesions, while larger lesions affecting the temporal visual associative areas precluded the development of hallucinations. In another study, using voxelwise statistical lesion analysis, phosphenes and simple visual hallucinations were specifically associated with damage to Brodmann areas 17 and 18 (respectively V1 and V2) and the optic radiations (Baier et al. 2010). These findings are compatible with the hypothesis that hallucinations result from a release from inhibitory input of visual areas bordering the damaged occipital lesion. However, an alternative explanation is that spontaneous activation occurs in, or at the edges of, the ischemic region, following local metabolic changes (Baier et al. 2010). The role of hyperexcitability in visual cortical areas, whether due to loss of inhibition or to focal metabolic changes in the damaged zone, is supported by the suppression of visual hallucinations and illusions by low-frequency repetitive transcranial magnetic stimulation of the occipital cortex in a patient with bilateral visual defects due to occipital ischemic lesions (Merabet et al. 2003). Interestingly, in a positron emission tomography (PET) study, visual hallucinations that occurred during recovery from cortical blindness were associated with increased regional cerebral blood flow in the initially severely hypometabolic parieto-occipital and temporo-lateral cortex (Wunderlich et al. 2000).
5 Hallucinations and Auditory Impairment
Deafness can be associated with a variety of simple or complex auditory hallucinations, of which the most intriguing and best-studied are musical hallucinations (Stewart et al. 2006). In a series of 125 elderly subjects with hearing impairment, one-third had hallucinations. Most were elementary (including tinnitus), while 2.5% of subjects heard voices and 2.5% heard music (Cole et al. 2002). Musical hallucinations can evolve from tinnitus or other elementary auditory hallucinations, a phenomenon first described by Hécaen and Ropert (1963). Most subjects complain of hearing familiar tunes. The hallucinations may be stereotyped or consist of a small number of tunes. These hallucinations are vivid and may be very realistic, but insight is preserved. The subject cannot stop the phenomenon voluntarily but, in some instances, may switch from one tune to another by concentrating. The hallucinations become “louder” during silence, and are attenuated by environmental noise (e.g. conversations and real music). A few cases of musical palinacousis (auditory perseveration) have been reported (Griffiths 2000). Musical hallucinations should be distinguished from musical obsessions, which belong to the spectrum of obsessive-compulsive disorders and lack the typical compelling sense of reality of a perception from an external source (Matsui et al. 2002). Musical hallucinations have a chronic course and have been reported to resist drug therapy.
No definite risk factors for musical hallucinations associated with hearing loss have been identified. A central lesion of the right or left hemisphere and/or a seizure seemed to have a facilitating or triggering role in some cases (Paquier et al. 1992). Musical hallucinations may be associated with disorders other than deafness, including psychiatric illness, focal brain lesions (right or left hemisphere), epilepsy, intoxication and inflammatory encephalopathy (Berrios 1990; Evers and Ellger 2004; Stewart et al. 2006). Several case reports describe patients with possibly relevant co-existing factors (Stewart et al. 2006).
Musical hallucinations associated with deafness are often considered to be an auditory equivalent of CBS. However, their pathophysiology remains obscure. In six patients with musical hallucinations and deafness, PET showed that brain activity increased with the severity of the hallucination in a distributed network distinct from the primary auditory cortex, which included the posterior temporal lobes, the right basal ganglia, the cerebellum and the inferior frontal cortices. This network is similar to that activated during normal perception and imagery of patterned-segmented sound (Griffiths 2000). The author of this PET study forwarded a mechanism based on amplified musical imagery, where the decreased signal-to-noise ratio of auditory transmission in the deaf leads to inappropriate activation of cortical networks usually involved in perception and imagery (Stewart et al. 2006).
6 Phantom Limbs
Phantom sensations, i.e. the vivid impression that an amputated limb is still present and, in some cases, painful, are present in almost all limb amputees (Melzack 1990; Ramachandran and Hirstein 1998; Flor et al. 2006). Phantoms appear immediately in 75% of cases, and the somatosensory experience corresponds to that of the real limb before amputation. As time passes the phantom limb changes shape, becoming “telescoped” into the stump: the patient is left with just the phantom hand or foot in the vicinity of the stump. The sensation gradually fades in many patients. The posture of the phantom is usually “normal”, but it may be unusual and sometimes uncomfortable. A phantom may also occur without amputation, after various types of severe deafferentation, such as brachial plexus avulsion or spinal cord injury. The sensation is vivid, and its “reality” is enhanced by wearing an artificial arm or leg. Interestingly, persons born with missing limbs may also experience phantoms. Functional imaging studies suggest that the phantom limb phenomenon results from reorganization of somatosensory cortical maps following deafferentation (Ramachandran and Hirstein 1998; Flor et al. 2006).
7 Dream-Like Hallucinations
The phenomenology of dreams is clearly different from that of visual hallucinations occurring in the course of brain disorders such as Lewy body diseases (see Table 4.2), and there appears to be no simple relationship between dreams and hallucinations (Collerton and Perry 2011). However, there is now convincing evidence that the primary states of being (wakefulness, rapid eye movement (REM) sleep and non-REM sleep) are not mutually exclusive but may become admixed or oscillate rapidly, resulting in numerous clinical phenomena, some of which are related to hallucinations (Mahowald and Schenck 2001).
7.1 Hypnagogic and Hypnopompic Hallucinations
Hallucinations occurring in the wake–sleep and sleep–wake transitions are termed hypnagogic and hypnopompic, respectively. Given their relation to REM sleep-associated dreams, the hallucinatory nature of these phenomena is not recognized in DSM IV. They are frequent in the general population, especially in younger subjects. In a large survey, hypnagogic and hypnopompic hallucinations were reported by respectively 37% and 12.5% of nearly 5,000 non-clinical subjects aged 15 years or more (Ohayon et al. 1996).
Hypnagogic and hypnopompic hallucinations are also reported in narcolepsy, a sleep disorder characterized by severe, irresistible daytime sleepiness and sudden loss of muscle tone (cataplexy), often associated with sleep-onset or sleep-offset paralysis and hallucinations, frequent movements and awakening during sleep and weight gain. Cataplexy is absent in a subset of patients. The disorder is due to early loss (possibly of auto-immune origin) of hypothalamic neurons that produce hypocretin, a wakefulness-associated neurotransmitter present in cerebrospinal fluid (Dauvilliers et al. 2007). Hallucinations occur in up to 66% of patients with narcolepsy and cataplexy (Billiard et al. 1983). In a recent series of 100 patients with narcolepsy, hallucinations were more frequent in patients with cataplexy (59%) than in those without cataplexy (28%) (Leu-Semenescu et al. 2011). Sleep-onset and sleep-offset hallucinations are more severe in narcoleptic patients than in healthy subjects. They are visual in most cases, consisting mainly of human characters (sometimes incomplete or distorted) and animals. Auditory hallucinations are mostly non-verbal. Tactile hallucinations involve contacts with persons or animals, sometimes with a feeling of pressure. Kinetic or motor hallucinations consist in sensations of floating, movement of all or part of the body, and out-of-body experiences. Patients may also experience illusions (visual or auditory) and/or a feeling of presence. These hallucinations are commonly multi-modal, realistic and also frightening, especially when associated with sleep paralysis. Insight may be lost, at least transiently. Even if patients are retrospectively well aware of the nature of these phenomena, some report difficulty in differentiating dreams from reality and might occasionally be misdiagnosed as schizophrenia. However, delusional thinking is exceptional (Dauvilliers et al. 2007; Fortuyn et al. 2009; Leu-Semenescu et al. 2011).
Hypnagogic hallucinations have been shown to occur when patients fall directly into REM sleep, suggesting that hallucinations in narcolepsy share mechanisms with dreams. Polysomnographic studies suggest that some hallucinations in Lewy body disorders (Parkinson’s disease and dementia with Lewy bodies (DLB)) could also result from the intrusion of dreaming into the awake state (Arnulf et al. 2000; Manni et al. 2011). Further insight into the pathophysiology of hypnagogic hallucinations has been provided by fMRI experiments comparing healthy individuals experiencing hypnagogic auditory hallucinations to non-hallucinators (Lewis-Hanna et al. 2011). Results suggested that hallucination proneness was associated with increased sensitivity of auditory and polysensory association cortex to auditory stimulation, an effect possibly due to enhanced attentional bias from the anterior cingulated gyrus.
7.2 State Dissociation
Prolonged dream-like vivid hallucinations are also present in status dissociatus, a form of parasomnia due to extreme dissociation between wakefulness, REM sleep and non-REM sleep (Raggi et al. 2010). Status dissociatus is observed in various diseases, such as treated narcolepsy–cataplexy, dementia, multiple system atrophy, status post-cardiac surgery, Morvan’s chorea, protracted alcohol withdrawal, fatal familial insomnia and Guillain–Barré syndrome. The concept that visual hallucinations in peduncular hallucinosis (Benke 2006) result from intrusions of dreams in the waking state, as postulated by Lhermitte, is debated and awaits polysomnographic confirmation (Braun et al. 2003).
8 Hallucinations in Neurodegenerative Diseases
Hallucinations are common in the course of the three most frequent neurodegenerative diseases, namely Alzheimer’s disease, Parkinson’s disease and dementia with Lewy bodies. Hallucinations have prognostic value in these patients, negatively impact quality of life, and increase the caregiver burden and stress. They also raise complex pathophysiological issues.
8.1 Parkinson’s Disease
The hallucinations of Parkinson’s disease (PD) have been extensively studied in recent years (reviews in Diederich et al. 2009; Fénelon 2010).
8.1.1 Clinical Features
Recent diagnostic criteria (Ravina et al. 2007) for “Parkinson’s disease-associated psychosis” require at least one of the following features: hallucinations, delusions, sense-of-presence and visual illusions, occurring with a clear sensorium and a chronic course (thus excluding delirium). Complex visual hallucinations are the most common type, and mostly consist of persons (who may or may not be familiar) or, less commonly, animals or objects. The hallucinated figures are usually single or few in number, and may be relatively stereotyped in a given patient. The hallucinations appear and vanish suddenly. Hallucinatory images are seen superimposed on the normal background scene. They recur in short sequences (seconds or minutes) and are more frequent in the evening and night. Auditory hallucinations may be elementary (ringing, knocks, etc.) but are usually complex. When auditory verbal hallucinations are present, they are neutral and clearly different from the pejorative or threatening auditory hallucinations characteristic of schizophrenia. Tactile hallucinations usually involve contact with small animals or being touched by someone, without the delusional component present in the Eckbom syndrome. Olfactory hallucinations may also occur. “Minor” psychotic symptoms include visual illusions (typically seeing an inanimate object as a living being) and a feeling of presence (see Sect. 4.1.2). Several hallucinatory phenomena may occur simultaneously: for instance, the patient may hear unreal persons conversing, or see and feel a small animal creeping along his or her leg. In a minority of cases, especially in patients with cognitive impairment, delusions may accompany hallucinations. Patients who are free of cognitive impairment realize the hallucinatory nature of their hallucinations, while demented patients commonly lose insight. Some patients with cognitive impairment may have partial and/or fluctuating insight.
8.1.2 Frequency
Visual hallucinations are present in one-quarter to one-third of PD patients. Auditory hallucinations are rarer. Hallucinations in other modalities were not systematically sought in most studies and their prevalence may be underestimated. If illusions and minor hallucinations (e.g. a sense of presence) are taken into account, the prevalence is higher, reaching 40–75% among chronically treated PD patients. The lifetime prevalence of hallucinations is higher than that observed in point prevalence studies, reaching at least 50%. Finally, the prevalence of hallucinations is higher in PD patients with dementia, in whom it reaches 50–70% (Fénelon and Alves 2010).
8.1.3 Associated Factors
The role of dopaminergic treatment has long been considered critical. Indeed, in controlled therapeutic trials, hallucinations are reported to be more frequent with dopaminergic agonists than with levodopa alone or placebo. However, disease-related factors play an important part as well. In clinical studies the main disease-related factor is severe cognitive impairment and/or dementia. Other significant concomitants of hallucinations or psychosis are older age, a longer PD duration, a greater severity of PD, altered dream phenomena (vivid dreams, nightmares, REM-associated behavioural disorder), daytime somnolence and abnormalities of visual input due either to coincident ocular disease or to specific retinal dysfunction affecting contrast sensitivity and colour discrimination. A facilitating role of depression is suggested by some studies.
8.1.4 Course and Prognosis
Hallucinations usually occur several years after PD onset. Once they have developed, hallucinations become a recurrent and chronic problem in most patients with PD. Patients with mild hallucinations and retained insight tend to have more severe hallucinations and to lose insight as the disease progresses. In longitudinal studies, hallucinations are associated with a higher risk of dementia, nursing-home placement and mortality.
8.1.5 Pathophysiology
Neuroimaging studies in PD have given conflicting results but generally point to decreased visual input and a dysfunction of “top–down” modulatory processes. In PD and DLB, pathological studies have shown an association between visual hallucinations and higher densities of Lewy bodies in the temporal lobe and amygdala, and also in other cortical areas. Dopaminergic, serotoninergic and/or cholinergic widespread projection pathways have been implicated in the genesis of hallucinations, based mainly on indirect pharmacological evidence or more theoretical considerations.
The number and heterogeneity of clinical and biological factors associated with hallucinations preclude any simple explanatory model. Hallucinations may constitute a common end pathway of different, and possibly associated, underlying mechanisms, including (a) dopaminergic overactivity and/or an imbalance in monoaminergic (relatively preserved) and cholinergic (altered) neurotransmission; (b) altered brainstem sleep/wake and dream regulation; (c) visual pathway dysfunction, whether non-specific (coincidental ocular disease) and/or specific (e.g. PD-associated retinal dysfunction and functional alterations in the ventral stream of visual cortical pathways); and (d) dysfunction of top–down visual mechanisms, such as impaired attentional focus. Finally, (e) antiparkinsonian drugs and other pharmacological agents may interfere with the preceding mechanisms at many levels. Diederich et al. (2005) forwarded an integrative model based on Hobson’s work on factors regulating consciousness (review in Hobson 2009). This model emphasizes dysregulation of the gating and filtering of external perception and internal image production. Other models involve cognitive psychology-based models of scene perception (see Sect. 4.2.3) (Collerton et al. 2005).
8.2 Dementia with Lewy Bodies
The central feature of DLB is a progressive cognitive decline interfering with social and occupational function. Recurrent visual hallucinations are one of the three core features, along with fluctuating cognition and spontaneous parkinsonism (Mckeith et al. 2005). Two core features are required for the diagnosis of probable DLB, and only one is required for diagnosis of possible DLB. Hallucinations of other modalities and systematized delusions are included among the supportive features. The frequency of hallucinations in DLB is difficult to assess because the clinical diagnostic criteria have high specificity but low sensitivity, especially in subjects with severe cognitive impairment (Nelson et al. 2010), and secondly because visual hallucinations are included in the core features, which may lead to overestimation of the frequency of hallucinations. Clinical and pathological studies may therefore be more reliable but information on hallucinations relies on retrospective analysis of clinical charts, with a risk of underestimating the frequency of hallucinations. In series with autopsy confirmation of the diagnosis, hallucinations had been present at some time during the disease course in an average of 46% of patients (range 13–80%) (McKeith 2002). In another retrospective autopsy study, visual hallucinations had occurred in 73% of 44 patients (Williams and Lees 2005). The prevalence of hallucinations in DLB is thus similar to that observed in PD with dementia. Hallucinations in DLB have the same phenomenological characteristics as those observed in PD (Mosimann et al. 2006; Nagahama et al. 2007). As in PD, a feeling of presence is often associated. However, hallucinations may develop early in the disease course and may even be present at onset (Tiraboschi et al. 2006). The mechanisms of hallucinations in DLB are likely to be similar to those involved in PD, although pharmacological factors probably play a lesser part.
8.3 Other Neurodegenerative Diseases
8.3.1 Non-Lewy-Body Parkinsonism
Hallucinations have rarely been studied in parkinsonian disorders other than PD and DLB (multiple system atrophy, progressive supranuclear palsy, corticobasal degeneration), so it is difficult to estimate their frequency. Available data suggest that hallucinations are rarely present in patients with non-Lewy body parkinsonism (about 10% in cross-sectional and clinical-pathological studies) (Williams and Lees 2005). One noteworthy exception is atypical Guadelupean parkinsonism, a condition which has two distinct phenotypes (a progressive supranuclear palsy-like syndrome and a parkinsonism-dementia syndrome), and which is associated with high intake of fruits or leaves rich in annonaceous neurotoxins. Hallucinations are present in 55% of subjects with Guadelupean parkinsonism. They are usually complex visual hallucinations (vivid animals, faces, people who were deceased) or occasionally auditory (Lannuzel et al. 2007).
8.3.2 Huntington’s Disease and Fronto-Temporal Dementias
Although behavioural and psychiatric disorders are common in the course of Huntington’s disease, hallucinations are rare: visual or auditory hallucinations were present in only 1.3% of 960 patients, of whom 0.2% reported tactile hallucinations and 0.3% other types of hallucination (Marder et al. 2000). In the same sample, delusions were present in 5.4% of cases. Interestingly, a subset of Huntington’s disease patients develops schizophrenia-like psychosis, with familial aggregation of psychotic symptoms suggesting the existence of genetic predisposing factors (Tsuang et al. 2000). Hallucinations are also rare in patients with fronto-temporal dementias (0–2%, Mendez et al. 2008), with the exception of progranulin mutation carriers, in whom hallucinations were present in 25% of patients in one series (Le Ber et al. 2008).
8.3.3 Alzheimer’s Disease
In Alzheimer’s disease, hallucinations are rarer than delusions. In a systematic review of 55 studies, most of which were cross-sectional, the mean prevalence rates of hallucinations and delusions were respectively 18% (range 4–41%) and 36% (range: 9.3–63%) (Ropacki and Jeste 2005). However, as in PD, the cumulative prevalence is reported to be higher in prospective studies of subjects with new-onset Alzheimer’s disease, increasing with the duration of the disease, to reach 51% at 4 years (Paulsen et al. 2000).
The phenomenology of hallucinations has rarely been studied in Alzheimer’s disease (Holroyd 1998). The hallucinations are mainly of a visual nature (people, animals and objects, in decreasing order of frequency) and less frequently auditory (ranging from conversations to noises). Olfactory hallucinations are rarely reported. The persistence of hallucinations in individual patients is variable. It should be emphasized that hallucinations may be more difficult to assess as the dementia progresses. Follow-up studies show that hallucinations are associated with poorer outcome, i.e. more rapid cognitive and functional decline, and with a higher risk of institutionalization and death (Scarmeas et al. 2005; Wilson et al. 2006). The most consistent factor related to psychosis (i.e. hallucinations and/or delusions) is the severity of cognitive impairment, as assessed with the Mini-Mental State Examination or other global cognitive measurements: more severe cognitive impairment is associated with a higher prevalence of hallucinations (Ropacki and Jeste 2005). Data on possible associations between hallucinations and other demographic or clinical variables, including age, age at onset and the duration of Alzheimer’s disease, are equivocal. Longitudinal studies aimed at identifying factors predictive of hallucinations are rare. In a follow-up study of 329 patients, the severity of cognitive impairment, the rate of cognitive decline and parkinsonism were predictive of the onset of hallucinations and delusions (Paulsen et al. 2000). In patients with pathologically confirmed Alzheimer’s disease, cortical Lewy bodies are associated with more persistent and severe hallucinations (McShane et al. 1995).
The mechanisms of hallucinations in Alzheimer’s disease are largely unknown, as is their relation to those postulated in PD and DLB. Abnormal sensory processing in the visual cortices (Holroyd and Sheldon-Keller 1995), together with altered top–down modulation of visual perception, may be involved. There is also growing evidence that psychosis (including hallucinations) in Alzheimer’s disease aggregates within families, suggesting that unidentified genetic factors may be involved (DeMichelle-Sweet and Sweet 2010).
9 Conclusion
Hallucinations and related phenomena such as illusions occur during the course of many neurological disorders and are a common consequence of sensory loss. There is a need for validated specific screening tools and rating scales. Although visual hallucinations predominate, the phenomenology is rich, and different types of hallucinations or related phenomena may be seen in combination. Insight into the hallucinatory nature of the perceptions is usually preserved and the emotional impact is generally limited. However, insight may be lost, especially in patients with cognitive impairment. Moreover, in some neurodegenerative diseases (PD and Alzheimer’s disease), hallucinations are predictors of poorer outcome, with a higher risk of nursing-home placement and death. The mechanisms of hallucinations resulting from neurological disorders or sensory loss are only partly understood. Hallucinations seem to result from abnormal activation of cortical areas involved in normal sensory processing, but this activation may be due to a variety of mechanisms that are not mutually exclusive.
Abbreviations
- CBS:
-
Charles Bonnet syndrome
- DLB:
-
Dementia with Lewy bodies
- fMRI:
-
Functional magnetic resonance imaging
- PD:
-
Parkinson’s disease
- PET:
-
Positron emission tomography
- REM sleep:
-
Rapid eye movement sleep
References
Aleci, C., & Liboni, W. (2009). Perceptive aspects of visual aura. Neurological Sciences, 30, 447–452.
Aleman, A., & Larøi, F. (2008). Hallucinations. The science of idiosyncratic perception. Washington, DC: American Psychological Association.
Arnulf, I., Bonnet, A.-M., Damier, P., Bejjani, B. P., Seilhean, D., Derenne, J. P., et al. (2000). Hallucinations, REM sleep, and Parkinson’s disease. A medical hypothesis. Neurology, 55, 281–288.
Baier, B., de Haan, B., Mueller, N., Thoemke, F., Birklein, F., Dieterich, M., et al. (2010). Anatomical correlate of positive spontaneous visual phenomena. A voxelwise lesion study. Neurology, 74, 218–222.
Benke, T. (2006). Peduncular hallucinosis. A syndrome of impaired reality monitoring. Journal of Neurology, 253, 1561–1571.
Berrios, G. E. (1985). Hallucinosis. In J. A. M. Fredriks (Ed.), Handbook of clinical neurology (Neurobehavioral disorders, Vol. 2). Amsterdam: Elsevier.
Berrios, G. E. (1990). Musical hallucinations. A historical and clinical study. The British Journal of Psychiatry, 156, 188–194.
Bien, C. G., Benninger, F. O., Urbach, H., Schramm, J., Kurthen, M., & Elger, C. E. (2000). Localizing value of epileptic visual auras. Brain, 123, 244–253.
Billiard, M., Besset, A., & Cadilhac, J. (1983). The clinical and polygraphic development of narcolepsy. In C. Guilleminault & E. Lugaresi (Eds.), Sleep/wake disorders: Natural history, epidemiology, and long-term evolution (pp. 171–185). New York: Raven Press.
Billiard, M., Jaussent, I., Dauvilliers, Y., & Besset, A. (2011). Recurrent hypersomnia: a review of 339 cases. Sleep Medicine Reviews, 15, 247–257.
Blanke, O., Landis, T., Spinelli, L., & Seeck, M. (2004). Out-of-body experience and autoscopy of neurological origin. Brain, 127, 243–258.
Blanke, O., & Metzinger, T. (2009). Full-body illusions and minimal phenomenal selfhood. Trends in Cognitive Sciences, 13, 7–13.
Blanke, O., & Mohr, C. (2005). Out-of-body experience, heautoscopy, and autoscopic hallucination of neurological origin. Implications for neurocognitive mechanisms of corporeal awareness and self-consciousness. Brain Research Reviews, 50, 184–199.
Braun, C. M. J., Dumont, M., Duval, J., Hamel-Hébert, I., & Godbout, L. (2003). Brain modules of hallucinations: An analysis of multiple patients with brain lesions. Journal of Psychiatry & Neuroscience, 28, 432–449.
Burke, W. (2002). The neural basis of Charles Bonnet hallucinations: A hypothesis. Journal of Neurology, Neurosurgery, and Psychiatry, 73, 535–541.
Charles, A. (2009). Advances in the basic and clinical science of migraine. Annals of Neurology, 65, 491–498.
Cogan, D. G. (1973). Visual hallucinations as release phenomena. Graeffe’s Archive for Clinical and Experimental Ophtalmology, 188, 139–150.
Cole, M. G., Dowson, L., Dendukuri, N., & Belzile, E. (2002). The prevalence and phenomenology of auditory hallucinations among elderly subjects attending an auditory clinic. International Journal of Geriatric Psychiatry, 17, 444–452.
Collerton, D., & Perry, E. (2011). Dreaming and hallucinations—Continuity or discontinuity? Perspectives from dementia with Lewy bodies. Consciousness and Cognition, 20(4), 1016–1020.
Collerton, D., Perry, E., & McKeith, I. (2005). Why people see things that are not there: A novel Perception and Attention Deficit model for recurrent complex visual hallucinations. The Behavioral and Brain Sciences, 28, 737–757.
Cooke, M. A., Peters, E. R., Fanon, D., Aasen, I., Kuipers, E., & Kumari, V. (2010). Cognitive insight in psychosis: The relationship between self-certainty and self-reflection dimensions and neuropsychological measures. Psychiatry Research, 178, 284–289.
Dauvilliers, Y., Arnulf, I., & Mignot, E. (2007). Narcolepsy with cataplexy. Lancet, 369, 499–511.
DeMichelle-Sweet, M. A., & Sweet, R. A. (2010). Genetics of psychosis in Alzheimer’s disease: A review. Journal of Alzheimer’s Disease, 19, 761–780.
Diederich, N. J., Fénelon, G., Stebbins, G., & Goetz, C. G. (2009). Hallucinations in Parkinson disease. Nature Reviews. Neurology, 5, 331–342.
Diederich, N. J., Goetz, C. G., & Stebbins, G. T. (2005). Repeated visual hallucinations in Parkinson’s disease as disturbed external/internal perceptions: Focused review and a new integrative model. Movement Disorders, 20, 130–140.
Eliott, B., Joyce, E., & Shorvon, S. (2009a). Delusions, illusions and hallucinations in epilepsy: 1. Elementary phenomena. Epilepsy Research, 85, 162–171.
Eliott, B., Joyce, E., & Shorvon, S. (2009b). Delusions, illusions and hallucinations in epilepsy: 2. Complex phenomena and psychosis. Epilepsy Research, 85, 172–186.
Evans, R. W., & Rolak, L. A. (2004). The Alice in wonderland syndrome. Headache, 44, 624–625.
Evers, S., & Ellger, T. (2004). The clinical spectrum of musical hallucinations. Journal of the Neurological Sciences, 227, 55–65.
Fénelon, G. (2010). Hallucinations in Parkinson’s disease. In F. Larøi & A. Aleman (Eds.), Hallucinations. A guide to treatment and management (pp. 361–375). Oxford: Oxford University Press.
Fénelon, G., & Alves, G. (2010). Epidemiology of psychosis in Parkinson’s disease. Journal of the Neurological Sciences, 289, 12–17.
Fénelon, G., & Hamdani, N. (2010). Hallucinations in neuropsychiatry and drug abuse: From phenomenology to pathophysiology. In G. F. Koob, M. Le Moal, & R. F. Thomson (Eds.), Encyclopedia of behavioural neuroscience (Vol. 2, pp. 6–11). Oxford: Academic.
Fénelon, G., Soulas, T., Cleret de Langavant, L., Trinkler, I., & Bachoud-Lévi, A.-C. (2011). Feeling of presence in Parkinson’s disease. Journal of Neurology, Neurosurgery, and Psychiatry, 82(11), 1219–1224.
Fernandez, H. H., Aarsland, D., Fénelon, G., Friedman, J. H., Marsh, L., Tröster, A. I., et al. (2008). Scales to assess psychosis in Parkinson’s disease: Critique and recommendations. Movement Disorders, 23, 484–500.
ffytche, D. H. (2007). Visual hallucinatory syndromes: Past, present, and future. Dialogues in Clinical Neuroscience, 9, 173–189.
ffytche, D. H. (2008). The hodology of hallucinations. Cortex, 44, 1067–1083.
ffytche, D. H. (2009). Visual hallucinations in eye disease. Current Opinion in Neurology, 22, 28–35.
ffytche, D. H., & Howard, R. J. (1999). The perceptual consequences of visual loss: “Positive” pathologies of vision. Brain, 122, 1247–1260.
ffytche, D. H., Howard, R. J., Brammer, M. J., David, A., Woodruff, P., & Williams, S. (1998). The anatomy of conscious vision: An fMRI study of visual hallucinations. Nature Neuroscience, 1, 738–742.
Flor, H., Nikolajsen, L., & Jensen, T. S. (2006). Phantom limb pain: A case of maladaptative CNS plasticity? Nature Reviews. Neuroscience, 7, 873–881.
Fortuyn, H. A., Lappenschaar, G. A., Nienhuis, F. J., Furer, J. W., Hodiamont, P. P., Rijnders, C. A., et al. (2009). Psychotic symptoms in narcolepsy: Phenomenology and a comparison with schizophrenia. General Hospital Psychiatry, 31, 146–154.
Gold, K., & Rabins, P. V. (1989). Isolated visual hallucinations and the Charles Bonnet syndrome: A review of the literature and presentation of six cases. Comprehensive Psychiatry, 30, 90–98.
Griffith, T. D. (2000). Musical hallucinosis in acquired deafness. Phenomenology and brain substrate. Brain, 123, 2065–2076.
Hadjikhani, N., Sanchez del Rio, M., Wu, O., Schwartz, D., Bakker, D., Fischl, B., et al. (2001). Mechanisms of migraine aura revealed by functional MRI in human visual cortex. Proceedings of the National Academy of Sciences of the United States of America, 98, 4687–4692.
Hécaen, H., & Ropert, H. (1963). Les hallucinations auditives des otopathes. Journal de Psychologie Normale et Pathologique, 60, 293–323.
Hobson, J. A. (2009). REM sleep and dreaming: Towards a theory of protoconsciousness. Nature Reviews. Neuroscience, 10, 803–813.
Holroyd, S. (1998). Hallucinations and delusions in Alzheimer’s disease. In B. Vellas, J. Fitten, & G. Fresoni (Eds.), Research and practice in Alzheimer’s disease (pp. 213–222). Paris: Serdi.
Holroyd, S., & Rabins, P. V. (1996). A three-year follow-up study of visual hallucinations in patients with macular degeneration. The Journal of Nervous and Mental Disease, 184, 188–189.
Holroyd, S., & Sheldon-Keller, A. (1995). A study of visual hallucinations in Alzheimer’s disease. The American Journal of Geriatric Psychiatry, 3, 198–205.
Jackson, H. J. (1931). Selected writings of John Hughlings Jackson (Vol. 1) (J. Taylor, G. Holmes, & F. M. R. Walshe, Eds.). London: Hodder and Stoughton.
Kasper, B. S., Kasper, E. M., Pauli, E., & Stefan, H. (2010). Phenomenology of hallucinations, illusions, and delusions as part of seizure semiology. Epilepsy & Behavior, 18, 13–23.
Khan, J. C., Shahid, H., Thurlby, D. A., Yates, J. R., & Moore, A. T. (2008). Charles Bonnet syndrome in age-related macular degeneration: The nature and frequency of images in subjects with end-stage disease. Ophthalmic Epidemiology, 15, 202–208.
Kolmel, H. W. (1985). Complex visual hallucinations in the hemianopic field. Journal of Neurology, Neurosurgery, and Psychiatry, 48, 29–38.
Lannuzel, A., Höglinger, G. U., Verhaeghe, S., Gire, L., Belson, S., Escobar-Khondiker, M., et al. (2007). Atypical parkinsonism in Guadeloupe: A common risk factor for two closely related phenotypes? Brain, 130, 816–827.
Le Ber, I., Camuzat, A., Hannequin, D., Pasquier, F., Guedj, E., Rovelet-Lecrux, A., et al. (2008). Phenotype variability in progranulin mutation carriers: A clinical, neuropsychological, imaging and genetic study. Brain, 131, 732–746.
Leu-Semenescu, S., Cochen de Cock, V. C., Dauriac le Masson, V. D., Debs, R., Lavault, S., Roze, E., et al. (2011). Hallucinations in narcolepsy with and without cataplexy: Contrasts with Parkinson’s disease. Sleep Medicine, 12, 497–504.
Lewis-Hanna, L. L., Hunter, M. D., Farrow, T. F. D., Wilkinson, I. D., & Woodruff, P. W. R. (2011). Enhanced cortical effects of auditory stimulation and auditory attention in healthy individuals prone to auditory hallucinations during partial wakefulness. NeuroImage, 57, 1154–1161.
Lhermitte, J. (1932). L’hallucinose pédonculaire. Encephale, 27, 422–435.
Lhermitte, J. (1951). Les hallucinations. Clinique et physiopathologie. Paris: Doin.
Mahowald, M. W., & Schenck, C. H. (2001). Evolving concepts of human state dissociation. Archives Italiennes de Biologie, 139, 269–300.
Manford, M., & Andermann, F. (1998). Complex visual hallucinations. Clinical and neurobiological insights. Brain, 121, 1819–1840.
Manni, R., Terzhagi, M., Ratti, P.-L., Repetto, A., Zangaglia, R., & Pacchetti, C. (2011). Hallucinations and REM sleep behaviour disorder in Parkinson’s disease: Dream imagery intrusions and other hypotheses. Consciousness and Cognition, 20(4), 1021–1026.
Marder, K., Zhao, H., Myers, R. H., Cudkowicz, M., Kayson, E., Kieburtz, K., et al. (2000). Rate of functional decline in Huntington’s disease. Neurology, 54, 452–458.
Matsui, T., Matsunaga, H., Ohya, K., Iwasaki, Y., Koshimune, K., Miyata, A., et al. (2002). Clinical features in two cases with musical obsessions who successfully responded to clomipramine. Psychiatry and Clinical Neurosciences, 57, 47–51.
Mauguière, F. (1999). Scope and presumed mechanisms of hallucinations in partial epileptic seizures. Epileptic Disorders, 1, 81–91.
Maury, A. (1861). Le Sommeil et les Rêves. Etudes Psychologiques sur ces Phénomènes et les Divers Etats qui s’y Rattachent. Paris: Didier.
McKeith, I. G. (2002). Dementia with Lewy bodies. The British Journal of Psychiatry, 180, 144–147.
McKeith, I. G., Dickson, D. W., Lowe, J., Emre, M., O’Brien, J. T., Feldman, H., et al. (2005). Diagnosis and management of dementia with Lewy bodies: Third report of the DLB Consortium. Neurology, 65, 1863–1872.
McShane, R., Gedling, K., Reading, M., McDonald, B., Esiri, M. M., & Hope, T. (1995). Prospective study of relations between cortical Lewy bodies, poor eyesight, and hallucinations in Alzheimer’s disease. Journal of Neurology, Neurosurgery, and Psychiatry, 59, 185–188.
Melzack, R. (1990). Phantom limbs and the concept of a neuromatrix. Trends in Neurosciences, 13, 88–92.
Mendez, M. F., Shapira, J. S., Woods, R. J., & Licht, E. A. (2008). Psychotic symptoms in frontotemporal dementia: Prevalence and review. Dementia and Geriatric Cognitive Disorders, 25, 206–211.
Menon, G. J. (2003). Complex visual hallucinations in the visually impaired: The Charles Bonnet syndrome. Survey of Ophthalmology, 48, 58–72.
Menon, G. J. (2005). Complex visual hallucinations in the visually impaired. A structured history-taking approach. Archives of Ophthalmology, 123, 349–355.
Merabet, L. B., Kobayashi, M., Baron, J., & Pascal-Leone, A. (2003). Suppression of complex visual hallucinatory experiences by occipital transcranial magnetic stimulation: A case report. Neurocase, 9, 436–440.
Mosimann, U. P., Rowan, E. N., Partington, C. E., Collerton, D., Littlewood, E., O’Brien, J. T., et al. (2006). Characteristics of visual hallucinations in Parkinson’s disease dementia and dementia with Lewy bodies. The American Journal of Geriatric Psychiatry, 14, 153–160.
Nagahama, Y., Okina, T., Suzuki, N., Matsuda, M., Fukao, K., & Murai, T. (2007). Classification of psychotic symptoms in dementia with Lewy bodies. The American Journal of Geriatric Psychiatry, 15, 961–967.
Nelson, P. T., Jicha, G. A., Kryscio, R. J., Abner, E. L., Schmitt, F. A., Cooper, G., et al. (2010). Low sensitivity in clinical diagnoses of dementia with Lewy bodies. Journal of Neurology, 257, 359–366.
Nir, Y., & Tononi, G. (2010). Dreaming and the brain: From phenomenology to neurophysiology. Trends in Cognitive Sciences, 14, 88–100.
Ohayon, M. M. (2000). Prevalence of hallucinations and their pathological associations in the general population. Psychiatry Research, 97, 153–164.
Ohayon, M. M., Priest, R. G., Caulet, M., & Guilleminault, C. (1996). Hypnagogic and hypnopompic hallucinations: Pathological phenomena? The British Journal of Psychiatry, 169, 459–467.
Panayiotopoulos, C. P. (1999). Elementary visual hallucinations, blindness, and headache in idiopathic occipital epilepsy: Differentiation from migraine. Journal of Neurology, Neurosurgery, and Psychiatry, 66, 536–540.
Paquier, P., van Vugt, P., Bal, P., Cras, P., Parizel, P. M., van Haesendonck, J., et al. (1992). Transient musical hallucinosis of central origin: A review and clinical study. Journal of Neurology, Neurosurgery, and Psychiatry, 55, 1069–1073.
Paulsen, J. S., Salmon, D. P., Thal, L. J., Romero, R., Weisstein-Jenkins, C., Galasko, D., et al. (2000). Incidence of and risk factors for hallucinations and delusions in patients with probable AD. Neurology, 54, 1965–1971.
Penfield, W., & Perot, P. (1963). The brain’s record of auditory and visual experience. Brain, 86, 595–696.
Pietrobon, D., & Striessnig, J. (2003). Neurobiology of migraine. Nature Reviews. Neuroscience, 4, 386–398.
Raggi, A., Cosentino, F. I. I., Lanuzza, B., & Ferri, R. (2010). Behavioural and neurophysiologic features of state dissociation: A brief review of the literature and three descriptive case studies. Behavioural Neurology, 22, 91–99.
Ramachandran, V. S., & Hirstein, W. (1998). The perception of phantom limbs. Brain, 121, 1603–1630.
Ravina, B., Marder, K., Fernandez, H. H., Friedman, J. H., McDonald, W., Murphy, D., et al. (2007). Diagnostic criteria for psychosis in Parkinson’s disease: Report of an NINDS/NIMH Work Group. Movement Disorders, 22, 1061–1068.
Ropacki, S. A., & Jeste, D. V. (2005). Epidemiology of and risk factors for psychosis of Alzheimer’s disease: A review of 55 studies published from 1990 to 2003. The American Journal of Psychiatry, 162, 2022–2030.
Russel, M. B., & Olesen, J. (1996). A nosographic analysis of the migraine aura in a general population. Brain, 119, 355–361.
Scarmeas, N., Brandt, J., Albert, M., Hadjigeorgiou, G., Papadimitriou, A., Dubois, B., et al. (2005). Delusions and hallucinations are associated with worse outcome in Alzheimer’s disease. Archives of Neurology, 62, 1601–1608.
Stewart, L., von Kriegstein, K., Warren, J. D., & Griffiths, T. D. (2006). Music and the brain: Disorders of musical listening. Brain, 129, 2533–3553.
Teunisse, R. J., Cruysberg, J. R., Hoefnagels, W. H., Verbeek, A. L., & Zitman, F. G. (1996). Visual hallucinations in psychologically normal people: Charles Bonnet’s syndrome. Lancet, 347, 794–797.
Tfelt-Hansen, P. C. (2010). History of migraine with aura and cortical spreading depression from 1941 and onwards. Cephalalgia, 30, 780–792.
Tiraboschi, P., Salmon, D., Hansen, L. A., Hofstetter, R. C., Thal, L. J., & Corey-Bloom, J. (2006). What best differentiates Lewy body from Alzheimer’s disease in early-stage dementia? Brain, 129, 729–735.
Tsuang, D., Almqvist, E. W., Lipe, H., Strgar, F., DiGiacomo, L., Hoff, D., et al. (2000). Familial aggregation of psychotic symptoms in Huntington’s disease. The American Journal of Psychiatry, 157, 1955–1959.
van der Zward, R., & Polak, M. A. (2001). Pseudohallucinations: A pseudoconcept? A review of the validity of the concept, related to associate symptomatology. Comprehensive Psychiatry, 42, 42–50.
Vaphiades, M. S., Celesia, G. G., & Brigell, M. G. (1996). Positive spontaneous visual phenomena limited to the hemianopic field in lesions of central visual pathways. Neurology, 47, 408–417.
Vignal, J.-P., Maillard, L., McGonigal, A., & Chauvel, P. (2007). The dreamy state: Hallucinations of autobiographic memory evoked by temporal stimulations and seizures. Brain, 130, 88–99.
Weidenfeld, A., & Borusiak, P. (2011). Alice-in-wonderland syndrome—A case-based update and long-term outcome in nine children. Child’s Nervous System, 27 (6), 893–896.
West, L. J. (1962). Hallucinations. New York: Grune & Stratton.
Wilkinson, F. (2004). Auras and other hallucinations: Windows on the visual brain. Progress in Brain Research, 144, 305–320.
Williams, D. R., & Lees, A. J. (2005). Visual hallucinations in the diagnosis of idiopathic Parkinson’s disease: A retrospective autopsy study. Lancet Neurology, 4, 605–610.
Wilson, R. S., Tang, Y., Aggarwal, N. T., Gilley, D. W., McCann, J. J., Bienias, J. L., et al. (2006). Hallucinations, cognitive decline, and death in Alzheimer’s disease. Neuroepidemiology, 26, 68–75.
Wunderlich, G., Suchan, B., Volkmann, J., Herzog, H., Hömberg, V., & Seitz, R. J. (2000). Visual hallucinations in recovery from cortical blindness. Imaging correlates. Archives of Neurology, 57, 561–565.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Fénelon, G. (2013). Hallucinations Associated with Neurological Disorders and Sensory Loss. In: Jardri, R., Cachia, A., Thomas, P., Pins, D. (eds) The Neuroscience of Hallucinations. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-4121-2_4
Download citation
DOI: https://doi.org/10.1007/978-1-4614-4121-2_4
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-4120-5
Online ISBN: 978-1-4614-4121-2
eBook Packages: MedicineMedicine (R0)