Abstract
This chapter describes three methods for assessing the impact of transfusion-transmitted infections on public health. In order of increasing precision and labor intensity, these tools are:
-
1.
A blueprint for a structured, qualitative inventory and report, describing the relevant characteristics of the emerging agent, which helps to make ad hoc decisions and which identifies gaps in our knowledge.
-
2.
Two more sophisticated “off the shelf” methods for the quantitative analysis of threats to blood safety are mentioned: the Biggerstaff-Petersen model and the European Up-Front Risk Assessment Tool (EUFRAT). The Biggerstaff-Petersen model estimates the number of potentially infectious donations, while EUFRAT also takes into account the components prepared from donations and the efficacy of various mitigating interventions.
-
3.
Finally examples of quantitative studies of specific agents are mentioned: a donor-recipient transmission study and a cost-benefit modeling study. For this kind of analysis, no standardized recipe is available.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Blood transfusion
- Emerging infection
- Transfusion transmitted infection
- TTI
- Risk assessment
- Outbreak
- Safety measure
- Intervention
- Donor screening
Introduction
A threat to the safety of blood components and blood products may arise because a new outbreak occurs. Recent examples are outbreaks caused by arboviruses (dengue, West Nile fever, chikungunya, and Zika), coronaviruses (MERS and SARS), and zoonotic outbreaks caused by the BSE/variant Creutzfeldt-Jakob disease (vCJD) agent from cattle, by the Coxiella burnetii bacterium from goats, and by hepatitis E virus genotype 3 (HEV-3) from pigs. Theoretically, threats may come from agents that always have been around; a “new” threat may arise because we realize that an “old” agent is less innocent for certain recipients than assumed.
Other chapters describe the prediction and monitoring of threats. In this chapter, it is described how the consequences for public health of a transfusion-transmitted agent can be estimated. A checklist is provided for a structured inventory of the relevant properties of an emerging transfusion-transmitted agent. Once completed, this inventory gives an indication of the transfusion-associated morbidity and mortality that can be expected and of mitigating interventions that can be considered. The inventory is based on the approach as designed by the author in 1998 for the Dutch blood transfusion service. It has been found to be useful in real-life blood banking, but it has not been validated or acknowledged officially; other approaches may be as good or better. Subsequently two models are described for a more quantitative analysis of the impact of a transfusion-transmitted infection; both models are available in the public domain. Finally, some examples are given of advanced, agent-specific studies which were performed to assess the impact of an emerging blood-borne threat. In a wider context the Alliance of Blood Operators developed the Risk-Based Decision Making framework for risk mitigation in blood safety, as yet it is beyond the scope of this chapter.
Assessing the Threat: A Structured Approach
The emergence of a (potential) blood-transmitted agent necessitates the evaluation of the threat it poses to the safety of blood components and blood products. This assessment serves several goals: (1) possibly short-term measures must be taken to limit blood-borne spread of the agent; (2) relevant gaps in our knowledge of the agent must be identified and addressed; (3) health authorities and the general public must be provided with relevant information regarding the safety of the blood supply; (4) parameters must be provided to modelers enabling cost-benefit analysis of potential interventions; and (5) a long-term safety policy must be defined. Assessing the threat of a transfusion-transmitted pathogen includes two steps:
Step 1: Collect Facts and Uncertainties
The properties of the agent that are relevant for blood banking must be collected. To complete this inventory, the checklist as presented in Table 2.1 of this chapter can be used. The inventory may seem to contain some redundancies, but it must be realized that, for example, the detection of a viral genome by PCR in blood components does not equate with infectivity. Concurrent antibodies may neutralize the agent, or only noninfectious RNA or DNA remnants of the agent may be present. Proven transmission of the agent by blood components does not equate with disease in the recipient. For example, so far, disease caused by transfusion-transmitted dengue, chikungunya, or Zika virus infection seems an exception.
Using the data as obtained in step 1, additional calculations and modeling may be performed to provide detailed figures for the expected morbidity and mortality and for the efficacy of interventions. The costs and benefits of preventive interventions, such as the introduction of donor deferral and donor screening, must be estimated. Unfortunately, detailed numerical analysis may take considerable time. Often safety measures must be considered in absence of a detailed cost-benefit analysis. The exact methodology for modeling and cost-benefit analysis is beyond the scope of this chapter but is partly covered by a following paragraph of this chapter.
Step 2: Report and Conclude
The inventory of Step 1 must be reported and summarized in a format that is understandable for blood bank directors, physicians, safety boards, and government officials. A practical format for the report is provided in Table 2.2. The report not only must present the relevant properties of the agent in a readable way, the data as obtained in step 1 must be interpreted, and three conclusions must be presented:
-
1.
An estimate must be provided of the expected morbidity and mortality, caused by the emerging agent via blood transfusion and blood products. Often, in the absence of hard data, only a carefully phrased educated guess is possible.
-
2.
Safety measures must be described that (may) reduce the expected transmission via blood components and blood products.
-
3.
Gaps in the knowledge of the agent must be identified that must be addressed.
Quantitative Analysis of the Impact of a Transfusion-Transmitted Infection and of Countermeasures
Tools for Quantitative Assessment of Transfusion-Transmitted Infections
The previous paragraph offers an approach to quickly obtain a thorough, but qualitative assessment of the threat to blood safety, caused by an emerging agent. Based on this approach, some excerpts from previous real-life situations and reports are:
-
“Given the efficacy of our inactivation procedures for enveloped viruses, it is unlikely that our plasma products transmit GB-virus-C.”
-
“Last spring, up to 1 in 5000 donors was silently highly viremic for parvovirus-B19.” (It was found that approximately every 4 years, parvovirus-B19 infections show a considerable seasonal peak, with many donors being silently infected).
-
“In the years following the outbreak of Q-fever, 1 in 100 infected persons may silently harbor chronic Coxiella infection, which amounts to 1 in 1000 blood donors in the affected area.” (According to literature, roughly one in one hundred persons who acquire Coxiella burnetii infection will develop chronic infection, while in a specific affected area, one in ten citizens became infected via air-borne transmission).
-
“Zika virus especially is a threat for pregnant women. An estimated 0.1% of our RBC transfusions concern pregnant women.” (Gynecologists and transfusion specialists were asked about the number of transfusions among pregnant women; and detailed transfusion data were available from a comparable country).
Such remarks are useful because they highlight the problem, but they provide insufficient quantitative information about the impact of the threat on public health. To facilitate a more quantitative analysis of the consequences of an emerging infection for the safety of blood components and blood products, two models are available in the public domain. The models are compared in a review by Kiely et al. [1]. In response to the West Nile virus outbreak in the USA, Biggerstaff and Petersen (CDC, Fort Collins, USA) designed a model for the estimation of the number of silently viremic blood donors, based on a combination of deterministic calculations and a Monte Carlo simulation [2, 3]. Others used the Biggerstaff-Petersen model to assess chikungunya outbreaks in La Reunion [4], Thailand [5], and Italy [6], a dengue outbreak in Australia [7], a Ross River virus outbreak in Australia [8], and a hepatitis A outbreak in Latvia [9].
Van der Poel (Sanquin Blood Supply Foundation, Amsterdam), Janssen (Transfusion Technology Assessment, University of Utrecht), and Domanovic (ECDC, Stockholm) initiated the computer-based, interactive “European Up-Front Risk Assessment Tool” (EUFRAT), for the quantitative estimation of transfusion transmission risks as posed by emerging infections [10]. The tool is freely accessible via http://eufrattool.ecdc.europa.eu. EUFRAT supports local outbreaks, and threats that are introduced by traveling donors, returning from affected areas abroad. After data have been entered, EUFRAT calculates the number of infected and diseased recipients. Entering the data includes five steps:
-
In step 1 predefined parameters for 18 infectious agents can be selected, or a new, still undefined agent can be chosen. Subsequently it must be indicated whether donors are involved who visited an outbreak-affected region, whether data on infected donors are available, whether the infection has a chronic phase, and whether donor deferral or donor screening is available.
-
Dependent on the choices entered in step 1, in steps 2 to 5, specific parameters must be entered concerning “disease and outbreak,” “donor screening and donation testing,” “blood component production and donor exposure,” and “recipient population.”
EUFRAT has been used to assess the impact of chikungunya in Italy [11], Q-fever in the Netherlands [11, 12], Ross River fever in Australia [8], and dengue in donors returning from affected areas [13].
Advanced Quantitative Assessment
As a rule, in the early phase of an emerging infection, insufficient data are available to determine precisely the impact of the threat and the costs and benefits of mitigating interventions such as the deferral of at-risk donors and the introduction of molecular or serological screening of donors. Sometimes the true costs and benefits of a safety measure only become clear years after its introduction. For example, universal leukodepletion of blood donations was hoped to reduce the risk of transmission of the vCJD agent. The filters involved were expensive. The efficacy of prion protein removal by leukodepletion is based on indirect evidence, obtained using laboratory animals which only partially reflect human blood donors incubating vCJD. Years later, leukodepletion filters have become very cheap; they virtually remove the risk of CMV, EBV, and HTLV transmission; they reduce transfusion reactions and alloimmunization; and it still is expected that they reduce the risk of vCJD transmission. All in all, leukodepletion turned out to be very effective but in unexpected ways. On the other side of the spectrum is the donor screening for HIV RNA in countries with a low incidence of HIV infection. Introduction of universal HIV RNA donor screening was considered to be indispensable for the societal trust in blood transfusion. However, in countries with a low incidence of HIV infection, “HIV NAT only” donations may not be encountered. Based on carefully collected data and using advanced modeling, Borkent and colleagues calculated that triplex-NAT donor screening for HIV, HCV, and HBV, on pools of six donations, costs Euro 5,200,000 per quality-adjusted life year (QALY) gained in the Netherlands [14]. For this exercise, detailed characteristics of blood transfusion, recipients, and local HBV, HCV, and HIV epidemiology were taken into account.
A more recent example of advanced modeling, performed to estimate the consequences of an emerging infection for public health, concerns the analysis of transfusion-transmitted HEV genotype 3 infection:
-
Of all HEV infections nationwide one in 700 is estimated to be due to blood transfusion, while for chronic HEV infections this is one in 3.5. HEV screening of Dutch whole blood donations in pools of 24 would prevent 4.52 of the 4.94 transfusion associated chronic HEV infections expected annually, at approximately Euro 310,000 per prevented chronic case [15].
These seemingly simple findings could not be generated using the Biggerstaff-Petersen model or the EUFRAT tool; they were obtained by dedicated modeling, after several studies generated essential data:
-
During 2013–2016 the monthly screening of 2000 plasma donations for HEV RNA provided detailed data on the incidence of HEV infection, the duration of viremia, and the distribution of viremia levels.
-
A British study provided data on the infectivity of HEV via transfusion [16].
-
In academic hospitals the course of HEV infection in vulnerable subsets of patients was elucidated.
It became clear that especially solid organ- and stem cell transplant patients are at risk for developing chronic hepatitis E, sometimes with rapid onset of cirrhosis.
-
For these groups of patients, the exposure to blood components and other sources of HEV was determined.
-
The effect of timely diagnosis of hepatitis E and subsequent antiviral treatment was studied.
-
The costs and the yield of donor screening for HEV RNA using different pool sizes were calculated.
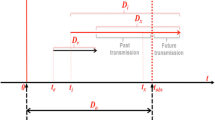
These examples of quantitative analysis point to a sobering conclusion. Reliable and detailed quantitative analysis of the impact of a transfusion-transmitted infection, including the costs and yield of mitigating measures, needs a team of specialists and considerable time. Figure 2.1 illustrates the complexity of only one aspect of this matter. Considering the impact of a transfusion-transmitted infection in terms of lost years of life and chronic sequelae, the a priori life expectancy of the exposed recipients varies considerably [17]. Figure 2.1 shows that platelets often are transfused to persons with (potential) long life expectancy, including young adults, children, and neonates at the far left of the graph, while Fig. 2.1 shows that the majority of fresh frozen plasma units was administered to patients with short life expectancies. Considering an emerging transfusion-transmitted threat, it appears that especially the administration of infectious platelets may have considerable consequences.
Characteristics of recipients of red blood cells, platelets, and fresh frozen plasma. (Reproduced with permission from John Wiley and Sons, from Borkent-Raven et al. [17])
An Unresolved Issue: Presence of DNA or RNA of a Pathogen Does Not Equate with Infectivity
No matter how detailed the knowledge of the course of viremia and the occurrence of antibodies for an emerging agent in donors with asymptomatic infection, the infectivity of blood donors in different phases of infection cannot be fully predicted. Only targeted studies provide clarity, as illustrated by the following three examples.
The donor-recipient HEV transmission study by Hewitt and colleagues showed that only 18 of 43 recipients (42%) of a blood component from an HEV-viremic donor acquired infection [16]. Absence of HEV antibodies and a high viral load in the donor made transmission more likely. The results of this study helped to estimate the minimum infectious dose of HEV and the infectivity of units of red blood cells, platelets, and plasma, given the levels of viremia in donors [15].
Remarkable details have been reported about the complex relation between infectivity of donated material and the detection of West Nile virus RNA in blood and organ donors [18]. In 54 blood donors, WNV RNA no longer was detectable in plasma 3 weeks after the donation that tested positive for WNV RNA. However, in 42% of the donors, WNV RNA remained detectable in whole blood up to 3 months after the index donation. In this phase, WNV is bound to erythrocytes, but – except for one case – blood components of the donors involved are not infectious for the recipients, probably due to the presence of neutralizing antibodies [18]. In contrast, organs from two donors in the later phase of infection (both testing positive for WNV IgG antibodies; one testing positive for WNV RNA in serum, one negative) caused WNV infection in their recipients [19].
Blood donors may silently harbor acute parvovirus B19 (B19V) infection. After acute infection, decreasing levels of parvovirus DNA are detectable during months to years. Once the parvovirus DNA level drops below 100,000 IU/mL (ref. 20) or 10,000 IU/mL [21], donors do not transmit B19V to their recipients, which is attributed to concurrent neutralizing antibodies or to a noninfectious amount of transfused virions. However, recently, an alternative explanation was reported [22]. Studying ten donors up to 22 months after acute asymptomatic B19V infection, viral DNA remained detectable for more than 1 year. After 150 days post-infection, the B19V DNA o f the donors became degradable by endonucleases, indicating that this concerned naked DNA, not the protected, encapsidated DNA as present in intact B19V virions. Hence, potentially infectious B19V viremia is only present during the first months of a much longer episode of B19V “DNA-emia” as detected by PCR.
Lasting Impact of vCJD
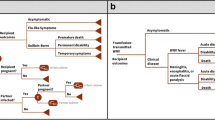
Considering the assessment of blood-borne threats to public health, possibly the most difficult task is to estimate the remaining threat of variant Creutzfeldt-Jakob disease (vCJD) , as posed by blood donors with possible subclinical vCJD infection. As reviewed by Seed and colleagues, several studies indicate that the classic, sporadic form of CJD is no threat to the safety of transfusion, but three fatal cases of vCJD and one subclinical infection have been attributed to transmission via blood transfusion [23]. Since the outbreak of mad cow disease (BSE) in Great Britain, with subsequent cases of vCJD in humans, many blood banks maintain safety measures to prevent transmission of vCJD via blood transfusion and blood products. Examples of safety measures are the exclusion of blood donors who stayed at least 6 months in the UK during 1980–1996 and the exclusion of donors who themselves were transfused. Is it time to lift these restrictions? Until recently it seemed that the outbreak of vCJD had ended. Unfortunately in 2016 a new vCJD patient was reported. This patient was found to be heterozygous (methionine/valine) for codon 129 of the human prion gene. This is alarming, because so far all vCJD patients were methionine homozygous (Fig. 2.2, lower panel). Possibly this first heterozygous patient reflects the start of a second wave of vCJD cases, with longer incubation times than the former homozygous cases. Apparently, people may harbor the infection during many years and, regarding blood banking, could be seen as asymptomatic but possibly infectious carriers. Studies of archived appendices suggest that indeed roughly 1 in 2500 British appendices tests positive for the vCJD agent. The first and second appendix studies involved 12,674 resp. 32,441 appendices, from persons born between 1961 and 1985 resp. 1941–1985 [24, 25]; see the two middle panels in Fig. 2.2. These persons experienced dietary exposure to the vCJD agent around 1990; and their appendices were removed in 1995–1999 resp. 2000–2012; in which 3 resp. 16 vCJD-prion-positive appendices were found. Is this finding really linked to dietary exposure to the vCJD agent in the 1980s and 1990s, or is there an unrelated, harmless, and natural background presence of the protein in appendices? The Appendix-III study included appendices and persons who did not live in the late 1980s and early 1990s [26]. The upper panel in Fig. 2.2 shows the confusing findings of the Appendix-III study: is the period of dietary exposure larger than assumed? Or is there no connection to the BSE/vCJD outbreak? Currently it seems wise not to abandon vCJD blood safety measures yet.
Summary and Conclusion
When a threat to the safety of blood occurs, one must find a balance between the time it takes to collect and report relevant information and the urgency to start mitigating interventions. This chapter described three methods for assessing the impact of transfusion-transmitted infections for public health, in order of increasing precision and increasing labor intensity:
-
1.
A blueprint for a qualitative inventory and a report, describing the relevant characteristics of the emerging agent, is offered in tables 2.1 and 2.2.
-
2.
Two more sophisticated, “off the shelf” methods for the quantitative analysis of a threat to blood safety, the Biggerstaff-Petersen model and the European Up-Front Risk Assessment Tool (EUFRAT), are described. The output of the Biggerstaff-Petersen model is the number of potentially infectious donations, while EUFRAT additionally takes into account the components prepared from donations and the efficacy of mitigating interventions such as donor screening and pathogen inactivation, enabling an estimation of the consequences for recipients.
-
3.
Examples of sophisticated quantitative studies of specific agents are mentioned: a donor-recipient transmission study [16] and a cost-benefit modeling study [15]. For this kind of analysis, no standardized recipe is available; the studies involved are defined by specific properties of the emerging agent and the local situation.
In an urgent situation, steps 1 and 2 will be started more or less simultaneously, and results may become available soon after. Sometimes an additional detailed cost-benefit analysis is needed. Only the implementation of partial or universal donor screening may generate sufficient data to precisely calculate the impact of the agent, facilitating the decision whether donor screening indeed is useful (in hindsight). In real-life blood banking, once safety measures have been implemented, it often is hard to stop them, even when the cost-benefit ratio is found to be very poor. Therefore, when a new threat arises, it must be considered to start donor screening only for a limited period [27]. This serves two purposes: it helps to prevent transmissions in an uncertain situation and maintains the public trust in blood transfusion, and it generates valuable data. When the period of temporary donor screening has ended, it can only be extended by an active decision to do so, based on the analysis of data that have become available in the meantime. This approach prevents the accumulation of inefficient preventive blood safety measures over time.
The impact of an emerging transfusion-transmitted infection on public health is only one of several factors that shape the policy regarding blood safety. In case of zoonoses (vCJD, Q-fever, and HEV genotype 3), agro-economic interests sometimes hindered effective safety measures. For other emerging agents, the emotional impact of the infection (e.g., of Zika-induced microcephaly), the societal trust in blood banking, and political liability (e.g., after local HIV or HCV “scandals”) may be more important for the introduction of blood safety measures than exact figures for transfusion-induced morbidity and mortality.
References
Kiely P, Gambhir M, Cheng AC, McQuilten ZK, Seed CR, Wood EM. Emerging infectious diseases and blood safety: modelling the transfusion-transmission risk. Transfus Med Rev. 2017;31(3):154–64.
Biggerstaff BJ, Petersen LR. Estimated risk of West Nile virus transmission through blood transfusion during an epidemic in Queens, New York City. Transfusion. 2002;42(8):1019–26.
Biggerstaff BJ, Petersen LR. Estimated risk of transmission of the West Nile virus through blood transfusion in the US, 2002. Transfusion. 2003;43(8):1007–17.
Brouard C, Bernillon P, Quatresous I, Pillonel J, Assal A, De Valk H, et al. Estimated risk of chikungunya viremic blood donation during an epidemic on Reunion Island in the Indian Ocean, 2005 to 2007. Transfusion. 2008;48:1333–41.
Appassakij H, Promwong C, Rujirojindakul P, Wutthanarungsan R, Silpapojakul K. The risk of blood transfusion-associated chikungunya fever during the 2009 epidemic in Songkhla Province. Thailand Transfusion. 2014;54:1945–52.
Liumbruno GM, Calteri D, Petropulacos K, Mattivi A, Po C, Macini P, et al. The chikungunya epidemic in Italy and its repercussion on the blood system. Blood Transfus. 2008;6:199–210.
Faddy HM, Seed CR, Fryk JJ, Hyland CA, Ritchie SA, Taylor CT, et al. Implications of dengue outbreaks for blood supply, Australia. Emerg Infect Dis. 2013;19:787–9.
Seed CR, Hoad VC, Faddy HM, Kiely P, Keller AJ, Pink J. Re-evaluating the residual risk of transfusion-transmitted Ross River virus infection. Vox Sang. 2016;110(4):317–23.
Perevoscikovs J, Lenglet A, Lucenko I, Steinerte A, Payne Hallstrom L, Coulombier D. Assessing the risk of a community outbreak of hepatitis A on blood safety in Latvia, 2008. Euro Surveill. 2010;15:19640.
Oei W, Janssen MP, van der Poel CL, van Steenbergen JE, Rehmet S, Kretzschmar ME. Modeling the transmission risk of emerging infectious diseases through blood transfusion. Transfusion. 2013;53(7):1421–8.
Mapako T, Oei W, van Hulst M, Kretzschmar ME, Janssen MP. Modelling the risk of transfusion transmission from travelling donors. BMC Infect Dis. 2016;16:143.
Oei W, Kretzschmar ME, Zaaijer HL, Coutinho R, van der Poel CL, Janssen MP. Estimating the transfusion transmission risk of Q fever. Transfusion. 2014;54:1705–11.
Oei W, Lieshout-Krikke RW, Kretzschmar ME, Zaaijer HL, Coutinho RA, Eersel M, Jubithana B, Halabi Y, Gerstenbluth I, Maduro E, Tromp M, Janssen MP. Estimating the risk of dengue transmission from Dutch blood donors travelling to Suriname and the Dutch Caribbean. Vox Sang. 2016;110(4):301–9.
Borkent-Raven BA, Janssen MP, van der Poel CL, Bonsel GJ, van Hout BA. Cost-effectiveness of additional blood screening tests in the Netherlands. Transfusion. 2012;52(3):478–88.
de Vos AS, Janssen MP, Zaaijer HL, Hogema BM. Cost-effectiveness of the screening of blood donations for hepatitis E virus in the Netherlands. Transfusion. 2017;57(2):258–66.
Hewitt PE, Ijaz S, Brailsford SR, Brett R, Dicks S, Haywood B, et al. Hepatitis E virus in blood components: a prevalence and transmission study in Southeast England. Lancet. 2014;15;384(9956):1766–73.
Borkent-Raven BA, Janssen MP, van der Poel CL, Schaasberg WP, Bonsel GJ, van Hout BA. The PROTON study: profiles of blood product transfusion recipients in the Netherlands. Vox Sang. 2010;99(1):54–64.
Lanteri MC, Lee TH, Wen L, Kaidarova Z, Bravo MD, Kiely NE, et al. West Nile virus nucleic acid persistence in whole blood months after clearance in plasma: implication for transfusion and transplantation safety. Transfusion. 2014;54(12):3232–41.
Nett RJ, Kuehnert MJ, Ison MG, Orlowski JP, Fischer M, Staples JE. Current practices and evaluation of screening solid organ donors for West Nile virus. Transpl Infect Dis. 2012;14:268–77.
Hourfar MK, Mayr-Wohlfart U, Themann A, Sireis W, Seifried E, Schrezenmeier H, Schmidt M. Recipients potentially infected with parvovirus B19 by red blood cell products. Transfusion. 2011;51(1):129–36.
Juhl D, Özdemir M, Dreier J, Görg S, Hennig H. Look-back study on recipients of parvovirus B19 (B19V) DNA-positive blood components. Vox Sang. 2015;109(4):305–11.
Molenaar-de Backer MW, Russcher A, Kroes AC, Koppelman MH, Lanfermeijer M, Zaaijer HL. Detection of parvovirus B19 DNA in blood: viruses or DNA remnants? J Clin Virol. 2016;84:19–23.
Seed CR, Hewitt PE, Dodd RY, Houston F, Cervenakova L. Creutzfeldt-Jakob disease and blood transfusion safety. Vox Sang. 2018;113:220. https://doi.org/10.1111/vox.12631. (Epub ahead of print).
Hilton DA, Ghani AC, Conyers L, Edwards P, McCardle L, Ritchie D, Penney M, Hegazy D, Ironside JW. Prevalence of lymphoreticular prion protein accumulation in UK tissue samples. J Pathol. 2004;203(3):733–9.
Gill ON, Spencer Y, Richard-Loendt A, Kelly C, Dabaghian R, Boyes L, Linehan J, Simmons M, Webb P, Bellerby P, Andrews N, Hilton DA, Ironside JW, Beck J, Poulter M, Mead S, Brandner S. Prevalent abnormal prion protein in human appendixes after bovine spongiform encephalopathy epizootic: large scale survey. BMJ. 2013;347:f5675.
Summary results of the third national survey of abnormal prion prevalence in archived appendix specimens. Public Health England Infection report (weekly). 2016;10(26).
Kramer K, Verweij MF, Zaaijer HL. Are there ethical differences between stopping and not starting blood safety measures? Vox Sang. 2017;112(5):417–24.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Zaaijer, H.L. (2019). Assessing the Threat: Public Health. In: Shan, H., Dodd, R. (eds) Blood Safety . Springer, Cham. https://doi.org/10.1007/978-3-319-94436-4_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-94436-4_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-94435-7
Online ISBN: 978-3-319-94436-4
eBook Packages: MedicineMedicine (R0)