Abstract
Herein, we describe our approach to robotic mitral valve repair. We now use the trans-thoracic cross clamp to arrest the heart. Using robotic techniques, we have used both traditional and modified repair methods with excellent outcomes. We describe the entire operative process including patient positioning, anesthesia, robotic arm trocar placement, cardiopulmonary perfusion, aortic occlusion, cardioplegia, and execution of the robotic mitral valve repair. Operative tips and pitfalls are included as well as details of our repair results.
Similar content being viewed by others
Keywords
Introduction
The reliability, durability, and superiority of mitral valve repair compared to valve replacement for degenerative mitral valve disease is well established [1–3]. Today, catheter-based mitral valve repair techniques are being developed clinically to provide a less invasive approach, which is more acceptable to patients. However, the long-term effectiveness of catheter-based methods to treat structural mitral valve dysfunction remains unproven. Thus, surgical mitral repair still remains the “gold standard” for patients with degenerative mitral valve regurgitation. Early minimally invasive surgical approaches were hampered by compromised exposure and limited instrument dexterity. The development of robotic technology with magnified 3-D vision and enhanced ergonomic instrument dexterity has overcome many of these limitations [4–6]. Mitral valve repairs now can be performed as a totally endoscopic procedure with a very high success rate and reproducibility [7–11]. Moreover, the quality of life following a robotic mitral repair has been shown to be excellent [12].
Our technique does not require a “mini” thoracotomy, but rather employs a small (15-mm) soft rubber port that serves as a “working” or “access” port. Using the least invasive robotic assistance, we now are able to employ conventional mitral valve repair techniques with excellent early outcomes. These proven techniques should obtain the same excellent long-term results as with the sternotomy approach. These methods have included leaflet resections with sliding-plastys, PTFE (Gore-Tex™—W.L. Gore & Assoc. Inc, Flagstaff, AZ) neo-chordae replacements to both anterior and posterior leaflets, and implantation of either flexible or rigid annuloplasty rings.
One challenge inherent during totally endoscopic mitral valve repairs is safe aortic occlusion and ideal cardioplegia delivery. While excellent results can be obtained with balloon catheter endoaortic occlusion and antegrade cardioplegia delivery, this technique requires considerable operator training, experience, and a significant increase in procedural cost [9, 10]. We have developed a simple robot-assisted endoscopic modification of the direct aortic cross clamp technique popularized by Chitwood and coworkers [5–7]. We place the “Chitwood” trans-thoracic cross-clamp (Scanlan International Inc, St. Paul, MN) via a small incision in the posterior axilla. The clamp is positioned across the aorta under visual guidance from the robotic system. For antegrade cardioplegia delivery we introduce an angio-catheter through the chest wall and into the aorta directly. The excellent visualization and instrument dexterity provided by the daVinci™ robotic system enables endoscopic performance of both maneuvers, rather than relying on direct vision through a working thoracotomy and conventional instruments. A similar robotic approach is used for our atrial septal defect closures (ASD), atrial myxoma resections, cryo-maze ablations for atrial fibrillation and mitral valve replacements.
Anesthesia and Patient Positioning
Anesthetic management begins with the spinal administration of a single dose of long acting morphine. When combined with direct local anesthetic injections, this regimen minimizes early post-operative port incision and pleural pain. Either a left radial or femoral artery catheter is inserted for hemodynamic monitoring and blood sample access. After anesthesia induction, the patient is intubated with a double lumen endotracheal tube, and thereafter, a transesophageal echo (TEE) probe is inserted. Then, under TEE guidance, an EndoPlege™ retrograde coronary sinus cardioplegia catheter (Edwards Lifesciences, Irvine, CA) is passed via the internal jugular vein with the final position confirmed by contrast fluoroscopy. In selected cases we place an Endo-Vent™ pulmonary artery vent catheter (Edwards Lifesciences, Irvine, CA) to assist with cardiac drainage and measure pulmonary artery pressures.
The patient is positioned at the extreme right edge of the operating table (Fig. 21.1). A transverse roll is placed under the mid-chest, and the right arm is positioned just below the table edge and is supported in a padded sling. This position allows access to the entire right lateral chest wall. The patient then is rotated leftward to facilitate right lateral chest wall access.
Patient position: the patient is placed on the operating table with the right side shifted to the edge. The right arm is placed below the operating table and is suspended using a “sheet sling”. A towel roll is placed behind the right shoulder for slight elevation. The robot instrument cart is placed on the left side of the patient with the instrument arms and camera “reaching over” to enter the right side of the thorax
Instrument Port Placement
Robotic instrument ports are placed after a long acting local anesthetic is administered (Fig. 21.2). First, the endoscopic camera port is placed lateral to the patient’s nipple in the right fourth intercostal space. In women this port incision is placed just above the infra-mammary crease with the breast distracted superiorly so that the port enters either the fourth or fifth intercostal space. Carbon dioxide is insufflated continuously via the camera port into the thorax at 6 L/min and 8 Torr of pressure. After the camera is introduced, the inter-thoracic environment is examined to determine the presence of adhesions and to be sure that is suitably positioned.
Instrument port placement: this illustration shows placement of the left and right robot instrument port trocars (third and fifth to sixth ICS). The trans-thoracic clamp is shown in the third intercostal space (ICS) at the posterior axillary line. A small sump sucker is passing into the left atrium via the clamp incision. The working port is shown in the fourth ICS. The camera port (fourth ICS) has the CO2 insufflation line attached. The trocar that is most medial is for the retractor arm
A 2.5-cm incision is made along the anterior axillary line and carried posteriorly in the fourth intercostal space. This incision accommodates a 15-mm soft rubber thoracoport (Ethicon Endo-Surgery Inc, Cincinnati, OH) that functions as a “working port” for the surgical assistant to access the operative site. To retrieve pericardial traction sutures safely, we place a finger through the “working port” incision and pass an angiocatheter one interspace lower in the mid axillary line. Thereafter, trans-thoracic pericardial retraction sutures are pulled through the angiocatheter and anchored. Guided by a finger in the “working port”, a Chitwood trans-thoracic aortic crossclamp (Scanlan International Inc, St. Paul, MN) is introduced in the same interspace as the camera and working ports via a small mid-axillary line incision. We then introduce a suction catheter beside the clamp for left atrial pulmonary venous drainage. This is very important to maintain continuous blood-free visualization. Thereafter, the left robotic instrument trocar is placed in the third interspace, equidistant between the camera port and the shoulder, under “working port” finger guidance. The atrial retractor trocar is placed in either the fifth or sixth interspace as medially as possible. Next, the right instrument cannula is placed, under endoscopic visual guidance, along the anterior axillary line (‘working port’ level) and just cephalad to the diaphragmatic chest wall attachment. This position usually is three to four intercostal spaces caudal to the working port. By placing this port inferiorly, greater separation of the two right instrument arms decreases potential external instrument arm conflicts. The right instrument cannula retracts diaphragm inferiorly, facilitating unobstructed instrument exchanges and obviating the need for a diaphragm retraction suture.
Cardiopulmonary Bypass
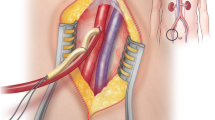
The right femoral artery and vein are exposed for cannulation via a small transverse incision placed just cephalad to the groin crease (Fig. 21.3). Using the Seldinger guide-wire technique and under trans-esophageal direction, a femoral venous cannula (either 25-Fr Quickdraw™ Venous Cannula, Edwards Lifesciences, Irvine, CA or BioMedicus™ Multi-stage Femoral Venous Cannula, Medtronic, Minneapolis, MN) is inserted via an anterior surface purse-string suture and passed the length of the inferior vena cave (IVC). Then it is passed through the right atrium so that the distal end resides several centimeters in the superior vena cava (SVC) (Fig. 21.4). If this cannula is positioned appropriately excellent venous drainage ensues, obviating the need for separate SVC cannulation. For operations requiring an open right atrium, a separate internal jugular cannula is passed into the SVC. The femoral artery is cannulated via a transverse arteriotomy, which is later repaired by direct suture closure. Cardiac drainage may be aided by a pulmonary artery vent that has been placed percutaneously. When needed, retrograde cardioplegia can be infused via an EndoPlege™ retrograde coronary sinus catheter.
Femoral artery and vein cannulation: this illustration shows arterial and venous cannulas that are used for cardiopulmonary perfusion. The venous cannula passes through the right femoral vein (distant cannula), into and through the superior vena cava and into the superior vena cava. The arterial cannula is shown in the foreground. All cannula insertions are done using the Seldinger guide-wire method under echocardiographic direction
Position of intra-cardiac cannulas: the femoral venous cannula is shown after it has passed through the right atrium and into the SVC. The balloon tipped retrograde coronary sinus catheter has been inserted via the right internal jugular vein and directed into the mid-sinus for cardioplegia administration via SVC. A pulmonary artery vent has been passed via the right internal jugular vein
Thereafter, the daVinci™ surgical cart is docked to instrument and camera trocars, followed by introduction of surgical instruments. If there is significant pericardial fat, it is removed at this time using a robotic electrocautery instrument. To maintain sufficient intra-thoracic CO2 pressure, which helps to provide an adequate “working space”, the assistant can hand cover thoracoports. After cardiac decompression and suspension of respiratory motion with the initiation of cardiopulmonary bypass, mediastinal displacement provides much more working space. Vacuum-assisted venous drainage is used to optimize pump return and cardiac decompression.
Cardiac Exposure, Aortic Occlusion, and Myocardial Protection
To extract pericardial retraction sutures over the aorta, an angiocatheter is passed through the anterior chest wall, avoiding the internal thoracic vessels. Following femoral cannulation for cardiopulmonary perfusion, the daVinci™ instrument cart is “docked” at the operating table, followed by camera and instruments insertion. After cardiopulmonary bypass is established with systemic cooling to 30 °C, the pericardium is opened 3–4 cm anterior to the phrenic nerve with Endowrist™ curved scissors or electrocautery (Intuitive Surgical, Mountain View, CA), and the pericardiotomy is extended to the aortic reflection (Fig. 21.5). Two traction sutures are placed along the posterior pericardium, and using a “crochet hook”, distracted laterally via a trans-thoracic angiocatheter and through the chest wall. To improve aortic exposure for cross-clamp positioning, a third pericardial traction suture is carried through the anterior chest wall. Here, care must be taken to avoid injury to the internal thoracic vessels. To prepare for the left atriotomy, the oblique sinus is opened behind the IVC, and the inter-atrial grove is dissected slightly using the robotic electrocautery (Fig. 21.6).
Pericardiotomy and retraction sutures. (a) After cardiopulmonary bypass has been established the pericardium is opened anterior to the phrenic nerve using the robotic electrocautery instrument. (b) The pericardial incision is carried cephalad to the aortic reflection. Care must be taken to avoid phrenic nerve injury by keeping this incision directed toward anterior surface of the aorta. (c) Cardiac exposure for a robotic mitral valve repair is developed using pericardial retraction sutures placed in the lateral edge and for retraction brought through the chest wall via angiocatheters. A third retraction suture is placed through the pericardial edge anterior the aorta and pulled through the anterior chest wall, avoiding internal thoracic vessels. Retraction of the anterior pericardium facilitates trans-thoracic aortic clamping
Inter-atrial groove dissection: prior to opening the left atrium and at the level of the right superior pulmonary vein, the fatty interatrial groove is dissected with the robotic electrocautery. At the same time the oblique sinus behind the IVS should be exposed. Both dissections help obviate both pulmonary vein injury and right atrial entry during the left atriotomy
Subsequently, the Chitwood aortic cross-clamp is positioned across the aorta (Fig. 21.7). To do this safely, the console surgeon exposes the transverse sinus with robotic instruments, while the patient-side assistant positions one arm of the clamp through the sinus (posterior to the aorta) and the other arm anteriorly. The endoscopic camera provides superb visualization of the right pulmonary artery and left atrial appendage, allowing careful clamp positioning with avoidance of structural injury.
Cross clamp deployment: the left robot instrument is lifting the aorta so that the posterior arm of the clamp can be passed through the transverse sinus safely. The right arm of the robot is also used to lift the aorta. Behind the aorta and near the tip the posterior clamp, the right pulmonary artery can be seen. In the distance the left atrial appendage should be visualized. Adequate visualization is the key to safe placement of the trans-thoracic aortic clamp. One should decrease pump flow during this maneuver
For antegrade cardioplegia administration, an angiocatheter (#14G, 5.5-in. with a small side-hole cut near the tip) is placed directly through the anterior chest wall (Fig. 21.8). The catheter should be aimed toward the aorta with care to avoid internal thoracic vessel injury. Thereafter, it is grasped with robotic instruments and directed visually just proximal to the cross-clamp and into the aortic root by the console surgeon. The stiff needle inside the angiocatheter may introduce unwanted “torque”. Therefore, the assistant should withdraw the needle just as the catheter tip crosses into the aortic lumen. The console surgeon may then advance an extra length of the now flexible catheter farther into the aorta before securing it to the skin and attaching the cardioplegia delivery system. Generally, it takes less than 10 min from the time cardiopulmonary bypass is initiated until aortic cross clamping and cardioplegia delivery. The ease and safety of the pericardiotomy, traction suture placement, inter-atrial groove dissection, and cross clamp positioning with decompressed heart easily justifies the few extra minutes of cardiopulmonary bypass time.
Cardioplegia catheter insertion and closure. (a) Using robotic visualization and instruments, the console surgeon directs the catheter that has been placed through the anterior chest wall into the proximal aortic root. (b) Following cardiac de-airing the catheter is removed and the entrance site closed with a pledgeted 4-0 PTFE suture. This illustration shows extracorporeal tying of this closure suture
After the cross clamp has been applied, the initial dose of antegrade cardioplegia is delivered via the aortic catheter. Generally, we give subsequent infusions via the retrograde coronary sinus catheter at 20-min intervals. However, if our anesthesiologist was unable to place the EndoPlege™ retrograde coronary sinus catheter (<10 % of the time), we infuse multi-dose antegrade cardioplegia, while visualizing the aortic root to be sure that there is adequate pressurization. At the conclusion the mitral valve repair, the aortic angiocatheter is removed and the entry site closed robotically with a pledget reinforced 4-0 PTFE suture (Fig. 21.8).
Robotic Mitral Valve Repair Techniques
Following cardiac arrest, the left atriotomy is performed using the Endowrist™ curved scissors (Fig. 21.9a). Thereafter, the Endowrist™ dynamic atrial retractor is positioned within the left atrium, elevating the inter-atrial septum, to provide mitral valve exposure (Fig. 21.9b). A “drop in” flexible cardiotomy suction catheter is placed in a dependent left pulmonary vein to help clear the operative field. Adjunctively, the assistant can use a straight rigid sucker to facilitate exposure and retraction. The console surgeon can reposition the retractor at any time to visualize the atrial septum (patent foramen ovale closure), the atrial appendage, or different mitral valve regions. We generally close the left atrial appendage in two-layers using 4-0 PTFE sutures (Fig. 21.10). Running sutures are “followed” using a long hook (ATS Medical Inc, Minneapolis, MN) with tension, maintained by the patient-side assistant. If the suture is too short to follow with the hook, it can be kept tight by passing the needle in and out of the working port. By using our “hook method”, the surgeon maintains needle possession and is always ready for each “bite”. This is much faster than passing the needle in and out of the chest for every tissue “bite”.
Left atriotomy and retractor placement. (a) The left atriotomy is made with the curved robot scissors and is carried toward the oblique sinus. Here, the left arm is holding up the edge of the right atrium for exposure. (b) Thereafter, the dynamic left atrial retractor is placed along the interatrial septum with lifting it for mitral valve exposure. A flexible sucker is shown in the left superior pulmonary vein to keep the atrium blood free
Left atrial appendage closure: this illustration shows the left atrial appendage being closed. The robotic needle driver (right) passes the needle through the appendage edges. Thereafter, the assistant uses a hook instrument, passed through the working port, to follow and tighten the suture. By following the suture in this manner, the closure line remains secure, and the console surgeon always retains the needle, speeding the closure
Both three dimensional (3-D) camera vision and Endowrist™ instrument dexterity facilitate precise manipulation of the mitral valve apparatus. All traditional repair techniques can be employed using our robotic approach. To assess the leaflet pathology, a robotic hook instrument is used, and resections are performed using robotic curved scissors. Early in our experience to repair posterior mitral leaflet pathology, we performed quadrangular resections with an annular plication. In recent years, we have preferred to preserve leaflet tissue either by performing triangular resections without an annular plication or by reducing any prolapse using PTFE (Gore-Tex™) neo-chords. However, in the presence of copious redundant posterior leaflet tissue, large leaflet resections with a sliding-plasty reconstruction can be performed using these techniques. Either (flexible or rigid) annuloplasty bands or a full ring can be implanted robotically.
A P2 triangular leaflet resection is illustrated in Fig. 21.11. After the resection, leaflets edges are approximated using a two-layer running 4-0 polypropylene suture. As described before, the patient-side assistant follows the sutures with the hook instrument and then hand ties them using a using a knot-pusher. When performing a sliding leaflet repair, a two-layer running 4-0 polypropylene suture material is used to reattach the leaflets to the annulus (Fig. 21.12). Gore-Tex™ neo-chords can be placed easily using robotic instruments. Papillary muscle visualization is excellent, and the wristed robotic instruments provide the dexterity needed for precise suture placement. A robotic instrument can be used to grasp Gore-Tex™ suture material so that knots can be tied without inadvertent slippage, which can shorten the neochords.
Triangular leaflet resection: a robotic triangular leaflet resection is shown. Generally, only the localized area of prolapse or ruptured chords needs to be resected. Often this is a small area as adjacent chords become displaced toward the ventricle with leaflet edge closure. The defect is closed using a two-layer polypropylene running suture. Again, the assistant uses a hook instrument to follow and facilitate tightening of the closure line
Sliding leaflet repair: in the presence of a large posterior leaflet prolapse, especially when there is other redundant tissue, a sliding leaflet plasty may be warranted. Here, the large prolapsing central segment is resected in quadrangular fashion. Thereafter, the remaining posterior leaflet segments (P1 and P3) are mobilized using a radial incision. During reattachment of the “P1 and P3 flaps” to the annulus leaflet, a running suture is used to advance them to meet in the annular center. Thereafter, the remaining vertical defect is closed with a running suture that is managed as described previously
Every repair should be tested by instilling cold saline into the ventricle via a catheter placed across the mitral valve. The catheter is introduced via the working port and is manipulated within the atrium by the console surgeon. Valve testing can be done either with a syringe or with a pressurized irrigator. After filling the ventricular with saline, we select the correct flexible annuloplasty band size. Because of our small working port (15-mm), it is difficult to pass standard inflexible annuloplasty band/ring sizers into the chest. Using the standard sizers as templates, we have fashioned flexible ring/band sizers from silastic sheet material. These sizers are introduced easily via the working port and can be manipulated using robotic instruments (Fig. 21.13).
Flexible annuloplasty band/ring sizers: flexible sizers have been made from thick silastic sheet material, using standard rigid ones as a template. Flexible sizers can be inserted easily through the small working port and thereafter, manipulated robotically toward the annular plane. This method provides the most accurate determination of the correct annuloplasty band or ring size
Over the years we have used several suture techniques to secure flexible annuloplasty bands and rings. The “interrupted” suture technique is time consuming because it requires a great deal of knot tying. Early in our experience, we secured annuloplasty bands with nitinol V-100 U-Clips™ (Medtronic Inc, Minneapolis, MN) and this method worked well. However, these clips are no longer manufactured. In early 2009 we changed to a running mattress suture technique, using braided suture (Fig. 21.14). With this method sutures are placed first at each fibrous trigone, passed through the annuloplasty band ends, and then tied. Thereafter, one suture is passed in a “running mattress” fashion—first through the mitral valve annulus—through the posterior band—back through the anterior band—and then through the valve annulus again, etc. The two running sutures are carried posteriorly, meeting at the mid-band, where they are tied. For rigid ring implantation we place interrupted sutures. After completion of the annuloplasty, the repair is saline tested again.
Annuloplasty band implantation—running suture technique. First, braided sutures are placed at each fibrous trigone and then passed through the annuloplasty band ends. After these trigone sutures are tied against the band, the needle is passed back through the band and then through the annulus in a horizontal mattress fashion. Thereafter, the needle is passed back through the band. From each end this sequence is replicated until sutures meet in the middle of the posterior band. Then, the sutures are tightened and tied by the assistant using an extracorporeal knot pusher
Atriotomy Closure and Air Removal
Once the valve repair is completed, the atriotomy is closed using two running 4-0 Gore-Tex™ sutures. A suture is placed at each end of the atriotomy with edges sewn toward the middle. As this suture line is being completed, the atrial sucker should be removed and if a pulmonary artery vent is present, suction discontinued. This provides passive left heart filling, which allows blood and entrapped air to escape through the untied atriotomy suture line. With the patient rotated leftward, the atriotomy becomes the highest point in the left heart. To complete cardiac de-airing, the perfusionist should fill the heart, while the anesthesiologist ventilates the left lung. Once the atriotomy sutures are tied, the aortic cross-clamp is removed and suction is placed on the aortic cardioplegia catheter to clear residual air. After the cardioplegia suture is tied, the atriotomy is inspected for hemostasis.
A19-Fr Blake drain is introduced through the atrial retractor port and directed into the posterior pericardium via the oblique sinus. Thereafter, the pericardium is closed loosely with two sutures. A second Blake drain is introduced into the pleural space via the right instrument port. After all instruments and trocars have been removed from the thorax, both lungs are ventilated, and the patient is weaned from cardiopulmonary bypass. After femoral artery repair, the right lung is deflated and the hand-held 3-D camera re-inserted to inspect all potential bleeding sites (atriotomy, aortic needle, trocar, pericardial suture). Bleeding usually can be controlled with an external electrocautery, and re-docking the robot rarely is needed. Before incision closure local anesthetic On-Q ™ infusion catheters (I-Flow Corp, Lake Forest, CA) are placed along the camera port, working port and clamp interspace sites.
Pearls and Pitfalls
-
Venous Cannulation: After the coronary sinus and pulmonary artery vent catheters have been placed in the superior vena cava and right atrium, it can be very difficult to identify the femoral vein guide-wire. Only the “J” end of the wire is clearly identifiable. When advancing the guide-wire through the atrium and into the SVC, it is essential to follow the “J” end to be sure that it has entered the SVC and is not curled in the atrium. Thereafter, we position the venous cannula sufficiently into the SVC to assure good venous return. It is much easier to withdraw the venous drainage cannula than to advance it after the guide-wire has been removed.
-
Avoiding diaphragm and liver injury: Some surgeons have experienced these complications in their early robotic mitral valve repair series. During right instrument port creation, the trocar can pierce the diaphragm, where it originates closely from the chest wall. This is especially true if the CO2 insufflation pressure has been released. We avoid this complication by placing the right instrument port under endoscopic visual guidance. This allows us to see the right instrument as it comes through the chest wall. The diaphragm and liver also can be injured a during right arm instrument exchange. During right instrument arm exchange, the diaphragm can move cephalad and lap over the cannula end. In this circumstance the diaphragm can be injured when the new instrument is inserted. We avoid this problem by using an extra-long trocar cannula for right instrument introduction. The tip is passed over the diaphragm, distracting it and allowing unimpeded instrument exchanges.
-
Running suture: The challenge of a using running suture line relates to coordination between the console and patient-side surgeon. The patient-side assistant uses a suture hook to tighten each loop, enabling constant maintenance of tension. This allows the console surgeon to keep the needle continuously in the robotic needle driver. If the suture is too short to allow this technique to be use comfortably, the assistant can retrieve the needle, hold the suture, and reintroduce the needle for robotic instrument sewing. This also will maintain constant tension on the suture line.
-
Cardioplegia catheter: If the aortic infusion catheter is displaced inadvertently during the operation, cardioplegia can be given via a retrograde cannula. In rare circumstances a longer antegrade cardioplegia cannula may be needed and can be introduced either through the chest wall or around the working port and then secured with an aortic suture.
-
Working Port: A soft 15-mm thoracoport has been adequate access to the pleural space and heart for most robotic cardiac procedures. If we are doing a concomitant cryo-maze procedure to ablate atrial fibrillation, we use a 20-mm thoracoport to have enough space to introduce both the cryo probe and irrigation catheter. Also, we use the larger port to insert rigid annuloplasty rings, as it is difficult to pass them through the smaller port. For mitral valve replacement, we use either a narrow rectangular 35 × 12-mm metal port (ATS Medical, Minneapolis, MN) or a small thoracotomy with a small silastic Alexis™ wound retractor (Applied Medical, Rancho Santa Margarita, CA).
-
Team Work: Robotic heart surgery is definitely a “team sport”. For the procedure to progress smoothly and safely there needs to be well-coordinated execution by the console surgeon, patient-side assistant, and the entire surgical team. This is especially true for specific maneuvers such as using running sutures, aortic clamping, and cardioplegia catheter insertion. It is critical that the console surgeon and patient-side assistant practice together and become a well-coordinated team. Our technique depends heavily on the assistant surgeon. There are technique modifications that to some degree can reduce the dependence upon the patient-side assistant. Either small nitinol U-clips or interrupted sutures can be used to sew leaflet tissue with robotic tying to minimize dependence on the assistant. Similarly, the annuloplasty band can be attached with short sutures again with robotic tying. With a careful planning and practicing all steps, the console surgeon and assistant can become a very efficient team, and complex robotic intra-cardiac surgery can be performed reproducibly and safely.
Outcomes
Between June 2003 and June 2011, we performed 410 robotic mitral valve repairs. During the same period, we have done an additional 53 mitral valve replacements for rheumatic disease. Of all patients 61.5 % were men with a mean age of 59 ± 13 years (20–86 years). Mitral repair techniques included leaflet resections (63 %), sliding leaflet reconstructions (20 %), Gore-Tex™ neo-chord replacements (18 %), and isolated annuloplasty ring implantations (17 %). Concomitant procedures included left atrial appendage closures (63 %), patent foramina ovale or ASD closures (26 %), and cryo-maze ablations for atrial fibrillation (17 %). In one patient a concomitant a robotic coronary artery bypass was performed.
There were two emergency conversions from a robotic to an open sternotomy procedure. One was in an 80-year old patient, who developed a retrograde aortic dissection upon institution of cardiopulmonary bypass, and the second was in a 77-year old patient who was explored for bleeding. The aortic dissection patient was the only operative mortality in the series. There was one conversion from repair to replacement (performed robotically) for post-repair moderate mitral regurgitation after ring placement for functional regurgitation.
For the series total cardiopulmonary bypass time averaged 143 ± 29 min with a mean cross clamp time of 99 ± 21 min. With experience both operative times have decreased, even in the presence of escalating pathology, complexity, and increased number of concomitant procedures. During the past 2 years our cardiopulmonary bypass and cross clamp times for lone mitral valve repairs have decreased to 121 ± 19 min and 84 ± 16 min, respectively. During the same interval, valve repairs with a concomitant cryo-maze procedure required times of 164 ± 44 min and 101 ± 21 min, respectively.
In this series post-operative trans-esophageal echo studies showed 0 to trace MR in 98 % of patients and no more than 1+ MR in any patient. Other series complications included perioperative strokes (1 %) and re-operations for bleeding (2 %) [0.5 % the last 2 years]. Our hospital length of stay was 4.0 ± 2.5 days for the entire group. Two patients required an early reoperation (one for endocarditis and the other for a delayed aortic dissection). Five patients required a late reoperation (two for endocarditis, one for a rigid ring dehiscence, one from ruptured Gore-Tex™ chord, and one for mitral stenosis (6 years after quadrangular resection).
References
Enriquez-Sarano M, Schaff HV, Orszulak TA, Tajik AJ, Bailey KR, Frye RL. Valve repair improves the outcome of surgery for mitral regurgitation: a long-term study. Circulation. 1995;91:1022–8.
Gillinov AM, Cosgrove DM, Blackstone EH, Diaz R, Arnold JH, Lytle BW, et al. Durability of mitral valve repair for degenerative disease. J Thorac Cardiovasc Surg. 1998;116:734–43.
Suri RM, Schaff HV, Dearani JA, Sundt III TM, Daly RC, Mullany CJ, et al. Survival advantage and improved durability of mitral valve repair for leaflet prolapse in the current era. Ann Thorac Surg. 2006;82:819–26.
Mohr FW, Falk V, Diegler A, Walther T, Gummert JF, Bucerius J, et al. Computer-enhanced “robotic” cardiac surgery: experience in 148 patients. J Thorac Cardiovasc Surg. 2001;121:842–53.
Nifong LW, Chu VF, Bailey M, Maziarz DM, Sorrell VL, Holbert D, et al. Robotic mitral valve repair: experience with the da Vinci system. Ann Thorac Surg. 2003;75:438–43.
Nifong LW, Chitwood WR, Pappas PS, Smith CR, Argenziano M, Starnes VA, et al. Robotic mitral surgery: a United States multicenter trial. J Thorac Cardiovasc Surg. 2005;129:1395–404.
Chitwood WR, Rodriguez E, Chu MW, Hassan A, Ferguson TB, Vos PW, et al. Robotic mitral valve repairs in 300 patients: a single-center experience. J Thorac Cardiovasc Surg. 2008;136:436–41.
Murphy DA, Smith JM, Siwek LG, Langord DA, Robinson JR, Reynolds BR, et al. Multicenter mitral valve study: a lateral approach using the da Vinci surgical system. Innovations. 2007;2:56–61.
Murphy DA, Miller JS, Langford DA, Snyder AB. Endoscopic robotic mitral valve surgery. J Thorac Cardiovasc Surg. 2006;132:776–81.
Smith JM, Stein H. Endoscopic placement of multiple artificial chordae with robotic assistance and nitinol clip fixation. J Thorac Cardiovasc Surg. 2008;135:610–4.
Nifong LW, Rodriguez E, Chitwood WR. 540 Consecutive robotic mitral valve repairs including concomitant atrial fibrillation cryoablation. Ann Thorac Surg. 2012;94:38–43.
Suri RM, Antiel RM, Burkhart HM, Huebner M, Li Z, Eton DT, et al. Quality of life after early mitral valve repair using conventional and robotic approaches. Ann Thorac Surg. 2012;93:761–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag London
About this chapter
Cite this chapter
Siwek, L.G., Reynolds, B.R. (2014). Robotic Endoscopic Mitral Valve Repair: Trans-thoracic Clamp Technique. In: Chitwood, Jr., W. (eds) Atlas of Robotic Cardiac Surgery. Springer, London. https://doi.org/10.1007/978-1-4471-6332-9_21
Download citation
DOI: https://doi.org/10.1007/978-1-4471-6332-9_21
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-6331-2
Online ISBN: 978-1-4471-6332-9
eBook Packages: MedicineMedicine (R0)