Abstract
This paper describes the use in routine diagnosis of virological kit, which was designed to identify the 15 most common respiratory viruses in clinical specimens of nasopharyngeal aspirates, swabs, and bronchoalveolar lavage. It is a one-step multiplex RT-PCR system for the detection of influenza virus type A and type B, human respiratory syncytial virus type A, B; human adenovirus, human metapneumovirus, human coronaviruses 229E/NL63 and OC43, human parainfluenza type 1, 2, 3, human rhinovirus type A, B, human enterovirus, and bocavirus 1, 2, 3, 4. The article presents research conducted on the basis of swabs collected from patients who came to the Ear, Nose, and Throat Emergency Care Unit at the Department of Otolaryngology, Military Medical Institute in Warsaw, in February 2013. Due to the nature of work in an laryngological emergency ward, the material was collected only from those patients who reported problems associated with rhinitis or any dysfunction of the upper respiratory tract. The study shows that patients who came to seek laryngological assistance were usually infected with viruses having affinity for the airway epithelium.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
The laboratory diagnostics of virological infections in the respiratory system is currently based primarily on modern methods of molecular biology. Serological methods, and in the case of influenza virus infection also a viral culture in chick embryo, constitute a smaller value for diagnostics, because of the time needed to obtain a result, although they are still considered to be the gold standard in virological studies of the respiratory system. The respiratory tract infection is divided into upper and lower respiratory tract infection. However, the upper respiratory tract infections constitute a preliminary stage to the infection of the bronchi and lung parenchyma. Chronic heart and lung diseases, diabetes, cancer, renal failure, hematopoietic system diseases, and other chronic diseases occur more frequently as complications in the case of patients with severe lower respiratory tract infections involving the respiratory viruses (Kim et al. 2013). In such a case, especially when the patient with severe symptoms of respiratory tract infection and associated immune disorders or the comorbidities comes to the laryngological ER, the virological laboratory diagnostics allowing for the identification of the etiological agent is extremely helpful.
1.1 Selected Pathogens Responsible for Respiratory Tract Infections
Respiratory tract infections are the most frequent cause of visits to the doctor. Pneumonia is still a threat to life and health, especially in children and elderly patients affected by comorbidities. The pathogens responsible for respiratory infections include viruses, bacteria, and in exceptional cases, fungi and parasites. Table 1 shows the most common viruses that are the cause of respiratory tract infections.
2 Methods
The material consisted of swabs from the nose and throat collected from patients during the ear, nose, and throat (ENT) emergency care in the period January–February 2013 in the Military Medical Institute in Warsaw, Poland (14 samples), and of the specimens which were accepted for tests for the detection of respiratory viruses by the Laboratory of Influenza Virus Research, National Center for Influenza in the National Institute of Public Health-National Institute of Hygiene in the season 2012/2013 (10 samples). The material was collected no later than 5 days after the onset of clinical symptoms according to the accepted criteria (WHO 2011).
2.1 Isolation of Viral RNA
The isolation of RNA is a template used in further polymerase chain reaction (PCR) studies to detect the presence of genetic material of viruses that cause respiratory tract infections. For this purpose QIAamp Viral RNA Mini Kit (Qiagen, Hilden, Germany) was used. The kit is designed to isolate RNA from clinical samples. A single elution with the use of elution buffer is sufficient to recover at least 90 % of the viral RNA from the QIAamp column.
2.2 Carrying Out a PCR Reaction
The RV15 One Step ACE Detection Kit (Seegene, Seoul, South Korea) is a qualitative in vitro test for the detection of 15 types of respiratory viruses in the aspirates from nasopharynx and nasopharyngeal swabs or samples from bronchopulmonary tree lavage in patients with clinical symptoms. The kit contains a set of reagents due to which it is possible to perform a Multiplex PCR. Simplification of the two-step method results in an increased repeatability of analysis and efficiency of reaction. The kit for determining 15 respiratory viruses in a sample of a clinical material is based on a process of reverse transcription (RT) and amplification of the target DNA by PCR using Dual Priming Oligonucleotide (DPO) primers, which provides freedom in a primer design and PCR optimisation and maximizes PCR specificity and sensitivity by fundamentally blocking non-specific priming. The DPO-based multiplex assay that permits the simultaneous amplification of target sequences of 15 viruses, presented after the amplification reaction, uses e.g., electrophoresis in an agarose gel preceded by nucleic acid isolation (Kim et al. 2013).
The kit consists of three panels/sets A, B, C, each containing reagents and primers for the detection of five respiratory viruses (details are given in Table 2) and includes two internal controls: PCR control and the control of the whole process. PCR controls were added to the A and B panel in order to identify the substances contained in the tested samples and to determine whether they might interfere with PCR amplification. Panel C has as an internal control a human RNase P, which allows the inspection of the whole process from the extraction of nucleic acids to RT-PCR. Additionally, 8-methoxypsoralen was used, which suppresses the activity of a DNA template. The 8-methoxypsoralen (8-MOP) reagent binds to the double-stranded structure of nucleic acids, forming covalent bonds between the strands upon activation by ultraviolet light.
2.3 Detection of PCR Products by Electrophoresis in Agarose Gel
When one-stage PCR was carried out in a thermocycler, the amplification products were placed onto a previously prepared 1.5 % agarose gel. The preparation of the gel consisted of dissolving the agarose in TAE (Tris-acetate-EDTA) buffer. After partial cooling, ethidium bromide was added at a concentration of 10 mg/ml. The gel was solidified using special well combs and mixtures, after amplification, were applied to the resulting holes in the agarose. The mixture also contained a loading dye. This procedure makes it possible to control the electrophoretic separation process using the kit for electrophoresis Wide Mini-SubCell GT/PowerPac Basic System (Bio-Rad Laboratories, Hercules, CA). Thus, the electrophoresis was carried out by controlling the migration of PCR products in a gel by placing a loading dye – bromphenol blue. To get the maximum separation of DNA fragments, the electric field did not exceed 5 V/cm of the gel. After the electrophoresis, the gel was analyzed under UV light in the GelDoc EQ system, and the resulting image was documented using Quantity One software (Bio-Rad Laboratories, Hercules, CA).
2.4 Eligibility Criteria of the Test
The presence of 15 respiratory viruses in the RNA samples tested was confirmed by the amplification products of the proper base pairs, as shown in Table 2.
3 Results and Discussion
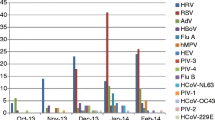
We found genetic material of eight different respiratory viruses including: Influenza Virus type A and B, Human enterovirus, Human parainfluenza virus, Human rhinovirus, Human coronavirus OC43, Human respiratory syncytial virus, and Human metapneumovirus. A co-infection of two or three types of respiratory viruses was often present. Of the 24 samples taken from patients, there were mixed infections with respiratory viruses in 15 cases (62.5 %); the most common co-infection combinations are presented in Table 3. Of the remaining nine samples, only viral genetic materials were identified of: influenza virus type A in 7 (29.1 %) cases, and Coronavirus OC43 in one and HEV virus in one case each. Figure 1 shows a breakdown of viruses.
Virological laboratory methods can be a valuable addition to medical clinical diagnostics conducted in patients with respiratory tract infections and avoid the use of unnecessary antibiotic therapy (Brydak et al. 2013). The commissioning of a microbiological examination must be supported by an appropriate medical decision on whether and how the result will be used. The selection of, or resignation from, the available laboratory testing method should be based on the analysis of the workload, cost, waiting time for the outcome, and the expected clinical benefits for patients (Wozniak-Kosek and Bydak 2013).
The knowledge of available laboratory techniques both virological and bacteriological, and their advantages and limitations is important for decision-making (Nitsch-Osuch et al. 2013). In cases requiring a rapid response on the part of the laboratory staff, the collaboration with a doctor is crucial to select appropriate tests and to interpret results. The difficulty in the treatment of infections caused by respiratory viruses is related to the lack of effective drugs. The only exception to this end is the treatment of influenza with the neuraminidase inhibitors oseltamivir and zanamivir which are highly effective (Demkow 2008; Van-Tam and Sellwood 2013).
References
Brydak LB (2008) Influenza, pandemic flu: myth or a real threat? Rhythm, Warsaw, pp 1–492 (in Polish)
Brydak LB, Wozniak-Kosek A, Nitsch-Osuch A (2013) Influenza diagnosis and vaccination in Poland. Respir Physiol Neurobiol 187:88–93
Demkow U (2008) The immunological and molecular diagnosis of respiratory tract infections. Med News 77:239–242 (in Polish)
Kim H-K, Oh S-H, Yun KA, Sung H, Kim M-N (2013) Comparison of anyplex II RV16 with the xTAG respiratory viral panel and Seeplex RV15 for detection of respiratory viruses. J Clin Res 4:1137–1141
Nitsch-Osuch A, Wozniak-Kosek A, Korzeniewski K, Zycinska K, Wardyn K, Brydak LB (2013) Accuracy of rapid influenza detection test in diagnosis of influenza A and B viruses in children less than 59 months old. Adv Exp Med Biol 788:71–76
Van-Tam J, Sellwood C (2013) Pandemic influenza, 2nd edn. CABI Publishing, Oxfordshire, United Kingdom, pp 1–234
WHO Global Influenza Surveillance Network (2011) Manual for the laboratory diagnosis and virological surveillance of influenza. WHO Press, Geneva, Switzerland, pp 1–139
Wozniak-Kosek A, Brydak LB (2013) Virological monitoring of influenza activity and influenza-like illness in the epidemic season 2011–2012 in Poland. Adv Exp Med Biol 788:77–82
Conflicts of Interest
The authors declare no conflicts of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Wozniak-Kosek, A., Kosek, J., Zielnik-Jurkiewicz, B. (2014). Detection of Respiratory Tract Pathogens with Molecular Biology Methods. In: Pokorski, M. (eds) Respiratory Infections. Advances in Experimental Medicine and Biology(), vol 835. Springer, Cham. https://doi.org/10.1007/5584_2014_30
Download citation
DOI: https://doi.org/10.1007/5584_2014_30
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-10014-2
Online ISBN: 978-3-319-10015-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)