Abstract
Hereditary hemorrhagic telangiectasia (HHT) is a hereditary disorder that causes refractory nasal bleeding, arteriovenous malformations in the lung (pulmonary arteriovenous fistula: PAVF), central nervous system (CNS-AVF), and liver (hepatic AVF). HHT is caused by genetic abnormalities in endoglin (ENG), ACVRL1 (ALK1), and other rare genes (e.g., SMAD4). The relationship between these gene mutations and the affected organs remains unclear.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
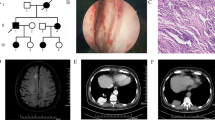
Hereditary hemorrhagic telangiectasia (HHT) is a hereditary disorder that causes refractory nasal bleeding, arteriovenous malformations in the lung (pulmonary arteriovenous fistula: PAVF), central nervous system (CNS-AVF), and liver (hepatic AVF). HHT is caused by genetic abnormalities in endoglin (ENG), ACVRL1 (ALK1), and other rare genes (e.g., SMAD4). The relationship between these gene mutations and the affected organs remains unclear.
We performed genetic analysis from whole blood of 464 suspected HHT patients or HHT carriers from April 2005 to November 2015 in 35 hospitals and found 264 patients positive for mutation in ENG, ALK1, and SMAD4 genes. Of these 264 positive results, we excluded 68 patients who were sporadic, non-familial cases and performed proband gene analysis. We also excluded 107 non-symptomatic mutation carriers and leaving a total of 89 patients with AVFs.
To clarify the relationship between gene mutations and the affected organs, we assessed the mutations and clinical presentation of these 89 patients. We found 25 mutations in the ENG gene from 68 patients and 8 mutations in the ALK1 gene from 21 patients. We then grouped patient AVF presentation (PAVF, CNS-AVF and hepatic AVF) according to the genetic mutation (Table 26.1).
Among patients with mutations in ENG, 19/25 (79%) mutations and 46/68 (69%) of patients presented with the same affected organ pattern. PAVFs were tending to be the same. Hepatic AVFs were rarely described in patient profiles so we were unable to evaluate hepatic AVF presentation patterns in mutated ENG patients.
In patients with mutations in ALK1, 8/10 (80%) mutations, 16/21 (76%) patients presented with the same affected organ pattern. For example, all five patients with the Arg479X mutation presented with the same affected organ pattern.
Previous reports have suggested that patients with mutations in ENG frequently have PAVFs. In contrast, patients with mutations in ALK1 frequently have hepatic AVFs and gastrointestinal telangiectasias but rarely have CNS-AVFs [1,2,3]. However, previous reports have not discussed similarity and combination of AVF patterns for each mutation.
In our analysis, approximately 70–80% of HHT patients with a previously detected genetic mutation presented with the same AVF pattern. Our result emphasizes the importance of genetic testing in HHT even if the patient had already been diagnosed according to other clinical findings.
References
Letteboer TG, Mager JJ, Snider RJ, et al. Genotype-phenotype relationship in hereditary haemorrhagic telangiectasia. J Med Genet. 2006;43(4):371–3.
Arthur H, Geisthoff U, Gossage JR, et al. Executive summary of the 11th HHT international scientific conference. Angiogenesis. 2015;18:511–24.
Komiyama M, Ishiguro T, Yamada O, et al. Hereditary hemorrhagic telangiectasia in Japanese patients. J Hum Genet. 2013;59:37–41.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2020 The Author(s)
About this paper
Cite this paper
Iwasa, T., Yamada, O., Morisaki, H., Morisaki, T., Kurosaki, Ki., Shiraishi, I. (2020). Relationship Between Mutations in ENG and ALK1 Genes and the Affected Organs in Hereditary Hemorrhagic Telangiectasia. In: Nakanishi, T., Baldwin, H., Fineman, J., Yamagishi, H. (eds) Molecular Mechanism of Congenital Heart Disease and Pulmonary Hypertension. Springer, Singapore. https://doi.org/10.1007/978-981-15-1185-1_26
Download citation
DOI: https://doi.org/10.1007/978-981-15-1185-1_26
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-1184-4
Online ISBN: 978-981-15-1185-1
eBook Packages: MedicineMedicine (R0)