Abstract
The management of ST-elevation myocardial infarction (STEMI) has evolved significantly with the introduction of new pharmacological therapies as well as interventional procedures and devices. The GISSI and ISIS-2 studies showed a mortality benefit of streptokinase over standard therapy (heparin ± oral anticoagulation)/placebo which lead to the widespread use of streptokinase in the late 1980s [1, 2]. The use of recombinant tissue plasminogen activator (rt-PA) was shown to be more beneficial than streptokinase in the TIMI and GUSTO trials [3, 4]. Results of other studies such as CLARITY and COMMIT paved the way for addition of clopidogrel to the drug regime which further reduced mortality [5, 6].
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
12.1 Introduction
The management of ST-elevation myocardial infarction (STEMI) has evolved significantly with the introduction of new pharmacological therapies as well as interventional procedures and devices. The GISSI and ISIS-2 studies showed a mortality benefit of streptokinase over standard therapy (heparin ± oral anticoagulation)/placebo which lead to the widespread use of streptokinase in the late 1980s [1, 2]. The use of recombinant tissue plasminogen activator (rt-PA) was shown to be more beneficial than streptokinase in the TIMI and GUSTO trials [3, 4]. Results of other studies such as CLARITY and COMMIT paved the way for addition of clopidogrel to the drug regime which further reduced mortality [5, 6].
Primary percutaneous coronary intervention (PPCI) became the preferred choice of treatment for acute STEMI, with balloon angioplasty (BA) showing an improvement in mortality (or the combined endpoint of mortality and MI) over thrombolysis in a number of studies [7, 8]. Subsequently, bare-metal stent (BMS) implantation in STEMI showed a reduction in target vessel revascularizations (TVR) in comparison with BA but without a reduction in death or MI in the Stent PAMI and CADILLAC trials [9, 10]. The percentage of vessels with TIMI III flow was numerically higher in the BA group as compared to the BMS group, while mortality and MI rates were numerically but not statistically lower [9]. When stenting (BMS) was compared with thrombolysis as in the STAT study, the results were similar with stenting showing a reduction in TVR but no reduction in death or MI [11]. When both first- and second-generation drug-eluting stents (DES) were compared to BMS in the setting of an acute STEMI, target vessel/lesion revascularization rates were shown to be lower with DES, but yet again no reduction in death or MI was shown [12,13,14,15]. Brodie et al. in a single-center study of 2195 patients over a follow-up period of 16 years showed long-term target vessel MI, and stent or lesion thrombosis was significantly higher with both BMS and DES as compared to BA (after landmark analysis at 1 year) [16]. Thus, although stent implant is often considered as definitive treatment for PPCI by securing the vessel lumen, this may not always provide optimal longer-term outcomes.
12.2 Drug-coated Balloons
There has been great interest recently in the concept of angioplasty with minimal or no permanent implant, by way of using either absorbable polymer DES or scaffolds. Drug-coated balloon-only (DCB-only) PCI has emerged as an alternative therapeutic option to treat coronary artery disease (CAD) and has the additional benefit of implanting no material with the exception of the necessary anti-restenotic drug. DCBs are semi-compliant balloons with a chemotherapeutic drug (commonly paclitaxel) incorporated with an excipient to facilitate the drug transfer upon inflation of the balloon. Paclitaxel is the drug of choice in most commonly available DCBs because of its highly lipophilic properties allowing rapid delivery into the vessel wall and sustained antiproliferative effect despite its short contact time with the vessel wall [17].
The SeQuent Please (B Braun, Melsungen AG, Germany), Pantera Lux (Biotronik, Berlin, Germany), and In.Pact Falcon (Medtronic, CA, USA) have the most published data supporting their efficacy and safety. The best long-term results of DCB are achieved with a DCB-only approach as compared to DCB plus BMS. DCB-only PCI is associated with a lower late lumen loss and lower target vessel revascularization.
12.3 Evidence for DCB Angioplasty in PPCI
Several studies have reported their experience of using DCB without stenting in the PPCI setting. Vos et al. carried out a pilot study involving 100 patients presenting with acute STEMI using the paclitaxel-coated Pantera Lux™. Cardiogenic shock and intubated out of hospital arrests were excluded. 59% had DCB-only PCI, with the rest requiring BMS implantation due to dissections of type C or greater (National Heart, Lung, and Blood Institute (NHLBI) classification). A 12-month follow-up revealed cardiac death in 2%, MI 0%, and target lesion revascularization rate of 3% in this selected group. TIMI III flow was achieved in 96% of patients [18].
Ho et al. reported their preliminary experience with paclitaxel-coated balloon (SeQuent Please) in the PPCI setting for 89 patients. 70% had TIMI 0 flow pre-procedure, and TIMI III flow was achieved in 98% patients. Glycoprotein IIb/IIIa inhibitors were used in 80%, and thrombus aspiration was carried out in 56%. DCB-only PCI was carried out in 96%, while the other 4% had bail out stenting for significant acute recoil or dissections. They reported a death rate of 4.5%, MI 0%, and TLR/TVR of 0% at 30 days [19].
Nijhoff et al. in a subgroup analysis from the DEBAMI trial showed that there was no difference in major adverse cardiac events in 40 patients treated with DCB-only PPCI in comparison with BMS only, BMS + DCB, and paclitaxel-eluting stent implantation at 6 months follow-up [20].
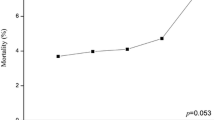
Wickramarachchi et al. in an abstract published at EuroPCR, 2017 in Paris, reported their experience in the use of DCB-only PPCI in an all-comer cohort of 253 patients. 4% of patients were in cardiogenic shock, and 6.7% were out of hospital cardiac arrests. 91% had DCB-only PCI. A 30-day mortality was only 2.4% and mortality for 379 days was 6.3%. For a mean follow-up period of 261 days, MI and TLR rates were 2.6% and 3.3%, respectively [21].
These publications suggest that DCB-only PPCI is a safe alternative to standard stent implantation in this high-risk group. We advocate this approach for several compelling reasons:
12.3.1 No Mortality Benefit with Stents
The use of BA in PPCI has been superseded by routine stenting in the contemporary era due to the reduction of TVR as mentioned before. However, DCB therapy addresses the issue of restenosis with its drug delivery reducing neointimal hyperplasia. An improvement of the quality in angiography and the use of potent antiplatelet therapy have reduced acute vessel closure rates. Currently, there are no studies showing a mortality benefit of stent implantation over balloon-only angioplasty or, in a majority of studies, a reduction of recurrent MI in this setting.
12.3.2 Risk of Stent Thrombosis
Studies have shown that the cumulative frequency of stent thrombosis (ST) following stenting with both BMS and DES for STEMI continues to increase beyond 1 year and that the frequency of very late ST may be higher with early-generation DES [16]. Moreover, the rate of stent thrombosis in patients undergoing PPCI can be high (ranging from 1 to 3% in contemporary trials). Patients with AMI have higher rates of stent-specific adverse events when compared to those with stable CAD. This could be related to coronary vasoconstriction and the presence of thrombus at culprit lesion site leading to suboptimal stent sizing and subsequent stent mal-apposition.
12.3.3 Inadequate Time to Know Patient’s History
Time pressure to open the occluded artery promptly in PPCI (shorter door-to-balloon times) may result in inadequate time to know patient’s full medical history. Routine stenting as per guidelines may therefore not be appropriate in some patients.
It remains a challenge to decide whether the patient is a candidate for a prolonged course of DAPT at the time of the PPCI. DES should be avoided in the presence of elevated bleeding risk, need for invasive or surgical procedures in the near future, and financial/social barriers that may limit patient compliance.
12.3.4 Avoidance of Long Stents in PPCI
DCB maybe a good alternative to treat diffuse lesions in PPCI as outcomes remain relatively unfavorable for stent-based coronary intervention especially those with de novo long CAD. Even in the DES era, studies have shown that the TLR rates can range from 6 to 28% for such lesion subsets with higher rates of instent restenosis for paclitaxel DES. Longer stent length is also recognized as predisposing factor for ST.
12.4 Technical Tips and Tricks with DCB-Only Angioplasty in Primary PCI
We recommend following the German consensus guidelines but with additional steps when successfully performing DCB-only PPCI [22].
12.4.1 Lesion Preparation
We recommend aspiration thrombectomy when faced with a high thrombus burden, i.e., TIMI thrombus grade 3 or more, aiming to reduce the thrombus burden to TIMI thrombus grade of 2 or less. A thrombus-laden lesion is more likely to hamper effective drug delivery to the vessel wall.
This should be followed by mandatory pre-dilatation of the lesion using semi- or non-compliant balloons with a balloon to vessel ratio of 0.8 to 1.0. This should be done carefully and slowly with enough pressure only to fully inflate the balloon (usually 6–8 atm). Liberal use of intracoronary nitrates is recommended as this helps accurate vessel sizing. We have a low threshold for the use of glycoprotein IIb/IIIa inhibitors in treating lesions with high thrombus burden. Also, acquisition runs after pre-dilatation should be of a slightly longer duration to carefully look for evidence of vessel-threatening dissections, in particular any contrast hang-up or accumulation within a dissection plane indicating a NHLBI type C dissection and possible early vessel closure due to intramural hematoma formation.
Coronary dissections are an inevitable result of BA, but most are microdissections that cannot be seen on angiography and are of no clinical significance. However, abrupt vessel closure remains one of the most fearful complications of BA usually associated with NHLBI dissection grades of type C and above. With a good knowledge of the different NHLBI grades of coronary dissection, careful selection of those patients suitable for DCB-only angioplasty is possible [23]. Ho et al. in their study reported no abrupt closure of the culprit artery. Only 4% of patients required bailout stenting for significant recoil/dissections of type C and above. Wickramarachchi U et al. reported acute vessel closure rate of 0.75% requiring bailout stenting and an overall bailout stenting rate of only 9%. The incidence of abrupt closure is also significantly reduced in the current era of more potent antiplatelet use.
12.4.2 Drug Delivery
If there are no dissections of more than NHLBI type C, TIMI III flow, and not more than 30% residual stenosis, drug delivery should be considered with the deployment of the DCB. DCB diameter should be the diameter of the largest balloon used to pre-dilate the lesion. The DCB should be used only for drug delivery and not for further angioplasty. It is good practice to check the guide catheter and wire position and ensure the O-ring is fully open before start delivering the DCB. Care should be taken not to touch the DCB prior to introduction. We recommend following manufacturer’s instructions for use to ensure adequate drug delivery. This will include maximum transit time to the lesion and balloon inflation times. In the case of a coronary dissection of type C or above after DCB use, we recommend bailout stenting with a second-generation DES rather than a BMS [24]. Figure 12.1 summarizes the key steps.
Proposed protocol for optimal use of DCB
The lesion should be aspirated if there is presence of intracoronary thrombus. The lesion should then be carefully pre-dilated. After check angiography, where there is TIMI-3 flow, dissection of grades A to B, residual stenosis of less than 30%, and TIMI thrombus grade no worse than grade 1–2, it is reasonable to proceed with DCB therapy. Alternatively, insertion of an intracoronary stent is likely to be required
12.5 Conclusion
In conclusion, the use of DCB as primary therapy in primary PCI represents a novel approach in treating STEMI patients. This approach is possible with appropriate patient selection and by performing two key preconditioning steps, namely, aspiration thrombectomy for lesions with high thrombus burden and careful lesion preparation. A randomized controlled trial (REVELATION) is underway to assess the safety and efficacy of a DCB-only strategy versus DES in primary PCI [25]. However, we would recommend performing DCB-only angioplasty in stable patients first, preferably with proctoring before treating such high-risk patient groups.
12.6 Primary PCI of RCA with Drug-Coated Balloon Angioplasty
Below is one detailed case illustration followed by pre-, immediate-, and post-DCB-only PCI images of two other cases.
12.6.1 History
A 47-year-old male smoker presented with inferior ST-elevation myocardial infarction (STEMI).
12.6.2 Baseline Coronary Angiography
The right coronary artery (RCA) showed 95% stenosis in mid-segment (culprit lesion site) and 70% diffuse stenosis in distal segment (Fig. 12.2).
12.6.3 Procedure
A 6 Fr sheath was inserted into the right radial artery, and the RCA was engaged with a 6 Fr Ikari left 3.5 guiding catheter.
A Runthrough NS guidewire was advanced into the right posterior descending artery. As there was minimal thrombus, aspiration thrombectomy was not performed. The mid- and distal RCA lesions were pre-dilated with a 2.5 × 15 mm balloon.
As POBA results were satisfactory (Fig. 12.3) and RCA lesions were diffuse in nature, we decided to treat these segments with drug-coated balloon (DCB).
Distal RCA was treated with a SeQuent Please Neo DCB 2.5 × 30 mm (inflated at 12 atm for 50 s) (Fig. 12.4).
Mid-RCA was treated with a SeQuent Please Neo DCB 2.75 × 30 mm (inflated at 12 atm for 45 s) (Fig. 12.5).
Final angiographic results were satisfactory (Fig. 12.6) with TIMI 3 flow restored at the end of the procedure. There was residual stenosis of 30% with no obvious dissection.
12.6.4 Restudy Angiogram
Restudy angiogram (Fig. 12.7) 9 months later showed widely patent RCA with positive remodeling observed in mid-RCA.
Optical coherence tomographic (OCT) imaging study (Fig. 12.8) showed a nicely healed plaque at mid-RCA (culprit lesion site).
Case illustration 2: Pre-, immediate-, and post-DCB-only PCI and follow-up angiography at 22 months of a 60-year-old male presenting with an anterior STEMI



Case illustration 3: A 53-year-old female presenting with a lateral STEMI. Pre-, immediate-, post-DCB-only PCI (showing a type b dissection) and follow-up images at 17 months showing a nicely healed dissection and an excellent result



References
Gruppo Italiano per lo Studio della Streptochinasi nell'Infarto Miocardico (GISSI). Effectiveness of intravenous thrombolytic treatment in acute myocardial infarction. Lancet. 1986;1:397–402.
Randomised trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction:ISIS-2. ISIS-2 (second international study of infarct survival) collaborative group. Lancet. 1988;2:349–60.
Chesebro JH, Knatterud G, Roberts R, et al. Thrombolysis in myocardial infarction (TIMI) trial, phase I: a comparison between intravenous tissue plasminogen activator and intravenous streptokinase. Clinical findings through hospital discharge. Circulation. 1987;76:142–54.
GUSTO Angiographic Investigators. The effects of tissue plasminogen activator, streptokinase, or both on coronary-artery patency, ventricular function, and survival after acute myocardial infarction. N Engl J Med. 1993;329(22):1615.
Chen ZM, Jiang LX, Chen YP, et al. Addition of clopidogrel to aspirin in 45,852 patients with acute myocardial infarction: randomised placebo-controlled trial. Lancet. 2005;366:1607–21.
Sabatine MS, Cannon CP, Gibson CM, et al. Addition of clopidogrel to aspirin and fibrinolytic therapy for myocardial infarction with ST-segment elevation. N Engl J Med. 2005;352:1179–89.
Grines CL, Browne KF, Marco J, et al. A comparison of immediate angioplasty with thrombolytic therapy for acute myocardial infarction. The primary angioplasty in myocardial infarction study group. N Engl J Med. 1993;328:673–9.
Weaver WD, Simes RJ, Betriu A, et al. Comparison of primary coronary angioplasty and intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review. JAMA. 1997;278:2093–8.
Grines CL, Cox DA, Stone GW, et al. Coronary angioplasty with or without stent implantation for acute myocardial infarction. Stent primary angioplasty in myocardial infarction study group. N Engl J Med. 1999;341:1949–56.
Stone GW, Grines CL, Cox DA, et al. Comparison of angioplasty with stenting, with or without abciximab, in acute myocardial infarction. N Engl J Med. 2002;346:957–66.
Le May MR, Labinaz M, Davies RF, et al. Stenting versus thrombolysis in acute myocardial infarction trial (STAT). J Am Coll Cardiol. 2001;37:985–91.
Sabate M, Cequier A, Iniguez A, et al. Everolimus-eluting stent versus bare-metal stent in ST-segment elevation myocardial infarction (EXAMINATION): 1 year results of a randomised controlled trial. Lancet. 2012;380:1482–90.
Raber L, Kelbaek H, Ostojic M, et al. Effect of biolimus-eluting stents with biodegradable polymer vs bare-metal stents on cardiovascular events among patients with acute myocardial infarction: the COMFORTABLE AMI randomized trial. JAMA. 2012;308:777–87.
Stone GW, Lansky AJ, Pocock SJ, et al. Paclitaxel-eluting stents versus bare-metal stents in acute myocardial infarction. N Engl J Med. 2009;360:1946–59.
Kastrati A, Dibra A, Spaulding C, et al. Meta-analysis of randomized trials on drug-eluting stents vs. bare-metal stents in patients with acute myocardial infarction. Eur Heart J. 2007;28:2706–13.
Brodie BR, Pokharel Y, Garg A, et al. Very late hazard with stenting versus balloon angioplasty for ST-elevation myocardial infarction: a 16-year single-center experience. J Interv Cardiol. 2014;27:21–8.
Scheller B, Speck U, Abramjuk C, et al. Paclitaxel balloon coating, a novel method for prevention and therapy of restenosis. Circulation. 2004;110:810–4.
Vos NS, Dirksen MT, Vink MA, et al. Safety and feasibility of a PAclitaxel-eluting balloon angioplasty in primary percutaneous coronary intervention in Amsterdam (PAPPA): one-year clinical outcome of a pilot study. EuroIntervention. 2014;10:584–90.
Ho HH, Tan J, Ooi YW, et al. Preliminary experience with drug-coated balloon angioplasty in primary percutaneous coronary intervention. World J Cardiol. 2015;7:311–4.
Nijhoff F, Agostoni P, Belkacemi A, et al. Primary percutaneous coronary intervention by drug-eluting balloon angioplasty: the nonrandomized fourth arm of the DEB-AMI (drug-eluting balloon in ST-segment elevation myocardial infarction) trial. Catheter Cardiovasc Interv. 2015;86(Suppl 1):S34–44.
Wickramarachchi U, Corballis N, Maart C, et al. Primary PCI with DEB-only angioplasty, first UK experience. EuroPCR, May 2017, Paris, abstract no: Euro17A-POS0364. https://abstractbook.pcronline.com/index/slide/abstract/364/search/deb: PCRonline.com 2017.
Kleber FX, Rittger H, Bonaventura K, et al. Drug-coated balloons for treatment of coronary artery disease: updated recommendations from a consensus group. Clin Res Cardiol. 2013;102:785–97.
Huber MS, Mooney JF, Madison J, et al. Use of a morphologic classification to predict clinical outcome after dissection from coronary angioplasty. Am J Cardiol. 1991;68:467–71.
Mok KH, Wickramarachchi U, Watson T, et al. Safety of bailout stenting after paclitaxel-coated balloon angioplasty. Herz. 2017;42:684–9.
Vos NS, van der Schaaf RJ, Amoroso G, et al. REVascularization with paclitaxEL-coated balloon angioplasty versus drug-eluting stenting in acute myocardial infarcTION-A randomized controlled trial: rationale and design of the REVELATION trial. Catheter Cardiovasc Interv. 2016;87:1213–21.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
This chapter is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
Copyright information
© 2018 The Author(s)
About this chapter
Cite this chapter
Wickramarachchi, U., Ho, H.H., Eccleshall, S. (2018). Drug-Coated Balloons in STEMI. In: Watson, T., Ong, P., Tcheng, J. (eds) Primary Angioplasty. Springer, Singapore. https://doi.org/10.1007/978-981-13-1114-7_12
Download citation
DOI: https://doi.org/10.1007/978-981-13-1114-7_12
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-1113-0
Online ISBN: 978-981-13-1114-7
eBook Packages: MedicineMedicine (R0)