Abstract
Background: Previous meta-analysis (Capodanno D, et al, 2012) concluded that in patients with non-valvular atrial fibrillation (NVAF) in world patients, novel oral anticoagulants (NOACs) significantly decreased incidences of all type of stroke and systemic embolism (SE) with similar risk of major bleeding compared to warfarin. But, it is unknown about efficacy and safety of NOACs compared to warfarin in East-Southeast Asian population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
I. Moderated poster
MP 1. The Efficacy and Safety of Novel Oral Anticoagulants Compared to Warfarin for Non-Valvular Atrial Fibrillation Patients in East-Southeast Asia. A Meta-Analysis of Randomized-Controlled Trials
Ervan Zuhri, MD, Oryza Gryagus Prabu, MD
Faculty of Medicine, Indonesia University
Background: Previous meta-analysis (Capodanno D, et al, 2012) concluded that in patients with non-valvular atrial fibrillation (NVAF) in world patients, novel oral anticoagulants (NOACs) significantly decreased incidences of all type of stroke and systemic embolism (SE) with similar risk of major bleeding compared to warfarin. But, it is unknown about efficacy and safety of NOACs compared to warfarin in East-Southeast Asian population.
Objectives: Because of differences in patient demographics and characteristics in East-Southeast Asian patients with world patients, efficacy and safety of NOACs compared to warfarin in East-Southeast Asian patients were evaluated.
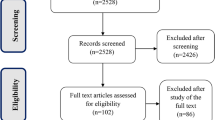
Methods: We systematically searched Medline, Embase, and Cochrane Registry up to August 2015 for double-blind randomized-controlled trials evaluating efficacy and safety of NOACs versus warfarin for NVAF in East-Southeast Asian patients. The primary efficacy endpoint was the incidences of all type of stroke and SE. The primary safety endpoint was the incidence of major bleeding. We not only evaluated primary efficacy and safety endpoint, but also evaluated secondary efficacy and safety endpoint. The secondary efficacy endpoint was incidences of hemorrhagic stroke, ischemic stroke, myocardial infarction (MI), and death from any cause. The secondary safety endpoint was incedences of intracranial hemorrhage (ICH) and clinically relevant non-major bleeding. Comparisons of all endpoint were expressed by Relative Risks (RRs) with 95% Confidence Intervals (CIs).
Results: Four double-blind randomized-controlled trials (n = 6.395 intention-to-treat East-Southest Asian patients) were included with duration of follow-up ranging from 1.8-2.5 years. Compared to warfarin, NOACs significantly decreased incidences of all type of stroke and SE (RR 0.68, 95%CI 0.55-0.85, P = 0.75, I2 = 0%), hemorrhagic stroke (RR 0.33, 95%CI 0.20-0.55, P = 0.14, I2 = 45%), and ICH (RR 0.32, 95%CI 0.20-0.49, P = 0.80, I2 = 0%). However, compared to warfarin, NOACs did not significantly decreased incidences of major bleeding (RR 0.79, 95%CI 0.54-1.17, P = 0.02, I2 = 70%), ischemic stroke (RR 0.95, 95%CI 0.73-1.24, P = 0.13, I2 = 47%), MI (RR 1.13, 95%CI 0.69-1.84, P = 0.52, I2 = 0%), death from any cause (RR 0.93, 95%CI 0.77-1.12, P = 0.47, I2 = 0%), and clinically relevant non-major bleeding (RR 0.79, 95%CI 0.52-1.21, P < 0.00001, I2 = 93%).
Conclusion: In East-Southeast Asian patients with NVAF, compared to warfarin, NOACs significantly decreased incidences of all type of stroke and SE, hemorrhagic stroke, and ICH with similar risks of major bleeding, ischemic stroke, MI, and death from any cause events.
Keywords: novel oral anticoagulants, warfarin, East-Southeast Asia, efficacy, safety.
MP 2. Length of AH Jump Associated with Elimination of Slow Pathway during Ablation of Atrioventricular Nodal Reentrant Tachycardia
Benny Togatorop, Sunu B Raharjo, Hananto Andriantoro, Dicky A Hanafy, Yoga Yuniadi
Division of Arrhythmia, Department of Cardiology and Vascular Medicine,
University of Indonesia, National Cardiovascular Center Harapan Kita Hospital
Background: Atrioventricular nodal reentrant tachycardia (AVNRT) is the commonest regular supraventricular tachyarrhythmia. Targeting the slow pathway (SP) has emerged as the superior form of treatment for atrioventricular nodal re-entrant tachycardia (AVNRT) for more than two decades. This technique has been found effective and is associated with a low complication rate. However, ablation of the slow pathway could result in either complete elimination or only modification of the SP (the presence of residual AH jump post-ablation). Unfortunately, long term observation of these two outcomes indicated that only modification of SP resulted in higher recurrence rate of the tachycardia.
Objectives: The aim of this study was to investigate whether the length of AH jump pre-ablation associated with the outcome of elimination/modification of SP.
Methods: The study patients included 56 patients with typical AVNRT (slow-fast), 20 males and 36 females, aged 44.2 ± 15.1 years. Slow pathway ablation was performed using a classical electro-anatomical approach. After ablation, AVNRT became non-inducible and anterograde atrioventricular (AV) conduction was preserved in all patients.
Results: Post ablation, non-inducibility of AVNRT was achieved in all 56 (100%) patients, with SP elimination in 33 (61%) patients and SP modification in 23 (39%) patients. Patients with SP elimination were older, had shorter sinus cycle length and longer AVNRT cycle length and had significantly higher number of cumulative junctional beats during ablation. Independent t-test showed that patients with SP elimination had significantly longer AH jump as compared with patients with SP modification (186.5 ± 97.7 msec vs 104.5 ± 56.4 msec, p < 0.001). Multivariate Cox regression analysis (adjusted with age, sex, cycle lengths, and cumulative junctional beat) showed that the length of AH jump was associated with complete elimination of slow pathway (RR 1.015; 95%CI 1.004 - 1.026, p < 0.05). Furthermore, ROC curve and multivariate analysis indicated that the length of AH jump of > 96 milliseconds had 13.3 times higher probability for complete elimination of the slow pathway (RR 13.3; 95%CI 2.9 - 60.9, p < 0.05) with a sensitivity of 81%, specificity of 65%, positive predictive value of 77%, and negative predictive value of 71%.
Conclusion: This study proved that the length of AH jump preablation is an independent predictor of slow pathway elimination during AVNRT ablation. Patients with the length of AH jump of > 96 msec had 13.3 times higher probability for complete elimination of the slow pathway as compared to patients with AH jump of < 96msec.
MP 3. Fishing For Silent Atrial Fibrillation for Secondary Prevention After Ischemic Stroke/Transient Ischemic Attack
Antonia Anna Lukito
Siloam Hospitals Lippo Village, Tangerang, Indonesia
Background & Objectives: Atrial fibrillation (AF) confers a high risk of recurrent stroke. Identify the best techniques to find silent AF is a crucial clinical need. Given the difficulties involved in detecting rare and often clustered episodes of paroxysmal AF, extended electrocardiographic (ECG) monitoring after an acute ischemic stroke improves the detection of paroxysmal atrial fibrillation.
Methods: We conducted a case series of fishing for silent AF in 5 patients who having acute ischemic strokes which were suggested embolic sources. The 7 days ECG monitoring (Spyder ®) were performed immediately after acute stroke.
Results:
Case 1: A 51 y.o. hypertensive female experienced sudden deafness due to second embolic ischemic stroke. Spyder ® monitoring was done and showed one episode of silent transient AF at day 7.
Case 2: A 61 y.o. hypertensive male experienced recurrent ischemic stroke. Spyder ® monitoring found a single episode of silent transient AF at day 7.
Case 3: A 43 y.o female with previous history of hyperthyroid had second ischemic stroke and Spyder ® found one episode of silent transient AF at day 5.
Case 4: A 57 y.o. male with dyslipidemia and transient ischemic attack (TIA), Spyder ® found 3 episodes of transient AF at day 5-7. Case 5: A 85 y.o male with mild hypertension and previous history of CABG, had ischemic stroke, Spyder ® found silent transient AF almost everyday.
Conclusion: Using this technique, transient AF was eventually detected in all of these patients. Since AF might be undiagnosed when asymptomatic and paroxysmal, systematically screening for silent AF for secondary prevention should be recommended in all patients after acute ischemic stroke. A 7-day continuous ECG monitoring after embolic stroke maybe associated with a greater detection of AF.
MP 4. Predicting The Type of Heart Failure in Patients with Chronic Heart Failure Based on Electrocardiographic Features: Role of The Scoring System
Bagaswoto HP, Damarkusuma A, Krisdinarti L, Maharani E
Department of Cardiology and Vascular Medicine, Faculty of Medicine, Universitas Gadjah Mada, Yogyakarta-Indonesia
Background & Objectives: Heart failure divides into 2 types based on left ventricular function, i.e. heart failure with reduced ejection fraction (HFrEF) or systolic heart failure and heart failure with preserved ejection fraction (HFpEF) or diastolic heart failure. The mortality of heart failure patients has been widely known inversely related to the left ventricular systolic function. Supporting examination needed to distinguished these two types of heart failure. Previous study showed HFrEF have small possibility ( < 10%) to occur when an electrocardiographic (ECG) features showed normal results. This study aims to create a scoring system based on the ECG features to predict the types of heart failure in patients with chronic heart failure.
Methods: We performed a cross-sectional analytic study by analyzing ECG and echocardiography data from 110 subjects with chronic heart failure patients hospitalized at Sardjito General Hospital since April 2015. HFrEF is defined as heart failure with an ejection fraction < 40%.
Results: Of the 110 subjects, 50 people have HFpEF, while 60 people suffered HFrEF. Multiple logistic regression analysis showed some ECG variables that became independent predictor of HFrEF, i.e. LAH (OR 4,44), QRS duration > 100 ms (OR 12,65), RBBB (OR 0,109), ST-T segment changes (OR 4,35) and prolongation of the QT interval (OR 7,40). From statistical analysis, we got a score for each ECG variables above i.e. LAH (point = 1), QRS duration > 100 ms (point = 2), RBBB (point = -1), ST-T segmen changes (point = 1) and prolongation of the QT interval (point = 2). Furthermore, based on ROC curve analysis, we obtained a score for HFpEF -1 to + 3, while HFrEF has a score of + 4 to + 6 with sensitivity 76%, specificity 96%, positive predictive value 95%, negative predictive value 80% and accuracy 86%.
Conclusion: Scoring system derived from this study, including the presence or absence of LAH, QRS duration > 100 ms, RBBB, ST-T segment changes and prolongation of the QT interval can be used to predict the type of heart failure in patients with chronic heart failure with satisfactory sensitivity and specificity value.
Keywords: chronic heart failure, scoring system, electrocardiographic features, type of heart failure.
MP 5. Diagnostic Scoring System for Atrial Fibrillation in Ischemic Stroke
Eric Hoetama
General Practioner Dr. H Marsidi Judono General Hospital, Belitung
Background & Objectives: Atrial Fibrillation (AF) is the most common arrhytmia that is found in daily practices. Patients with AF have four- to five-fold increased risk of developing ischemic stroke compared to normal population. Diagnosing AF can sometimes be quite difficult especially in the setting of paroxysmal AF. Moreover, paroxysmal AF can also increase the risk of thromboembolic complications. Some cases of cryptogenic stroke are believed to be cardioembolic in origin which caused by occult AF. This study aimed to develop a simple scoring system to detect patients with ischemic stroke most likely to have AF, so that recurrent stroke can be prevented.
Methods: We conducted diagnostic study using cross sectional design. Total 173 subjects were gathered. Those subjects were patients with ischemic stroke admitted in Belitung or Ruteng General Hospital from January 2014 until August 2015. Data collected were subjects’ characteristics, hypertension, diabetes, obesity, dyslipidemia, smoking history, congestive heart failure (CHF), alcohol consumption, valvular heart disease, chronic obstructive pulmonary disease, myocardial infarct history, previous stroke, Modified National Institutes of Health Stroke Scale (mNIHSS) score, and left atrial diameter. We analyzed those data using bivariate and logistic regression multivariate analysis.
Results: Multivariate analysis showed significant relationship between AF and some of the variables, which are hypertension, diabetes, obesity, CHF, left atrial enlargement, age and mNHISS score. We developed 7-point scoring system derived from those variables. A cutoff score of 3 or higher has sensitivity 97,1% and specificity 54,3%. Also, this scoring system has Area Under the Curve (AUC) value of 88,9% (CI95% 83,1% - 94,7%).
Conclusion: This scoring system uses only clinical and echocardiography profile that are easy to do, so it can be utilized as a simple diagnostic tool to identify ischemic stroke patient who is likely to have AF. Future studies are needed to determine another possibly related parameters.
Keywords: Atrial fibrillation, ischemic stroke, diagnosis, scoring system.
MP 6. Early Experience in Cardiac Resynchronization Therapy for Advance Heart Failure Patients
Irlandi Meidhitya Suseno 1 , Astri Astuti1, Steven R Utomo2, Doni Friadi3,Muhammad Iqbal3, Beny Hartono3, Muhammad Munawar3
'Department of Cardiology and Vascular Medicine, Padjadjaran University, Dr. Hasan Sadikin Hospital, Bandung, Indonesia
2 Departement of Cardiology and Vascular Medicine, Samratulangi University, Manado
3 Binawaluya Cardiac Center, Jakarta
Background & Objectives: Cardiac resynchronization therapy (CRT) has been demonstrated as a beneficial therapy option in certain subgroups of chronic heart failure patients. It can improve left ventricular (LV) function, survival, and symptoms. Report ofbeneficial effect of this relative now modality in Indonesia is still lacking. And therefore our main objective is to evaluate characteristic of patients, including description of clinical respond and LV function pre and post CRT implantation.
Methods: This is a retrospective, single center and descriptive study. All patients underwent CRT implantation at our hospital are enrolled in this study. Before and up to 12 month after implantation, clinical response and echocardiography study is performed.
Results: During period of January 2008 until July 2015 there were 72 patients advance heart failure (HF) at our hospital were implanted CRT or CRT Defibrilator (CRT-D) and 85% of them was male. Recurrent VT history was demonstrated in 11% patients. The most frequently applied mode were CRT-DDD (56%) followed by CRTD-DDD (33%) while CRT-VVI and CRTD-VVI were 7% and 4% respectively. The mean age was 54 ± 13 years. Ischaemic cardiomyopathy was noticed as majority of etiology of heart failure (58%). In ischaemic cardiomyopathy group, 20 patients (47%) had underwent percutaneous coronary intervention (PCI), 9 patients (21%) had coronary artery bypass graft (CABG), both PCI and CABG in 2 patients (5%), and 13 patients (31%) had no revascularization procedure. Chronic kidney disease was diagnosed in 37% patients, hypertensive heart disease in 30% patients, diabetes melitus notice in 29% and 22% of them had dyslipidemia. Almost all patient (96%) were given therapy angiotensin converting enzyme inhibitor (ACE-I) or angiotensin receptor blocker (ARB), beta-blocker in 94% patients, and mineralocorticoid receptor antagonist (MRA) in 82% patients. Antiplatelet and statin therapy was given in 51% and 50% patients. Of all the patient underwent CRT implantation, only 72% (52 patients) had complete ECG and echocardiographic study pre- and post implantation. Pre implantation ECG shows Left bundle branch block (LBBB) morphology in 40% patients. The mean QRS duration was 135 ± 22 ms. Clinical improvement of NYHA FC were detected in 67% patients. Increasing LV ejection fraction (EF) > 15% occured in 23% patients, while improvement 10-14% and less than 10% were noted in 33% and 44% patients respectively. Less improvement in EF occured more frequent in non-LBBB group (38% vs 6%). Other echocardiographic parameters, LV End-Diastolic Diameter (LVEDD) was also measured, the mean LVEDD pre-implantation was 68.0 ± 10 mm and post-implantation was 64.7 ± 12 mm. In general, responder criteria including clinical and improvement of EF were documented in 79% patients.
Conclusion: This study gives characteristic and outcomes information of patients underwent CRT implantation. It could be used for further investigation in CRT implantation strategies development.
MP 7. Reducing Radiation Exposure in the Electrophysiology Laboratory Using 3D Mapping System in AVNRT Ablation
Yansen I, Nauli SE, Priatna H, Rahasto P
Department of Cardiology and Vascular Medicine Tangerang General Hospital
Background: Radiofrequency ablation (RFA) is considered a safe and effective therapy for both atrial and ventricular arrhythmias. The success of catheter ablation for “simple” arrhythmias has led to the development of ablation procedures for more “complex” arrhythmias, such as atrial fibrillation (AF) and ventricular tachycardia (VT) which makes longer procedure time and fluoroscopic exposure. While advances in catheter ablation technology (advanced mapping systems, intracardiac echocardiography [ICE], 3D image fusion, or 3D rotational angiography) have led to a reduction in the need for fluoroscopic guidance, patients and operators can still receive significant radiation exposure.1 Minimizing radiation according to the “as low as reasonably achievable” (ALARA) principle is therefore a critical element of the procedure.2 This can be achieved through raising operator awareness and optimizing technical settings of the x-ray system.
Objective: The Objective of this study is to compare fluoroscopic time and radiation exposure during ablation in patients with AVNRT using conventional ablation and 3D mapping ablation.
Methods: There are 8 consecutive patients with AVNRT that were included in this study. These patients were sent to our EP lab for SVT ablation. Seven patients were ablated using conventional EP system. One patient was ablated using 3D mapping system. In accordance to standard protocol , we use fluoroscopy to localize and observe the movement of the ablation catheter during RFA in conventional EP system while in 3D mapping system we use 3D monitoring to observe and monitor the movement of the ablation catheter. After each procedure we calculate the fluoroscopy time, cumulative Dose Area Product (DAP) and cumulative Air Kerma (AK). This numbers were measured by the system after each procedure. After that we compare between conventional EP system and 3D mapping system. We use the same settings of the x-ray system, the same number of catheters in all patients and the same operator.
Result: 7 patients were ablated using conventional EP system. The mean fluoroscopy time was 960.1 ± 612 seconds, cumulative DAP was 14592.6 ± 6559.7 mGy.cm2 and cumulative AK was 136.5 ± 44 mGy. We did ablation using 3D mapping system only in one patient. The fluoroscopy time was 247 seconds, cumulative DAP was 5035 mGy.cm2 and cumulative AK was 42.440 mGy.
Conclusion: The result of this study shows that 3D mapping system significantly reduce fluoroscopy time and also radiation exposure in patients undergone AVNRT ablation. Less radiation will benefit not only for patients but also for medical personal who involve in ablation procedure.
Keywords: radiation, dose area product, air kerma, AVNRT, 3D mapping.
MP 8. Snaring Technique for Difficult LV Lead Replacement on CRT
Hari Yudha, Yan Herry, Muzakkir, Hermawan, Hauda El Rasyid, Sunu Budi R, Dicky A. Hanafy, Yoga Yuniadi
Division of Pacing and Electrophysiology, Department of Cardiology and Vascular Medicine, Faculty of Medicine Universitas Indonesia—National Cardiovascular Center Harapan Kita, Jakarta, Indonesia
Background: In recent years, implantation of cardiac resynchronization therapy devices has significantly increased. Left ventricular (LV) pacing through the Coronary Sinus (CS) is the standard approach for cardiac resynchronization therapy (CRT). Many implanting physicians use an “over-the-wire” approach to LV lead placement that may not provide enough support for lead advancement into tortuous or stenosis vessels. New techniques have been described that utilize directional and support catheters to allow direct advancement of the lead into the target branch. We presented a unique and a very rare case with fractured of wire inside the LV lead. Challenging problem and technique during procedure such as how to put in the new LV lead replacement in to stenosis CS, and novel technique from femoral vein using snare catheter to catch the LV lead wire to support implantation of new LV lead.
Case Report: A 68-years old female was sent for LV lead reposition. She had been diagnosed with chronic heart failure with functional NYHA II-III from non ischaemic etiology with risk factor hypertension and menopause. CRT was done in 2014 due to low EF and left bundle branch block (LBBB) with QRS duration 178 ms, despite optimal medical treatment with angiotensin receptor blocker and beta blocker. Even though LV lead was put on the right place, we still couldn’t find the best tresshold. So operator decided to put the wire inside of the lead for support. After implantation, showed tresshold for right ventricular lead was 0.4 V, current 0.4 mA, R wave 9.7 mV with resistance 580 ohm. Atrial lead showed tresshold 1 V, current 0.6 mA, P wave 3.3 mV, resistance 516 ohm. LV lead showed tresshold 2.2 V, current 1.4 mA, resistance 464 ohm. Two months after implantation there was improvement of patient’s condition. From electrokardiogram showed biventricular pacing. Atrial lead, RV lead and LV lead from chest x-ray was on correct position.
Ten months after implantation she revealed shortness of breath during moderate activity and hoarse of voice but no history of seizure or syncope. Interrogation was done to find the best tresshold and P/R wave. After repetitive interrogation the electrokardiogram still showed evidence of lost capture (no biventricular pacing). Previous echocardiogram showed reduced LV contraction with LA (Left atrium) & LV dilatation, moderate MR (mitral regurgitation) and intraventricular dysynchroni. Laboratory found no prolongation of prothrombin time and INR. Because of that, we decided to put the patient for LV lead replacement. During the procedure, we found 3 sites of LV lead wire fractures at the proximal, mid and distal lead (Figure 1.A). Before implant of the new lead, we tried to put out the LV lead wire first. Several times we tried to evacuate the lead wire (Figure 1.B), but only the proximal and the mid lead wire was successful released. We decided to ignored a little part of fracture wire and decided to implant the new LV lead at posterolateral branch from previous LV lead. But, the LV lead couldn't reach the CS because of restrained.
We performed coronary venography and which showed severe stenosis at 2 places, at the proximal coronary sinus (CS), first closed to thebesian valve and the second at the proximal-mid CS (figure 2.A anad 2.B). So, we tried to cannulated the CS with guidewires first. Wiring at proximal until distal CS with runthrough NS and balance middle weight universal II was done. After successful wiring, predilatation with balon Sprinter at two side was done at proximal CS with 16-20 atm at 10-14 sec and distal CS with 16 atm at 30 sec (figure 2C and 2D). LV lead was tried to put in at the CS but still couldn't enter the mid-distal CS so we planned for snaring technique to picked up the lead from CS to the right atrium (RA) (figure 3).
Snaring technique was performed to catch the lead wire from femoral vein. Lead wire was continued to be encouraged from proximal-distal CS and we planned to put long sheath to the RA (figure 3.A, B). After long sheath was successful inserted at the RA, snare catheter was inserted from right femoral vein. LV lead wire was catched and holded on by snare catheter at the RA (figure 3.C). LV lead was successful implanted at the posterolateral branch of coronary vein (figure 3.D). After implantation we found the new LV lead tresshold was 2 V, current 2.3 mA, R wave 9.2 mV and impedance 483 ohm. After the procedure, LV lead was connected to the generator. During procedure heparin was given iv with adjusted dose from ACT. Antibiotic and skin closure was done after that and the patient was sent to recovery room with stablized condition.
Conclusion: New tools and techniques have greatly improved the efficiency and success rate ofLV lead placement. LV lead implantation likely needs to evolve from a strictly anatomically based procedure to a “targeted” implant strategy. Electrophysiologists should arm themselves with the best data before and during the procedure to guide proper lead placement for each patient. Modalities such speckle-tracking echocardiography to guide LV lead placement can be used. In our case, combining technique has been developed to optimalization the implantation lead. Conservative strategy for fractured wire of LV lead has been choosed for shortening the mean time of procedures. After implantation, reassestment must be done to evaluate the result of biventricular pacing and to see the complication after fragment of fractured wire was retained at CS. For further suggesstion, we need a tools and newer techniques to handle the fractured wire.
MP 9. A Comparison of Atrial Parameters in Sick Sinus Syndrome Between Younger and Older than 40 Years Old Underwent Permanent Pacemaker
Made Satria Yudha, Sunu Budhi Raharjo, Dicky Armein Hanafy, Yoga Yuniadi
Division of Arrhythmia; Department of Cardiology and Vascular Medicine University of Indonesia, National Cardiovascular Center Harapan Kita Hospital
Background: Sick sinus syndrome (SSS) is a term used for a variety of cardiac arrhythmias, occurring predominantly in the elderly, that result from a senescent sinus node resulting in intermittent sinus pauses and rare sinus arrest, but also by inappropriate and often intermittent bradycardia, tachycardia, and the frequent alternation between the 2 conditions (tachycardia-bradycardia syndrome). Sick sinus syndrome is generally a disease of aging. It is uncommon in younger age. Atrial parameters in pacemaker implantation especially threshold and p wave is thought to be different between younger than 40 and older than 40 year old because aging process may be associated with generalized atrial fibrosis.
Methods: We examined gender, pacemaker mode of pacing, RA implantation site, RV implantation site, atrial and ventricular parameters during permanent pacemaker implantation in 115 patients with sick sinus syndrome between years 2012-2013 registered in National Cardiovascular Center Harapan Kita. The subject then classified into two groups, < 40 and > 40 years old. The two groups compared with statistical analysis.
Results: 115 patients underwent pacemaker implantation due to sinus node dysfunction. 11 patients (9.6%) were younger than 40 years old, 104 patients (90.4%) were older than 40 years old. Atrial threshold were (mean ± SD) 0.54 ± 0.15 vs 0.66 ± 0.22, p = 0.061; atrial p wave 3.61 ± 1.29 vs 3.67 ± 1.95, p = 0.278; ventricular threshold were 0.68 ± 0.24 vs 0.69 ± 0.29, p = 0.767; ventricular R wave 9.86 ± 2.86, p = 0.767. There are no significant differences between gender, pacing mode, RV-RA implantation site, atrial and ventricular setting (threshold, P/R wave, current and impedance) between two groups.
Conclusions: There were no significant differences in atrial and ventricular parameters between two age groups. These results suggest relatively similar atrial conditions that predisposes patient to sick sinus syndrome is independent to the age group.
Keyword: Atrial parameters, sick sinus syndrome, permanent pacemaker.
MP 10. The Relationship between Pacing Thresholds and Site of Ventricular Pacing Leads
Septa Mariani, Reza Yudha, Indy Masfufah, Chaerul Achmad, Augustine Purnomowati, Toni M Aprami
Department of Cardiology and Vascular Medicine, Padjadjaran University, Dr. Hasan Sadikin Hospital, Bandung, Indonesia
Background: Finding an optimal position for the pacing lead would be facilitated if locations with low pacing thresholds, which is reduces the pacing current delivered by the pacemaker. Right ventricular apex (RVA) is prefer site for pacing than right ventricular outflow tract (RVOT) because of access and lead tip stability. But it causes ventricular activation from cardiac apex spread to base (opposite to normal ventricular depolarization). The most suitable site for pacing is posterior septal wall of the right ventricular outflow tract (RVOT) as a more physiological alternate site for pacing. The objective of this study was to test the relationship between pacing tresholds and site of ventricular pacing leads.
Methods: 61 subjects (46 subjects of RVA group, 15 subjects of RVOT group) who came to Hasan Sadikin hospital and needed permanent pacemaker between January 2014 until August 2015 were enrolled in this study. None of the subjects had clinical features of heart failure and LV ejection fraction less than 45%. Basic characteristic (age, gender, blood pressure, PPM type, diagnose) and lead characteristic (site, threshold, impedance, R wave, sense) would be presented in each group with significancy of differences. To knowing the correlation each variable, we did Pearson test if normal data distribution or Chi-Square Test if it wasn’t normal.
Results: This study had significant difference of pacemaker type (35(76,1%) vs 6(40%); p = 0,010), Ventricular threshold pacing (0.57 ± 0.14 vs 0.9 ± 0.26; p = 0,000), and Ventricular sense pacing (2.7 ± 0.8 vs 2.16 ± 0.99; p = 0,005) between RVA group and RVOT group. There were no significant difference of men (21(45,7%) vs 5 (33%); p 0,406), age (64,6 ± 15.7 vs 63.13 ± 13.27; p = 0,741), Systolic blood pressure (156,1 ± 21.7 vs 160.82 ± 30.79; p 0.572), impedance (1477 ± 548 vs 1521.07 ± 701.67; p 0,123), and R wave pacing (11.3 ± 6.1 vs 8.54 ± 4.55; p = 0,119) between both groups. Correlation analysis showed significant relationship between RVOT site lead implantation and Treshold pacing (p = 0,000).
Discussion: RV apex has remained the preferred site for pacing since it is easy to access and provided stable lead position. However, it can cause worsening of heart failure in patients because of ventricular dyssynchrony from apical pacing. RV apical pacing typically produces a wide LBBB pattern with negative QRS vector in leads I, III, aVF and positive in lead I. Lee et al showed myofibrillar disarray in canine models exposed to long term RV apical pacing. Tse et al demonstrated myocardial perfusion defects and regional wall motion abnormalities in patients with chronic pacing from RV apex. Alternate pacing site that would mimic the normal electrical activation is posterior septal portion of RVOT. An optimal position of a ventricular pacing lead is defined by low pacing thresholds. At similar pacing thresholds high pacing impedance additionally reduces the pacing current delivered by the pacemaker. We will expect the longevity improvement of battery implanted pacemaker.
Conclusion: Beside it will mimic the normal electrical activation, RVOT pacing appears to be an effective site of lead implanted pacemaker because of low threshold pacing than RVA pacing at similar impedance. It will improve the battery longevity of pacemaker.
II. Poster presentation
PP 1. Anticoagulant Usage for Patients with Atrial Fibrillation from Atrial Fibrillation Registry in a Single Center
Steven Alviano Yuwono 1 , K Marwali, ANM Wibowo1, D Hadi1, RW Putra1, Sunanto Ng12
1 Faculty of Medicine, Universitas Pelita Harapan, LippoVillage, Indonesia.
2 Siloam General Hospital, Lippo Village, Indonesia.
Background and Objective: Atrial fibrillation is well recognized to increase the risk of embolic stroke; hence, anticoagulation is recommended to substantially reduce this risk. Based On the European Society Of Cardiology (ESC) Guidelines, CHA2DS2-VASc Score can be used for embolic stroke prediction in atrial fibrillation patients And HAS-BLED score to assess bleeding risk. Physicians are recommended to prescribe oral anticoagulant for high-risk patients based on CHA2DS2-VASc score. The objective of this study was to evaluate anticoagulant usage for atrial Fibrillation patients In a Local secondary institution.
Methods: We performed a cross-sectional Consecutive study from January-July 2015 on patient diagnosed with atrial fibrillation included in Atrial Fibrillation Registry in a Single Center. Twenty-eight patients were included in the study while the remaining 12 with valvular etiology were excluded from the study. CHA2DS2-VASc Score and HAS-BLED Score were then assessed from each patient, where a score of > 2 and a score of > 3 from each score respectively indicate ‘high risk’.
Results: There were 14 (50%) male. Age, CHA2DS2-VASc score and HAS-BLED Score will presented as follow (median [Min.-Max.]): 59.11(37-94), 3(0-6), And 2(0-4) respectively. 20(71.4%) samples had a CHA2DS2-VASc score of > 2 and were considered as high risk for embolic stroke which 6(30%) patients received oral anticoagulant. The anticoagulant that was used was 100% vitamin K antagonist (VKA), 9(45%) did not receive any anticoagulant, 1(5%) received clopidogrel, 2(10%) received aspirin, and 2(10%) received dual antiplatelet therapy (DAPT). 1(50%) of those who receive neither anticoagulant nor antiplatelet was related to coronary artery disease etiology. 8(28.6%) Samples had HAS-BLED Score of > 3 and were considered as high risk for bleeding, 2(25%) received VKA, 5(62.5%) did not received any anticoagulant, 1(12.5%) received aspirin, and no patients received either clopidogrel or DAPT. Among All the patients, which were considered high risk based on their CHA2DS2-VASc score, 40% of them were also considered high risk according to their HAS-BLED score
Conclusion: More than half of patients (70%) with CHA2DS2- VASc Score of > 2 did not received oral anticoagulant despite the guidelines recommendation. Forty Percent of patients who have high-risk CHA2DS2-VASc Score also have a high-risk HAS-BLED score.
PP 2. Transcutaneous Pacing Pitfalls: Failure to Capture Transcutaneous Pacing in Patient with Acute Coronary Syndrome
Gadih Ranti Endamatriza 2 , RD Robin Hendra Wibowo2, Hasan Basri1, Gitta Puspita',Gugun Iskandar Hadiyat1, Chaerul Achmad, Augustine2 Purnomowati2, Toni Mustahsani Aprami2
1 Hasna Medika Cardiac Center, Cirebon, Indonesia
2 Cardiology and Vascular Medicine Department, Faculty of Medicine, Padjadjaran University, Bandung, Indonesia
Introduction: Transcutaneous pacing is a valuable therapy in emergency cardiac care and has emerged as a lifesaving procedure. According to 2010 ACLS AHA guidelines, transcutaneous pacing as first line for the treatment of symptomatic bradycardias with poor perfusions, especially in unstable patients. It’s imperative to acquire the knowledge and skill for utilizing the transcutaneous pacing.
Case Presentation: A 55 years old man was admitted to the emergency department complaining anginal chest pain since 3 days ago. Physical examination revealed heart rate of 29x/minutes and other examination within normal limit. Laboratory findings showed Troponin T > 2 ng/dL. ECG showed Junctional bradycardia and STEMI inferior. He was diagnosed acute inferior myocardial infarction and junctional bradycardia. The patient was treated conservatively and was to put transcutaneous pacing. This patient was given acetosal 162 mg, clopidogrel 300 mg, sulfas atropine and heparinization. After setting up the transcutaneous pacing, the ECG showed capture like rhythm but actually it was muscle pacing artifact. After the pacing current was increased, the capture was occurred. After this procedure patient was in stable condition with improving heart rate. On the fifth day, the ECG showed sinus rhythm and the patient discharged from hospital.
Discussion: In transcutaneous pacing electrical current is passed from an external pulse generator via a conducting cable and externally applied, self-adhesive electrodes through the chest wall and heart. In emergency situations transcutaneous pacing can serve as a therapeutic bridge until the patient is stabilized, an adequate intrinsic rhythm has returned or a transvenous pacemaker is inserted. But there are some problems in transcutaneous pacing which should be physician's first concern. Common problems are discomfort, failure to capture, under sensing, over sensing and a noisy ECG signal. In our patient, after we set up the transcutaneous pacing, ECG showed failure to capture. The most common reason for not obtaining capture is failure to increase the current sufficiently to electrically stimulate the heart. Capture thresholds are markedly vary among individuals and may change over time. Current should be increased to the lowest threshold for electrical capture. Other ways to overcome this problem are moving the pacing electrode to another place on the precordium which may facilitate capture. Determine if there were metabolic acidosis or hypoxia because those two conditions could prevent cardiac response to pacing. It is important to distinguish between electrical capture and artifact during pacing. Positioning the ECG electrodes as far as possible from the pacing electrodes should help to minimize the signal distortion. Transcutaneous pacing also cause some discomfort in our patient, most subjects have difficulty tolerating pacing when current is above 50 mA. Unfortunately, capture thresholds are generally above this level, therefore analgesia and sedation should be routinely considered for comforting the patients.
Conclusion: Prompt recognition of transcutaneous pacing indication, troubleshoot that may occur during pacing and how to solve those problems are integral part for the success of this critical procedure.
Keywords: transcutaneous pacing, failure to capture, acute coronary syndrome.
PP 3. Acute Anterior ST-Elevation Miocard Infarction after The Ablation Procedure on Patient with Premature Ventricular Complexes
Taka Mehi 1 , Darwin Maulana1, Ignatius Yansen2, Siti Elkana Nauli2, Pudjo Rahasto2, Hardja Priatna2
1 Departement of Cardiology and Vascular Medicine, Faculty of Medicine, Univeritas Indonesia/ National Cardiovascular Center Harapan Kita-Jakarta
2 Interventional Cardiologist of Tangerang General Hospital-Banten
Background: Premature ventricular complexes (VPCs) are ectopic impulses originating from ventricular wall that associated with many underlying cardiac condition, including ischemia. Various symptoms are associated with VPCs, and may overlapping with coexistence of another cardiac disease. It is known that myocardial ischaemia and infarction leads to severe metabolic and electrophysiological changes that induce silent or symptomatic life-threatening arrhythmias. This report showed if there was corelation between arrhytmia and the ablation prosedure, and also acute coronary syndrom that happened after the procedure.
Case disscussion: A 47 year old female came to the outpatient clinics with chief complaint palpitation since 1 month ago. There was no dyspnea on effort, orthopnea and paroxysmal nocturnal dyspnea. She had no experience of syncope, dizziness or chest pain, but seldom had she got chest and back discomfort while she was on activity. She said that she was diagnosed Impaired Glucose Tolerance (IGT) and hypertension since a few months ago, and has no family history of coronary artery disease and cardiomyopathy. On physical examination, an elevated blood pressuure 146/66 mmHg was found, but others were within normal limit. Electrocardiogram showed sinus rhythm with frequent PVC. Echocardiography found that the systolic function was descrease with EF 27%, Hypokinetic was found at anterior and anteroseptal segment of LV. Patient then diagnosed with PVC, IGT and stage I Hipertension and planned to perform electrophysiology study and the ablation. The ablation procedure was successful, but after 6 hour-post procedure care, patient complaint typical chest pain with changing ECG pattern that showed anterior ST elevation accompanied with Q wave morphology. Early PCI was performed in the next 6 hours, found there was a total occlusion at proximal LAD with collateral vessel from RPDA to distal LAD. After the implantation of BMS to the lesion, patient freed from the symptoms.
Summary: Reported an unexpected case of a 67 year old female came to the outpatient clinics with chief complaint palpitation and chest discomfort since 1 month ago, she had history of IGT and hypertension. The EP study and ablation then performed after diagnosed with PVC frequent. About 6 hours after the procedure, acute STEMI was happened, and found there was a total occlusion at proximal LAD, so then the PCI was performed with 1 BMS implanted.
Keywords: STEMI, post ablation, early PCI.
PP 4. Association between P Wave Dispersion with Diastolic Dysfunction Severity in Reduced Ejection Fraction Heart Failure Patient
Silitonga CY, Bagaswoto HP , Mumpuni H, Maharani E
Department of Cardiology and Vascular Medicine, Faculty of Medicine, Gadjah Mada University, Yogyakarta
Background: Diastolic Dysfunction is defined as functional abnormalities that exist during LV relaxation and filling. Diastolic dysfunction in heart failure may cause hemodynamic and morpholocigal changes in left atrium which can further causes significant morbidity and mortality. P wave dispersion is related to the nonhomogenous and interrupted conduction of sinus impulses intra and inter-atrially. This study aims to give broader knowledge whether P wave dispersion is related to severity of diastolic dysfunction in heart failure.
Methods: We performed a cross-sectional analytic study by analyzing p wave dispersion in 12 leads ECG and echocardiography data from 52 subjects with heart failure reduced ejection fraction (HFrEF) patients with sinus rhythm that hospitalized at Sardjito General Hospital since April 2015. P wave dispersions were calculated by measuring minimum and maximum P wave duration values on the surface electrocardiogram. HFrEF is defined as heart failure with an ejection fraction < 40%.
Results: The study was done in 42 males (80%) and 10 females (20%), with average age of 57 + 9.9 years old. Thirteen patients (25%) were in prolonged relaxation stage (stage 1) of diastolic dysfunction, 12 patients (23.1%) were in pseudonormal stage (stage 2) of diastolic dysfunction, and 27 (51.9%) were in restrictive pattern stage (stage 3). P wave dispersion was 50.92 + 17.6 mm in stage 1, 57.41 + 17.8 mm in stage 2 and 57.67 + 18.78 in stage 3 with p value = 0.5. As the severity of diastolic dysfunction increased, the p wave dispersion also increased but it does not show any statistically significance.
Conclusion: P wave dispersion is not significantly related to the severity of diastolic dysfunction in reduced ejection fraction heart failure patients.
Keywords: Heart failure, p wave dispersion, diastolic dysfunction.
PP 5. Atrial Fibrillation is Associated with Cognitive Decline Independently from Cerebral Infarct
Ricardo Adrian Nugraha 1 , Michael Jonatan1, Rina Judiwati2
1 Faculty of Medicine, Universitas Airlangga — Dr. Soetomo General Hospital, Surabaya
2 Department of Biomedics, Faculty of Medicine, Universitas Airlangga, Surabaya
Introduction: It is unclear if Atrial Fibrillation (AF) is an independent risk factor for mild cognitive impairment and dementia in elderly non-stroke patients. The association between AF and cognitive impairment prior to a first stroke has yet not been characterized. However, growing evidence shows that AF is also a risk factor for significant cognitive decline through a multitude of pathways. At the same time, cognitive decline could accelerate incidence of cryptogenic strokes in utreated AF.
Objective: To investigate if AF is associated with an increased risk for cognitive decline.
Methods: We screened abstracts and full-text articles from Medline and Cochrane General Database by searching from keywords and bibliographies. 11 RCTs and 2 prospective cohort studies were included. 80% of participants were male and mean age was 68 years.
Results: 13 studies with 588 subjects, of whom 63 (10.7%) had parossistic, persistent or permanent AF during 5 year of follow-up using Holter ECG monitoring. Parossistic AF tended to be at increased risk for cognitive decline compared to control group (hazard ratio [HR], 1.29; 95% CI: 1.00, 1.67). Persistent AF was independently associated with increased risk of incident cognitive decline compared to control group (HR = 1.42 [95% CI 1.17-1.72], P < .001). Permanent AF were at highest risk compared to control group (HR, 2.10; 95% CI: 1.40, 3.15 or HR, 1.97; 95% CI: 1.34, 2.87).
Discussion: There are some literatures explaining why AF could exacerbate cognitive decline. 1) Participants with AF had lower total brain volume compared with those without AF (P < 0.001). AF was associated with lower volume of gray and white matter hyperintensities (P < 0.001 and P = 0.008, respectively), but not of white matter hyperintensities (P = 0.49). 2) Analysis of inflammatory markers in AF patients revealed increasing in hs-CRP, FGF, G-CSF, GM-CSF, IL-1RA, IL-9, IL-13, IL-17, and IFNy compared to non- AF groups. These are correlated significantly with declining in the neurocognitive functions memory and speed.
Conclusions: In the absence of clinical stroke, people with AF are likely to reach thresholds of cognitive impairment or dementia at earlier ages. AF is independently associated with worsening cognitive trajectory, especially global cognition, short-term memory, naming, and information processing speed, among elderly.
Keywords: Atrial Fibrillation, Cryptogenic Stroke, Cognitive Impairment, Dementia.
PP 6. Catheter Ablation of an Epicardial Accessory Pathway via The Middle Cardiac Vein: a Case Report
Yansen I, Nauli SE, Priatna H, Tanubudi D, Rahasto P
Departement of Cardiology and Vascular Medicine Tangerang General Hospital
Introduction: Catheter ablation is the treatment of choice for Atrioventricular Reciprocating Tachycardia (AVRT) with a longterm success rate of 95%. However, ablation of accessory pathways (APs) can be challenging ex. Epicardial accessory pathway (AP). Epicardial AP are most commonly found in the posteroseptal (PS) and left posterior regions. This kind of epicardial AP results from a connection between an extension of the coronary sinus (CS) myocardial coat along the middle cardiac vein (MCV), posterior coronary vein (PCV), or the neck of a CS anomaly and left ventricular epicardium. Therefore, they can be successfully ablated only from inside the CS or its branches, if endocardial ablation fails. Majority (70%) of CS APs occur without a diverticulum or other venous anomaly, and the ventricular end is located close to the MCV or PCV.
Case Illustration: We reported a rare case of 28-year-old female with recurrent supraventricular tachycardia who was referred for an electrophysiologic study (EPS). No past history of any cardiac disease. Baseline ECG (Figure 1) showed normal sinus rhythm without any ventricular preexcitation. In EP lab, Induction of arrhythmia showed the orthodromic atrioventricular reciprocating tachycardia (AVRT) with posteroseptal AP (Coronary Sinus catheter 7-8) hence we did transseptal puncture and tried to ablate the left posteroseptal AP. However, left posteroseptal endocardial RFA attempts via transseptal puncture failed to ablate the AP. After that we tried to ablate the AP epicardially from coronary sinus branch. Mapping in the Middle cardiac vein (MCV) showed good result and RFA in this area (Figure 2) achieved successful ablation of ventriculoatrial conduction. Because of the close proximity of the CS ostium and posterolateral branch of the right coronary artery, caution should be exercised during RFA into the CS. Unfortunately we did not do CS venography to look for anomaly in CS branch.
Conclusion: We have reported a rare case of epicardial left posteroseptal AP that is successfully ablated in MCV.
Keywords: epicardial accessory pathway, ablation, left posteroseptal accessory pathway, middle cardiac vein, sinus coronaries.
PP 7. Certain Areas of Myocardial Ischaemia Have Higher Atrial Fibrillation Risk
Alexandra N 1 , Thengker A1, Hadi MW1, Lim H1,2, Lukito AA1,2
1 Siloam Hospitals Lippo Village, Tangerang, Indonesia
2 Pelita Harapan University
Background: The prevalence of atrial fibrillation (AF) keeps increasing, while AF itself increases morbidity and mortality. Coronary artery disease (CAD) is associated with AF. AF preceded by myocardial ischaemia has worse prognosis. By knowing the causative ischaemic area, clinicians would be able to make better risk assessments and decide early AF preventions. Scarcity of this data leads us to conduct this reasearch.
Methods: Research is conducted retrospectively through medical records from January 2014 until June 2015. Subjects with AF preceded by myocardial ischaemia are included. Exclusion criteria are thyroid dysfunction, premature complexes, valvular problems, pulmonary hypertension, and chronic obstructive pulmonary disease. Demographic, ischaemic area, and comorbids are recorded. Ischaemic area were carefully concluded from the combination electrocardiography images, and decreased wall motion from echocardiography.
Results: From 44 subjects, the most frequent ischaemic area is inferolateral (22.7%), followed by inferoanterior (18.2%), and anterior (18.2%). Most subjects were male (68.2%). Time interval from first diagnosed CAD to first diganoses AF in 46.7% subjects is < 1 year, 13.3% < 4 years, 6.7% < 3 years. The most common comorbids are hypertension (61.4%), dyslipidemia (40.9%), and chronic kidney disease (34.1%).
Conclusions: Inferolateral is the most frequent area preceding AF. AF preceded by myocardial ischaemia is found 1.46 times more often in men than in women. The most common comorbid is hypertension.
PP 8. Choice of Agents in Control of Atrial Fibrilation in Single Center Study
Kelvin Marwali 1 , Rico WP2, Angeline NMW2, Steven AY2, Dylan H2, Sunanto Ng1,2
1 Siloam General Hospital
2 Faculty of Medicine, Pelita Harapan University, Lippo Village, Indonesia
Background & Objective: The burden of atrial fibrillation (AF) is set to increase due to widespread aging population. The lack of data on AF and its management in the Indonesia highlight the need for a study of AF management in our region. This study aims to evaluate performance between various control agents.
Methods: A crossectional study from January to July 2015, 40 patients was collected concecutively (age median 59 (min – max 34 – 94), 22 (55%) female, 6 (15%) coronary disease, 15 (37,5%) hypertensive, 7 (17,5%) cardiomyopathy, 12 (30%) valvular, 9 (22,5%) heart failure) with stable atrial fibrilation who were admitted to our local secondary hospital. Patient was managed with class III antiarrhytmic drug, cardiac glycoside or none. Patient's heart rate and rhytm was reassessed in 24 hour and discharge.
Results: The findings of this study will be reported in the following (median [min-max]). In emergency 8 (20%) of the patients were managed with digoxin IV and 8(20%) amiodarone IV in ED. Heart rate on 125 (58-196) bpm reduced to 90 (58-163) bpm in 24 hour. During hospitalisation patient were prescribed with oral digoxin 20 (50%), amiodarone 1 (2.5%) and beta blocker 10 (25%) during hospitalisation respectively. Heart rate at discharge 85 (60-131) bpm and prescription of oral digoxin during discharge was 40% (n = 16) while those of beta blocker was 12.5% (n = 5). The rate of rhythm conversion to sinus rhythm was 2.5% (n = 1) in 24 hour and 10% (n = 4) at discharge.
Conclusion: Rate control was prefered rather than rhytm control in our local secondary hospital. Digoxin was the prefered agents for rate control although the guideline suggests beta blocker as first line agents.
PP 9. The incidence of Persistent Iatrogenic Atrial Septal Defect in Patients Post Transseptal Puncture During Ablation Procedure: a Prospective Study
Yansen I, Nauli SE, Priatna H, Rahasto P
Departement of Cardiology and Vascular Medicine Tangerang General Hospital
Background: Catheter ablation for treatment of cardiac arrhythmia has become a more and more important curative treatment option over the past decade. Several randomized studies have shown that catheter ablation is clearly superior to antiarrhythmic drug treatment in patients with paroxysmal and persistent atrial fibrillation.1 However, ablation procedure is highly invasive and is associated with relatively infrequent, but at times severe procedural complications.2 Among these complications, thromboembolic events may occur periprocedurally or post-interventionally.3 Although never explicitly assessed, persistent iatrogenic atrial septal defects (iASD) after transseptal access may provide a cause for such thromboembolic events during long-term follow-up through the route of paradoxic embolism. Transseptal catheterization is frequently performed to access the left heart during percutaneous cardiac procedures. The amount of damage to the interatrial septum and the risk of persistent iASD differ and depend on the tools, technologies, and approaches used for catheter ablation.4-5 Studies assessing the presence of a residual iatrogenic atrial septal defect (iASD) after transseptal catheterization with 8F transseptal sheaths have suggested that the majority of these iASDs close within 6 months.
Objective: The objective of this study was to assess the incidence of iASDs in patients undergoing transseptal puncture with a 8 F transseptal sheath in our center.
Methods and Results: There are 6 consecutive patients (4 men and 2 women) included in this study. All patients undergone transseptal puncture during ablation procedure. There are 4 patients with left accessory pathway and 2 patients undergone Atrial Fibrillation (AF) ablation. We use 8F long sheath (SL0, St. Jude Medical) and 71 cm Brockenbrough needle for transseptal procedure (St. Jude Medical). We only did single transseptal procedure in patients with left accessory pathway and double transseptal puncture in AF patients for circular mapping catheter and ablation catheter. We did the transseptal puncture using modified technique with coronary sinus decapolar catheter as guidance.6 No problem was found in transseptal puncture procedure. After the ablation all patients underwent transesophageal echocardiography (TEE) 1 month after the procedure to look for iASD. Majority of patients (86,6%) did not have iASD anymore. Only one patient (13,35%) who undergone AF ablation had 1 mm residual iASD. Our result strengthen previous study that show after 6 months most of iASD will close and in our study even earlier only one month.
Conclusion: Transseptal catheterization procedures with 8F transseptal sheath have a high spontaneous closure rate of iASDs in one month observation so is not associated with an increased rate of stroke/systemic embolization during long-term follow-up.
Keywords: iatrogenic atrial septal defect, transseptal, transoesophageal echocardiography.
PP 10. Clinical Characteristics of Atrial Fibrillation in Regional Heart Center
Citra Kiki Krevani, Hauda El Rasyid, Uvita Yulistin S, Tommy Daendes, Yerizal Karani, Masrul Syafri
DR. MDjamil Hospital, West Sumatera
Background and Objective: Atrial fibrillation (AF) is the most frequent sustained arrhythmia in clinical practice, affecting 1-2% of the general population with the prevalence increasing with age. Eventhought most of AF is not a life threatening arrhythmia, it become a serious problem because decrease quality of life. There is no data about clinical characteristics atrial fibrillation during hospitalization in DR. M. Djamil Hospital as a regional heart center in Sumatera. The aim of this study was to describe the characteristics of patients and initial management with atrial fibrillation (AF) enrolled in the Regional Heart Center of DR M Djamil Hospital, West Sumatera.
Methods and Result: From Agustus 2013 to July 2015, 147 hospitalized patients with ECG-documented AF were enrolled from medical record in Regional Heart Center of M Djamil Hospital. Clinical type of AF was reported as paroxysmal in 22, persistent in 90, and permanent in 16 patients or classified as a first episode in 14 patients. Heart failure is a concomitant disease in 65,3% AF patient, follow by hypertension (47,6%), valvular heart disease (29,9%) and coronary heart disease (12,7%). Most patients were hospitalized caused by AF rapid ventricular response (68,1%), acute heart failure (46,3%) and Acute Coronary Syndrome (14,9%) respectively. Rhythm control was being pursued in 48 patients (39.1%) with class III antiarrhythmic agents, while rate control (99 patients) mainly with beta-blockers (50,3%) and cardiac glycosides (44,9%) was pursued in the remainder of the patients. Dabigatran was given to 57% of patients and the others was given warfarin as tromboembolism event prevention. Embolic risk score is (CHAD2VaSC) more than 2 in 63,9% patients. Echocardiography showed left atrial dimention LAD) is 44 ± 70 mm with ejection fraction (LVEF) 54 ± 5%. The long of stay (LOS) patient is 5 ± 9 days.
Conclusion: AF Persistent was the most subset of AF that have been found in DR M Djamil Hospital, with the rapid ventricle respon at the first time of admission, with the rate control strategy as the most choosen as first approachment.
Keyword: Atrial fibrillation, rhythm control, rate control, anticoagulant.
PP 11. Comparison between Dabigatran and Warfarin in Risk of Bleeding in Patients with Atrial Fibrillation
Adrina Vanyadhita
Faculty of Medicine University of Indonesia, Jakarta, Indonesia
Background: Globally, atrial fibrillation affects 1-2% of the general population and it is considered as the most common sustained cardiac arrhythmia. Atrial fibrillation is associated with the occurrence of stroke and other thromboembolic events. Therefore, the use of antithrombotic agents is recommended in atrial fibrillation. Dabigatran is a new generation of anti-thrombotic that showed lower risk of major bleeding in patients with atrial fibrillation. Therefore, the aim of the study is to compare the risk of major bleeding in dabigatran and warfarin in patients with atrial fibrillation.
Methods: Literature searching was conducted using the database of PubMed and Cochrane. Studies regarding the comparison between dabigatran and warfarin in patients with atrial fibrillation with full- text availability, language in English and publication within the last 10 years were included. Ten studies fullfiled the criterion and included in the study.
Results: Six studies showed lower risk of major bleeding in patients using dabigatran compared with warfarin. Three studies stated there was no significant difference in major bleeding between dabigatran and warfarin. Two studies revealed higher risk of major bleeding in patients with atrial fibrillation and other comorbid conditions.
Conclusion: Our results suggested the beneficial use of dabigatran in the absence of other comorbid conditions with the dose of 110 mg, as it is associated with lower risk of major bleeding in patients with atrial fibrillation. For this patient, the use of warfarin is still preferable compared to dabigatran due to the availability of studies regarding the use of dabigatran in lowering the risk of major bleeding in patients with atrial fibrillation with comorbidity of valvular heart disease.
Keywords: Dabigatran, Warfarin, Risk of Bleeding in Patients, Atrial Fibrillation.
PP 12. Factors Affecting Sinus Rhythm Conversion in Patients with Non-valvular Recent Onset Atrial Fibrillation
Chandra Wijaya, Hauda El-Rasyid, Masrul Syafri, Yerizal Karani
Departement of Cardiology and Vascular Medicine, Faculty of Medicine Andalas University General Hospital of Dr. M.Djamil Padang
Background: Atrial fibrillation (AF) is a strong risk factor for death with an increase from 1.5 to 1.9 times in the analysis of Framingham. AF is also associated with an increase of 5 times the incidence of stroke. The strategy of FA in the early stage still maintaining sinus rhythm. Many studies have attempted to search for any factors that can predict whether the AF in patients with non valvular recent- onset FA can still return to sinus rhythm or not, but the results still debatable.
Method: This is a descriptive study with cross sectional analytic design. The subjects were all patients with non valvular recent onset atrial fibrillation ( < 72 hours). Univariate analysis test conducted by test unpaired T-test for numerical variables and chi-square test for categorical variables. Several factors are significant in the univariate analysis, followed by multivariate statistical test with logistic regression.
Result: From 68 subjects there were 36 patients (52.9%) with return to sinus. After univariate analysis showed 3 factors that influence the return to sinus rhythm. These factors include, Coarse AF (OR 0.30, 95% CI 0.11 to 0.82, P = 0.017) , LA diameter (OR 0.28 95% CI 0.10 to 0.77, P = 0.012), and LAV (OR 0.29, 95% CI 0.11 to 0.79, P = 0.014). Multivariate analysis showed influencing factors independently to return to sinus rhythm was Coarse AF (OR 3.68, 95% CI 1.16 to 11.66 P = 0.027) and LAV (OR 4.69, 95% CI 1.47 to 14.99 P = 0.009).
Conclusion: Coarse AF and LAVI is an independent factor for return to sinus in patients with non valvular recent onset atrial fibrillation.
Keyword: Non Valvular, Recent onset AF, Coarse AF, Fine AF, LAVI.
PP 13. Comparison between Rate-Corrected JT interval with Rate-Corrected QT interval to Predict Diastolic Dysfunction Severity in Heart Failure Patients
Maulana I, Bagaswoto HP, Mumpuni H, Maharani E
Departement of Cardiology and Vascular Medicine, Faculty of Medicine, Gadjah Mada University, Yogyakarta
Background: There has been little study of the ability of electrocardiography to evaluate the presence or absence of diastolic dysfunction (DD). It is known that prolonged rate-corrected QT (QTc) interval would be most closely associated with DD, given the temporal alignment of electrical repolarization and mechanical relaxation in diastole. Although QTc has been the standard measurement of ventricular repolarization, it includes both depolarization (QRS complex) and repolarization (JT interval), and may not always be sensitive indicator compared with rate-corrected JT (JTc) interval which represent only ventricular repolarization. Prolonged QRS duration can also gave DD because left ventricular dyssynchrony. This study will examine comparison between JTc and QTc to predict DD severity in heart failure patients.
Methods: We performed a cross-sectional study of 110 heart failure patients who went to Sardjito General Hospital from April to August 2015. The QTc interval was calculated using Bazett’s formula, and JTc interval was calculated by subtracting the QRS duration from the QTc interval. DD was assessed using echocardiography and classified into three categories (relaxation, pseudonormal and restrictive).
Results: Fifty-five (50%) patients have relaxation type, 26 (23.6%) as pseudonormal, and 29 (26.4%) as restrictive. JTc measurement was significantly difference between groups (relaxation type, 354 ± 34 ms; pseudonormal, 374 ± 60, restrictive 381 ± 41; p = 0.02). QTc measurement was also have significantly difference between groups (relaxation type, 457 ± 38 ms; pseudonormal, 487 ± 61, restrictive 509 ± 50; p < 0.001).
Conclusion: QTc interval and JTc interval were associated with diastolic dysfunction severity, but QTc interval was more superior than JTc interval to predict diastolic dysfunction severity in heart failure patients.
Keywords: Diastolic dysfunction, QTc interval, JTc interval.
PP 14. Atrioventricular Block in Patients with Hypertrophic Cardiomyopathy: A Case Report
Fadli Aditya Rizky 1 , Nuraini Yasmin2, Badai Bathara Tiksnadi3, Chaerul Achmad3
1 Department of Internal Medicine, Padjadjaran University, Bandung
2 Cardiovascular Division, Department of Internal Medicine, Padjadjaran University, Bandung
3 Department of Cardiology and Vascular Medicine, Padjadjaran University, Bandung
Introduction: Hypertrophic cardiomyopathy (HCM) is characterized by a thickening of the left ventricle which is not caused by an abnormal heart filling conditions. Atrioventricular block is a rare manifestation of HCM. We present an 18 year old male patient admitted to hospital due to an episode of syncope with history of recurrent syncope. Similar complaints are also experienced by father of patient who subsequently underwent placement of permanent pacemaker (PPM), but has died at the age of 37 years.
Method: We evaluated a patient with HCM and history of syncope accompanied by total atrioventricular block (TAVB). Electrocardiogram and echocardiography was performed. Patients then treated in the high care cardiac unit and underwent placement of PPM. Given the young age of the patient and the existence of similar complaints in the father of patient, then Arrythmogenic Right Ventricular Cardiomyopathy/ Dysplasia (ARVC/ D) is still considered as one of the etiologies of arrhythmias in this patients. We performed computed tomography (CT) scan with contrast angiography to exclude the etiology.
Result: The results of echocardiography showed a concentric left ventricular heart with a dilated left atrium. Left ventricular systolic function was 69% with a normal movement of the heart wall. Heart valves and right ventricular contractility was in the normal range. This result supports the diagnosis of non-obstructive HCM. Results CT scan showed thickening of the left ventricular wall which is accompanied by thickening of intraventricular septum that support a HCM. There was no evidence of ARVC/ D.
Conclusion: We have discussed the case of the occurrence of TAVB in an 18 years old male patient diagnosed with HCM. Prevalence of TAVB in HCM is very rare and the mechanism is not yet known clearly.
PP 15. Correlation between Demographic and Clinical Factors and Treatment Compliance in Patients with Atrial Fibrillation
Dylan Hadi 1 , K Marwali2, ANM Wibowo1, SA Yuwono1, RW Putra1 , Sunanto Ng1,2
1 Faculty of Medicine, Universitas Pelita Harapan
2 Siloam General Hospital, Tangerang, Indonesia
Background & Objective: Non compliance in patients is a worldwide problem and is multifactorial. Travel distance, age, gender and other clinical factors have been showed to be related to patient compliance to treatment. Our study aimed to examine the correlation between travel distance, gender, age and CHADSVASc as well as HASBLED score and patient compliance in management of atrial fibrillation.
Methods: The study was designed as a cross-sectional observational study with consecutive sampling done from January to July 2015. Thirty four patients that were diagnosed with atrial fibrillation were included. Their sex and age determined, CHA2DS2VASC and HASBLED score were calculated along with the distance between the patient’s home and the medical centre. We also included data for compliance defined on whether the patient came for the first follow up after their admission.
Results: The result was obtained on 34 samples and presented as follow [Median, [min-max)]: There were 20 females (58%) , distance to medical centres are [12,6 , (3,3-100)] , CHA2DS2VASC [2,58, (0-6)] and HASBLED [2, (0-4)]. Among 34 samples only 8 came back for their follow up, 5 samples died, and the rest did not return for their follow up. Of those 8 samples coming back for their follow up , 6 were females and 2 were males, age [54, (4278)], CHA2DS2VASC [2, (1-5)] , HASBLED [0, (0-4)] , distance results was available only to 6 of the 8 compliant samples [7.2 (5.448.7)]. Additionally, 7 samples came back for the second follow up visit. The correlations between age, CHADVASC , HASBLED, and distance to compliance related to initial follow up was insignificant with correlation coefficients of 0,141 , -0.25 , 0.206 ,0,336 and P values of0,425 , 0,888 , 0,242 , 0,117 respectively, while correlations to the second follow up visit were more significant with correlation coefficients of 0,258, 0,090, 0,318 , 0,176 and P values of 0,140 , 0,611 , 0,066 , 0,422 respectively. Interestingly the correlation of the initial follow up visit to the second follow up visit were vastly significant with correlation coefficients of 0,918 and (p value < 0.05)
Conclusions: There were no significant correlations between the patient’s distance to medical centre, sex and age to their compliance regarding the first follow up visit but there were significant correlation between the initial follow up visit with the second follow up visit.
PP 16. Correlation between Lipoprotein and Left Atrial Dimension in Patients with Atrial Fibrillation: a Cross Sectional Study
Hadi MW 1 , Thengker A1, Alexandra N1, Lim H1,2, Lukito AA1,2
1 Siloam Hospitals Lippo Village, Tangerang, Indonesia,
2 Pelita Harapan University
Background: Dyslipidemia is suggested to have association with atrial fibrillation (AF) and left atrial (LA) dilatation is associated with AF. However, several studies about association of dyslipidemia and AF are still unclear and controversial. Thus this study aims to know if there is correlation between lipid profile and LA diameter in patients with AF.
Method: In this cross sectional study we collected 64 medical records of patients with AF from January to July 2015 in our institution. We collected lipid profile and LA diameter from echocardiography studies. Lipid profile consists of total cholesterol, low density lipoprotein (LDL), high density lipoprotein (HDL), and triglyceride level. Diagnosis of dyslipidemia is based on Adult Treatment Panel III Cholesterol Guidelines and LA dilatation is defined as LA diameter > 40 mm using echocardiography.
Result: 41 patients (64.1%) have dyslipidemia (total cholesterol mean = 167.59 ± 47.80, LDL 107.87 ± 41.09, HDL 44.05 ± 11.54, triglyceride 114.72 ± 41.148) and 17 patients (26.6%) have dilated LA (mean LA diameter = 40.08 ± 8.50). Fisher's exact test showed no significant association between dyslipidemia and dilated LA (p > 0.05). Unpaired T test showed no significant association between lipid profiles and dilated LA (p > 0.05) and between dyslipidemia and LA diameter (p > 0.05). Bivariate analysis using Pearson’s test showed significant correlation between HDL level and LA diameter (r = -0.433, p < 0.05). No significant correlations between total cholesterol, LDL, triglyceride levels and LA diameter (p > 0.05).
Conclusion: 64.1% patients with AF have dyslipidemia and 26.6% have dilated LA. There is correlation between HDL level and LA diameter but no correlation between total cholesterol, LDL, triglyceride level and LA diameter in patients with AF.
PP 17. Correlation between Serum Uric Acid Level And Aortic Dimension In Patients With Atrial Fibrilation
Thengker A 1 , Hadi MW1, Alexandra N1, Lim H1,2, Lukito AA1,2
1 Siloam Hospitals Lippo Village, Tangerang, Indonesia,
2 Pelita Harapan University
Background: Increase serum uric acid (UA) has been shown directly promote and a marker of oxidative stress. Oxidative stress involve in cardiovascular disease such as aortic dilatation and Atrial Fibrilation (AF). Oxidative stress responsible for the regulation of matrix metalloproteins and smooth muscles apoptosis that play role in regeneration and destruction of aortic wall. oxidative stress also significantly changes the electrophysiological characteristics of Pulmonary Vein which is facilitate the occurence of AF. Previous study shows independent relationship between aortic root dimensions with increase of UA. This study tries to investigate the previous study in population of atrial fibrilation.
Method: A total of 28 Atrial Fibrilation patients consecutively taken from Siloam Hospital Lippo Village Medical Record from January to July 2015. Valvular problem were excluded in this study. The Aortic Root dimensions were measured using 2D Echocardiography. Serum UA level were included in patients laboratory result.
Results: 20 of 28 patients (71.4%) in normal serum UA level, 8 of 28 patients (28.6%) in high serum UA level. Bivariate analysis with Spearman correlation showed that there is significant correlation between serum UA level with Aortic Dimention (p = 0.001).
Conclusion: In conclusion, the serum UA levels were correlated with aortic root dimention in Atrial Fibrilation patients.
PP 18. Correlation between SCN5A Gene Mutation and Occurenceof Ventricular Fibrillation in Brugada Syndrome
Maulana R, Herman H, Maghfirah I, Alzahra' F, Putrinarita A, Nugraha F
Background: Previous studies have suggested that SCN5A mutation are associated with ventricular fibrillation leading to sudden cardiac death. Recent observation however have reported otherwise. Thus, the clinical importance of SCN5A mutation for developing ventricular fibrillation in Brugada Syndrome patients is not clear.
Objectives: This study aims to analyze the relationship of SCN5A mutation related to ventricular fibrillation in Brugada Syndrome patients.
Method: We searched PubMed, MEDLINE, EBSCO, ProQuest, Science Direct, Clinical Key, and Cochrane database for prospective RCT and Cohort studies that compare ventricular fibrillation events in SCN5A mutation in Brugada Syndrome patients. The meta-analysis was performed by RevMan 5.3 (fixed-effects model) to provide a pooled estimate for relative risk (RR) with 95% confidence intervals (95% CIs).
Results: Six clinical studies met our inclusion criteria and included a total of 452 patients, which 78 of them have ventricular fibrillation. There was no significant differences found in rate of ventricular fibrillation outcomes between Brugada Syndrome with or without SCN5A mutation. (risk ratio (RR) = 1.12; 95% CI = 0.71, 1.76, p = 0.64).
Conclusion: SCN5A mutation are not associated with the occurence of ventricular fibrillation in Brugada Syndrome parients. However, further investigation is needed to confirm these findings.
Keyword: SCN5A mutation, brugada syndrome, ventricular fibrillation.
PP 19. The Efficacy of Mechanical CPR Device Compared to Manual CPR on Rate of Return of Spontaneous Circulation (ROSC) in Cardiac Arrest Patients: A Meta-Analysis od Randomized Study
Maghfirah I, Herman H, Maulana R, Nugraha F, Pravian D
BACKGROUND: Recent studies demonstrated the use of automated mechanical chest device may enhance the rate of return of spontaneous circulation (ROSC) in patient with cardiac arrest. However, the effect of mechanical CPR versus manual CPR is remained controversial.
OBJECTIVES: This study aims to analyze the efficacy of mechanical CPR compared to manual CPR on ROSC rate during cardiac arrest.
METHODS: We searched PubMed, MEDLINE, EBSCO, ProQuest, Science Direct, Clinical Key, and Cochrane database for prospective RCTs that compare ROSC rate ofmechanical CPR and manual CPR in cardiac arrest patients. The meta-analysis was performed by RevMan 5.3 (random-effects model) to provide a pooled estimate for odds ratio (OR) with 95% confidence intervals (95% CIs).
Results: A total of 8 randomized studies (Mechanical CPR compared to Standard CPR) met the criteria for this meta-analysis. The studies included 6417 adult cardiac arrest patients treated by mechanical CPR and 7579 patients by manual CPR. There was no significant differences found in rate of return of spontaneous circulation (ROSC) between mechanical CPR and manual CPR (odds ratio (OR) = 1.13; 95% CI = 0.95, 1.36, p = 0.18).
Conclusion: Mechanical CPR is not superior to manual CPR in improving ROSC rate in cardiac arrest patients. However, these findings should be confirmed in large randomized controlled clinical trials.
Keyword: mechanical CPR, standard CPR, ROSC, cardiac arrest.
PP 20. Atypical AVNRT with bystander Septal AP: A Rare Case
Indy Mashfufah 1 , Mohammad Iqbal1, Maya Munigar Apandi1, Chaerul Achmad1, Beny Hartono2, Augustine Purnomowati1, Toni M Aprami1
1 Department of Cardiology and Vascular Medicine, Universitas Padjadjaran, Dr. Hasan Sadikin Hospital, Bandung, Indonesia.
2 Binawaluya Cardiac Center, Jakarta
Introduction: Paroxysmal Supraventricular Tachycardia with sudden onset and termination is relatively common. The major cause are AVNRT (approximately 50 to 60% of cases), AVRT (approximately 30% of cases), and AT (approximately 10% of cases). Preexcited tachycardia occur in up to 10% of patients with preexcitation syndromes. The usual mechanisms of regular preexcited tachycardia are atrial flutter or tachycardia, antidromic reciprocating tachycardia, and typical atrioventricular (AV) nodal reentry with bystander accessory pathway (AP). We present a unusual mechanism of PSVT, atypical (fast-slow) AV nodal reentry with bystander septal AP.
Case Report: A 46-year-old female had recurrent episodes of palpitations. She had non documented Paroxysmal Supraventricular Tachycardia and her resting electrocardiogram was normal. Electrophysiological study shown concentric retrograde atrial conduction with right ventricular pacing. Tachycardia was induced during atrial extrasystole which shown ventriculoatrial conduction 81 ms with AH/HA less than one.
We’ve done Zypes methode (Hys-synchronous Ventricular Extrastimulation) and Para Hisian pacing to differentiate between atypical AVNRT and AVRT due to septal Accessory Pathway. Zypes test showed atrial advencement and Para Hisian Pacing showed stimulation atrial time was almost the same which confirmed the existence of septal Accessory Pathway. The accessory pathway cannot be mapped during atrial pacing nor ventricular pacing. The decremental conduction and presence of retrograde dual atrioventricular nodal physiology giving the clue of atrioventricular nodal reentrant tachycardia as one of the mechanisme of tachycardia. So we ablated slow nodal pathway by radiofrequency. Following ablation, there was no evidence of retrograde dual AV nodal physiology and no tachycardia was inducible by atrial and ventricular pacing nor by isoproterenol infusion. The patient was remained arrhytmia free over a 2-month follow up.
Discussion: This case present retrograde dual AV node physiology in the presence of septal accessory pathway. It is important to recognize presence of AP as a bystander in preexcited atypical AVNRT. Following the ablation of slow nodal pathway, no tachycardia was inducible. So we conclude the mechanism of this PSVT was Atypical AVNRT with bystander septal accessory pathway.
PP 21. Atrioventricular Reentrant Tachycardia in a Child with Intermittent Ventricular Preexcitation
Nursidiq A.A 1 , Arifianto H.1, Purwaningtyas, N2, Wasyanto, T.2 Widjaja, S.L2
1 Resident in Cardiology and Vascular Medicine Department
2 Cardiology and Vascular Medicine Department 3 Cardiology sub division of Child Health Department Universitas Sebelas Maret/Dr Moewardi Hospital, Surakarta, Indonesia
Background: In ventricular preexcitation, an accesory pathway conducts electric impulse directly from atrium to the ventricle. Its incidence is 0.1 to 0.3% among the general population. The accesory pathway serve as a subtrate for reentry and caused atrioventricular reenterant tachycardia (AVRT).
Case Illustration: A 9 years old boy with history of recurrent palpitation came to emergency department due to palpitation. He had been diagnosed with supraventricular tachycardia and got bisoprolol but palpitation still reoccurred. In physical examination, we found tachycardia, with hemodynamically stable and he had no other abnormality. Electrocardiographic (ECG) showed orthodromic AVRT which caractherized with narrow QRS complex tachycardia with short RP interval. Vagal maneuver and intravenous adenosine was failed for terminating the AVRT. Intravenous amidarone was administered to terminate the AVRT. Post termination ECG revealed an intermittent ventricular preexcitation. Patient was discharge with therapy amiodarone amiodarone 100 mg twice daily and planed to EP study in referral hospital
Discussion: In our patient after AVRT was terminate, resting ECG showed intermittent ventricular preexcitation. It was indicate thatAVRT had mediated by accesory pathway. The mechanism of intermittent preexcitation has not clearly understood but is likely related to the refractory period of the accessory pathway as well as the cellular connectivity within the pathway. Intermittent ventricular preexcitation suggests poor antegrade conduction through the accessory connection. The finding of intermittent ventricular preexcitation indicates a long antegrade refectory period of the accessory pathway. Although risk of sudden death is low in intermittent ventricular preexcitation, it has been observed in some patients with cardiac arrest.
Medical treatment is effective but not addres the underlying cause. ß-blocker is the first line therapy. Amiodarone, flecainide, and sotalol could be choiced if ß-blocker is contraindicated or fails to control tachycardia. Radiofrequency ablation should be considerd particularly in patient older than 5 years old, especially in our patient its due to reecurent AVRT.
Summary: We reported orthrodromic AVRT in a child with intermitten ventricular prexcitation. Understanding the mechanism of arrythmia will lead to make diagnosis and plan of treatment.
PP 22. Depiction of Atrial Flutter Ablation in National Cardiovascular Center Harapan Kita 2010-2014
Wahyu Aditya, Hariyudha, Dian Larasati, Rima Sagita, Taka Mehi, Nana Maya Suryana, I Putu Parwata Jaya, Dicky Armein Hanafy, Yoga Yuniadi
Department of Cardiology and Vascular Medicine Faculty of Medicine, Universitas Indonesia, Divison of Arryhtmia, National Cardiovascular Center Harapan Kita
Aim: Catheter ablation of typical atrial flutter (AFL) has a high long-term success rate. However, the occurrence of new- onset atrial fibrillation (AF) after successful ablation of typical AFL is common. There is no data about the occurence of new onset AF after ablation of typical AFL in National Cardiovascular Center Harapan Kita, Jakarta.
Methods: Data was derived from medical record. Consist of 69 Atrial flutter patients treated with cavotricuspid isthmus (CTI) ablation in National Cardiovascular Center Harapan Kita, Jakarta during 2010- 2014. Typical AFL was diagnosed when ECG showed : readily visible & regular inverted flutter waves in the inferior leads, positive flutter waves in lead V1 and regular atrial rate between 240 and 340 bpm. Exclusion criteria: age < 18 years, contraindication to anticoagulation, prior nonpharmacologic interventions for AFL, prior documentation of AF. All available medical records and ECG documentation were reviewed carefully by investigators to exclude the presence of prior AF.
Results: There were 49 patients with typical atrial flutter who underwent CTI ablation. No major differences in baseline characteristics. Of 49 patients 93% were successfull CTI ablation. New onset AF was found about 16% during follow up.
Conclusion: There were 49 CTI ablation during 2010-2014. Successfull rate of CTI ablation was 93% and during follow up 16% patients became new onset AF
Keywords: Atrial Flutter, Cavotricuspid isthmus Ablation, Atrial Fibrilation.
PP 23. Electrocardiogram Strain Pattern in Heart Failure Patients: Is It More Associated with LV Dilatation or Hypertrophy?
Pratama R S, Bagaswoto H P, Mumpuni H, Maharani E
Department of Cardiology and Vascular Medicine, Faculty of Medicine, Gadjah Mada University, Yogyakarta
Background: The classic electrocardiogram (ECG) strain pattern has been well-recognized as a marker for left ventricular hypertrophy (LVH) and adverse prognosis in hypertensive patients. The strain pattern occurs frequently in heart failure patients. However, whether LV dilatation or hypertrophy in patient with heart failure is more strongly associated with strain pattern has been subject to controversy. This study was aimed to find stronger relationship between strain pattern to Left Ventricular Internal Dimension (LVIDd) or Left Ventricular Mass Index (LVMI) in patient with heart failure.
Methods: We conducted a cross sectional study between Januari 2015 - April 2015. We registered 110 patients diagnosed with heart failure with preserved ejection fraction (HFpEF) and reduced ejection fraction (HFrEF). Typical strain is considered when there is a downsloping convex ST segment in leads V5 and/or V6 with an inverted asymmetrical T-wave opposite to the QRS axis. In this study, LVIDd of > 52 mm and LVMI of > 115 g/m2 in male or > 95 g/m2 in female, measured by transthoracal echocardiography, is considered LV dilatation and hypertrophy respectively.
Results: Of 110 heart failure patients, there were only 37 patients with ECG strain pattern (33%, 26 males. Among patients with ECG strain pattern, 29 (78.4%) were presenting with LV dilatation and 33 (89.1%) with LV hypertrophy. We found that LV hypertrophy has stronger but statistically not significant association with ECG strain pattern (OR = 2.504, CI 0.776-8.078, p = 1.32) than does LV dilatation (OR = 2.389, CI 0.959-5.95, p = 0.08)
Conclusion: LV hypertrophy has stronger but statistically not significant association with ECG strain pattern than LV dilatation in patients with heart failure.
Keyword: strain pattern, heart failure, LV internal dimension, wall thickness.
PP 24. Electrocardiographic T-peak to T-end interval, is it related with severity of diastolic dysfunction in heart failure patients?
Damarkusuma A, Bagaswoto H P, Mumpuni H, Maharani E
Department of Cardiology and Vascular Medicine, Faculty of Medicine, Gadjah Mada University, Yogyakarta
Background: The costs of heart failure (HF) hospitalisations are known to be huge as it represents as end stage form of almost all cardiac diseases nonetheless of the origin aetiology. Hence, an improvement of the diagnostic tool and treatment is considerably needed. Diastolic dysfunctions by echocardiography marker in HF have been associated with adverse outcomes of the patients with HF. A study shown that ECG QTc interval has an association among HF with diastolic dysfunction. Recently, another study using animal models stated that ECG Tpeak to T-end (TpTe) interval could be more representative of transmural dispersion of ventricular repolarization than QTc interval. Since TpTe is not well established yet as diagnostic tool in this circumstance, this study will examine the association of the TpTe interval with the severity of HF based on diastolic dysfunction.
Methods: Cross-sectional study of the association between TpTe and diastolic dysfunction echocardiography markers in 67 heart failure patients who went to Sardjito General Hospital from April to August 2015 was performed. Thirty five (52.2%) patients were categorized as relaxation, 14 (20.9%) as pseudonormal and 18 (26.9%) as restrictive filling. TpTe on the resting electrocardiogram was measured using ImageJ software specifically in the lead V5. Afterwards, TpTe interval and echocardiograms markers were analysed blindly without knowing the identity or clinical entity of the patients. Diastolic dysfunction was assessed using pulse wave mitral inflow Doppler echocardiography and pulse wave tissue Doppler echocardiography of the septal mitral annulus in which are regularly used based on the existing guidelines. Furthermore, all analyses were done by using SPSS 21st version.
Results: Total 67 patients were included in this study with mean of age 57 ± 10.5 years old in which 3 grades were categorised as relaxation, pseudonormal, and restrictive filling with each mean of age 60.6 ± 9.4 years old, 52.5 ± 12.5 years old, and 55.06 ± 9.04 years old respectively. Due to abnormality distribution of the data, median was used instead of mean to describe the result of each TpTe interval in these grades comprises 123.43 ± 53.4 ms, 128 ± 48.2 ms, and 120.6 ± 50.1 ms respectively shown in relaxation, pseudonormal and restrictive filling categories. Furthermore, the pseudonormal and restrictive filling were combined to be described as “Moderate or greater dysfunction” while3 the relaxation was as “Mild dysfunction”. This analyses showed that increased TpTe was not associated with the degree of diastolic dysfunct (OR 0.997 [95% CI 0.982 to 1.012]; P = 0.654).
Conclusion: There is no association between TpTe interval and the diastolic dysfunction severity in patients with HF. Hence, a further study with larger sample is required to justify this method in order to diagnose the diastolic dysfunction severity on HF patients.
Keyword: T-peak to T-end interval, heart failure, diastolic dysfunction.
PP 25. Electrophysiological Characteristics and Radiofrequency Ablation in Patients with Right Ventricular Outflow Tract and Left Ventricular Outflow Tract Origin Premature Ventricular Contraction
AA SG Mas MeiswaryastLP 1 , Deddy KJ2, Dicky A.H3, Yoga Y3
1 Departement of Cardiology and Vascular Medicine, Faculty of Medicine, Udayana University.
2 Departement Cardiology and Vascular Medicine, Faculty of Medicine, Andalas University
3 Departement of Electrophysiology and Arrhythmia, Faculty of Medicine Indonesia University
Introduction: Premature ventricular contraction (PVC) is the most common cardiac arrhythmia in patients with or without any kind of diagnosed cardiac diseases. PVC is an extra heart beat originates from the ventricles and comes before the normal heart beat. Determining PVC characteristic is important for ablation procedure and it can help in pre-procedural planning and potentially may improve ablation outcome
Objectives: The aim of this study is to compare the electrophysiological characteristic and the results of radiofrequency ablation in patients with RVOT origin and LVOT origin PVC at National Cardiovascular Center Harapan Kita (NCCHK).
Subjects and Methods: This is a cross-sectional study that used the data from two years database in NCCHK. All patients who had undergone electrophysiology study and radiofrequency catheter ablation of RVOT origin and LVOT origin PVC at Division of Arrhythmia of NCCHK from January 2013-December 2014 were enrolled in this study.
Results: There were 63 patients which was consisted of 54 patients wth PVC of RVOT origin and 9 patients with PVC of LVOT origin. There were no significant differences of baseline characteristics between the two groups. The uncorrected QT interval was differ significantly between patients with RVOT PVC and LVOT PVC (202.33 ± 184.487 ms vs 356.25 ± 46.407 ms; p-value = < 0.001). There were no significant differences electrophysiological characteristics between both groups, such as AH interval, HV interval, Antegrade AV node ERP, Atrial ERP, Antegrade WP, Retrograde WP, and Retrograde AV node ERP. The success rate of catheter ablation of RVOT PVC group was 94.4%, and in LVOT PVC group was 77.8% (p-value = 0.002).
Conclusions: The uncorrected QT interval on patients with LVOT PVC was significantly higher than patients with RVOT PVC who had undergone electrophysiology study and radiofrequency catheter ablation at NCCHK. There were no remarkable differences of the electrophysiological characteristics in cases with RVOT PVC and LVOT PVC. The success rate of RVOT PVC ablation was considerably higher than LVOT PVC ablation.
Keywords: Right Ventricular Outflow Tract, Left Ventricular Outflow Tract, Premature Ventricular Contraction.
PP 26. Delayed Cardioversion of Ventricular Tachycardia Leads to Acute Kidney Injury
Albert Sudharsono 1, Sony Y Wibisono2
1 General Practioner Dr. Agoesdjam General Hospital, Ketapang, West Borneo
2 Internist-Nephrologist Dr. Agoesdjam General Hospital, Ketapang, West Borneo
Introduction: Ventricular Tachycardia (VT) is a life-threatening arrhythmia. VT refers to a series of 3 or more ventricular complexes occuring at rate of 100-250 beats/min. In patients with sustained VT and sign of unstable hemodynamic compromise, immediate synchronized cardioversion is required. Delaying the management of unstable VT more likely results to other organ impairment and ultimately sudden cardiac death.
Case Report: A 33 years old male was admitted to the emergency department with a chief complain of suddenly reduced of consciousness. Three days prior to his admission, he suffered fever; he just arrived from Java about one week. He was a healthy young man with no history of smoking, chest pain, hypertension, kidney disease or diabetes. When admitted, the blood pressure was 80/60 mmHg, weak pulse, irregular heartbeat, and body temperature 36,1oC. Peripheral blood count showed thrombocytopenia. The 12 lead electrocardiography showed a sustained ventricular tachycardia with RBBB and Right axis deviation. Due to unstable hemodynamic, cardioversion was proposed, yet it was refused by patient’s relative, waiting for patient’s family arrival. During hospitalization, warfarin 2 mg and amiodarone 0.5 mg/min were administered; norepinephrin and dopamine were titrated with initial dose 8 mcg/min and 10 mcg/ min, respectively. Kidney function impairment was shown gradually with increased creatinine serum from 2.2 mg/dl to 4.5 mg/dl, manifestation of melena, fever and deterioration of general condition. After 3 days of hospitalization, patient’s family finally signed consent to do the cardioversion, double 100J biphasic shock was conducted. Post cardioversion showed Sinus bradycardia and T inverted in lead II, III, avF. Patients regained his consciousness and undergone a hemodialysis twice regarding to his acute kidney injury. After the condition was transportable, patient was referred to hospital in Java for further examination.
Discussion: This case present an acute kidney injury due to delaying early synchronized cardioversion in VT case. Ventricular tachycardia was rarely found in young healthy population without prior underlying disease. Early cardioversion shows reduction of mortality outcome and other organ impairments in this case kidney. In addition, young patients without prior underlying disease shows better survival rate.
Keywords: Acute kidney injury, Cardioversion, Ventricular tachycardia.
PP 27. Expulsion of Generator Permanent Pacemaker due to Infection of Staphylococcus Aureus: a Case Report
Indra Wahyu Saputra, Ardian Rizal, Sasmojo Widito
Departement of Cardiology and Vascular Medicine, Faculty of Medicine, Brawijaya University/Dr Saiful Anwar Hospital, Malang, Indonesia
Introduction: Infection of the pacemaker pocket, the endocardial lead, or both, occurs in 1.9 per 1000 device-years of patients with permanent pacemakers. In cases of infection, pacemaker removal and lead extraction are necessary, but older leads may not come out with simple traction and might require a more complex approach to extraction, sometimes cause failure and and or complications.
Case Presentation: A 60 year old hypertensive and diabetic man had single chamber pacemaker implanted in July 2014 for complete atrioventricular block with symptoms of dizziness and syncope. On the 14th day post implantation, at the outpatient follow-up, he suffererd pain and erythematous skin at the operation site, and serosanguinous drainage was noted from a slightly open 1 cm surgical incision at the site of implantation. Local wound care was performed, cultures were obtained, and oral chloramphenicols for a possible wound infection were started. His wounds healed well, but this incident repeated at September 2014 and October 2014. The last outpatient follow up at May 2015, the patient presented with erosion of the pacemaker pocket and fully exposing of the pulse generator (figure 1). The pacer was still functioning well, pacing almost all the time. Then he was admitted to the hospital.
On the first day of the admission, the patient’s blood pressure was 140/80 mmHg and his body temperature was 37.2°C. Laboratory analysis revealed a white blood cell count of 11,220/ μL, a neutrophil count of 61%. A transthoracic echocardiogram performed did not show any vegetation. A therapy of chloramphenicol was initiated as an empiric antibiotic. 2 days later a temporary pacing wire was placed in the right ventricular apex via femoral approach. The next day the original pacemaker was removed and the leads extracted. Gentle manual extraction was applied in an attempt to remove the lead. Blood cultures from pus in the pocket were positive for Staphylococcus aureus. Present antibiotherapy was replaced by cefotaxim owing to susceptibility of the microorganism on culture antibiogram. The old pacemaker pocket of was debrided. After 3 weeks of antibiotic therapy and wound care, the patients finally agree to undergo a new pacemaker implantation on the opposite side. He was then treated for several weeks with antibiotics, his wounds healed well and he has now been followed for 2 months and has encountered no problems.
Conclusion: This case illustrates the benefit of pacemaker removal and lead extraction in the patient who had 1 year lead implantation with recurrent infection of the pacemaker pocket. This procedure was proven effective and safe with.
PP 28. Hypoglycemia Can Increase Risk of Cardiac Arrhythmia and Cardiovascular Mortality in Multimorbid Patients with Diabetes Mellitus Type 2
Ricardo Adrian Nugraha 1 , Michael Jonatan1, Rina Judiwati2
1 Faculty of Medicine, Universitas Airlangga — Dr. Soetomo General Hospital, Surabaya
2 Department of Biomedics, Faculty of Medicine, Universitas Airlangga, Surabaya
Introduction: Multimorbid patients with type 2 diabetes, who use insulin secretagogues and/or insulin, are in the very high risk group for getting cardiovascular complications associated with hypoglycemia. Several research have reported that an intensive glucose-lowering treatment, with insulin or sulfonylureas, is associated with an increased risk of hypoglycemia and may exert negative effects on the cardiovascular risk. The surge of sympathetic activity during hypoglycemic episodes may induce arrythmia, cardiac ischemia, and cerebral ischemia.
Objective: To review the correlation between hypoglycemia with non-fatal and fatal arrythmia from electrocardiographic changes by analyzing current clinical literature about safety considerations of tight glycemic control.
Methods: Comprehensive structured search on Pubmed and Cochrane database were conducted. All authors independently selected studies, extracted data, and assessed the methodological and evidence quality using the Cochrane Risk of Bias Table. Randomized control trial and human cohort studies were included. After conducting articles screening towards 31 abstracts according to inclusion and exclusion criteria, there were 21 articles left, in which 17 of them were included in this study. Data analysis was performed by RevMan 5.1.
Results: ACCORD trial showed an increase in all-cause mortality with intensive glycemic control, whereas the ADVANCE study and VADT showed no benefit with aggressive glycemic control. Chow (2014) reported 25 insulin-treated diabetic patients and monitoring 134 hours of recording at hypoglycemia, 65 hours at hyperglycemia, and 1.258 hours at euglycemia. Tachycardia and premature atrial/ventricular compelxes were significantly higher during hypoglycemia episode compared with euglycemia or hyperglycemia episode. Arrhythmias were more frequent during nocturnal than daytime hypoglycemia. In 12.537 diabetic patients from ORIGIN Trial, hypoglycaemia was associated with a greater risk for CV death (HR: 1.71; 95% CI: 1.27-2.30, P < 0.001) and arrhythmic death (HR: 1.77; 95% CI: 1.17-2.67, P = 0.007).
Discussion: Sympathetic response induced by hypoglycemia increases the risk of arrhythmias from Ca2+ overload, which occur with symphatetic stimulation. Patients who experience hypoglycemia are at an increased risk of silent ischemia as well as QTc prolongation (torsade-de-pointes) and consequent arrhythmias. Rapid fluctuations with a mean amplitude of glucose excursion (MAGE) > 5 mmol/l promote vulnerability of electrical stability of the heart, considered a proarrhythmic event.
Conclusion: Hypoglycemia, which is frequently asymptomatic and prolonged, may increase the risk of arrhythmia and CV death in patients with type 2 diabetes. There is a plausible mechanism that could contribute to increased cardiovascular mortality during intensive glycemic therapy. Targets for glycemic control need to be adjusted in patients who have history of hypoglycemia with a priority to stabilize glucose homeostasis without rapid fluctuations. Appropriate glycemic control represents one of the major goals of the therapeutic management of diabetes mellitus.
PP 29. Idiopathic Left Ventricular Tachycardia in Children
Ahmad Yasa1, Dicky Armein Hanafy2, Yoga Yuniadi2
1 Resident of Cardiology and Vascular Medicine, Faculty of Medicine, Universitas Sebelas Maret, Solo
2 Department of Cardiology and Vascular Medicine, Faculty of Medicine, Universitas Indonesia, Jakarta
Introduction: Ventricular tachycardia (VT) in childhood is uncommon, the incidence of VT at this age is low, approximately 0,2-1,8 in 10.000 children of school age, compared to adults. Idiopathic ventricular tachycardia (IVT) is ventricular tachycardia that occurs in the absence of clinically apparent structural disease. Incidence of idiopathic left ventricular tachycardia (ILVT) is approximately 10% - 15% of IVT. In this report, we present a rare case of ILVT in children.
Case Illustration: A healthy 10-year-old female patient presented with a 6-month history of recurrent attacks of palpitations. Patient was referred from private hospital, with diagnosis of supraventricular tachycardia. When she arrived at National Cardiovascular Center Harapan Kita, the ECG revealed normal sinus rhythm. Echocardiography confirmed normal anatomy and function of the heart, and laboratory showed no abnormalities. During electrophysiological study, ventricular tachycardia was easily induced by ventricular decremental pacing. The tachyarrhythmia showed RBBB morphology with superior axis and positive QRS axis in lead I indicating left posterior fasciculus VT. Mapping of posterior fasciculus showed diastolic potential 90 ms before QRS wave. Multiple radiofrequency ablation (RFA) were performed at this site and successfully eliminated ILVT.
Conclusion: A rare case, a healthy 10-year-old female patient was diagnosed idiopathic left ventricular tachycardia and successful ablation was performed at this case.
Keyword: children, idiopathic left ventricular tachycardia, radiofrequency ablation.
PP 30. Idiopathic Left Ventricular Tachycardia with STEMI Inferior: A Case Report
Melisa Ryska Sari 1, Ismugi2
1 General Practioner Raden Said Soekanto Hospital, Jakarta
2 Cardiologist Raden Said Soekanto Hospital, Jakarta
Introduction: Idiopathic fascicular left ventricular tachycardia (ILVT) has been characterized by its QRS morphology during VT (RBBB and left axis deviation) and represents 10-15% of all idiopathic left ventricular tachycardia. Most ILVT originates from the left ventricular endocardium, the origin of tachycardia was localized to a small region of reentry or triggered automaticity located in the posteroinferior left ventricle close to the posterior fascicle of the left bundle branch. Response to verapamil suggested a role for the slow inward calcium channel in the genesis of arrhythmia.
Case Illustration: A 44 years old man came to the emergency ward with chief complaint of palpitation and chest discomfort five days prior to hospitalization. He had a history of STEMI Inferior post PCI in 2006 and 2015 associated with ischemic heart disease. He was a former smoker and lack of physical activity. On physical examination, he was compos mentis, his temperature was 36,8 C, blood pressure was 110/70 mmHg , heart rate was 155x/minute and respiratory rate was 22x/minute and peripheral oxygen saturation was 98%.His conjunctiva were not anemic, and the sclera were not icteric. Jugular venous pressure was 5-2 CmH2O. On examination of cardiovascular system, no murmurs or gallop was found.The breath sound was vesicular in both lungs, with no rales and wheezing. His abdomen was soft with no palpable liver and peristaltic sound was normal. Extremities were warm and there were no pretibial edema in both feet. No peripheral cyanosis noted. The electrocardiography showed idiopathic left ventricular tachycardia, QRS rates was 155 bpm, PR interval cannot be interpreted. Note that the tachycardia exhibit a right bundle branch block (RBBB) pattern with a left superior axis. Chest x ray showed > 50% of cardiothoracic ratio with normal aortic segmen. Cardiac waist was flat, Apex downward. Basal congestion ( + ), Enlarged pulmonary vein ( + ) Primary percutaneous coronary intervention (PCI) was performed to this patient. It revealed 90-95% in distal right coronary artery (RCA), with significant 90% stenosis in diagonal branch of LAD (left anterior descending) and 70% stenosis proximal in left circumflexy coronary artery. A drug eluting stent (DES) 2,75x20 mm was implanted in distal to mid RCA. The patient was initially treated with intravenous amiodarone and successfully slowed the tachycardia but did not terminate it. Althouth it has given his haemodynamic stability, emergent electrical cardioversion was consulted to help guide initial pharmacological therapy and finally terminated the tachycardia with resultant normal sinus rhythm. Management of patient including administration of ISDN 3x5 mg, simvastatin 1x20 mg, bisoprolol 1x2,5, aspirin 80 mg o.d and verapamil 2x80 mg o.d.
Discussion: ILVT typically affects young males aged 15-40 years, who account for 60-80% of all cases. Symptoms typically include dizziness, palpitations, chest discomfort and occasionally syncope. Patients will often presents with peroxysms of VT making it difficult to diagnose and capture, although sustained VT does occur. Most episode occur at rest, though VT can also be triggered during elevated states of cathecolamine such as exercise emotional stress. Effectiveness of verapamil in suppressing this form of ILVT suggest a role for the slow inward calcium current.
Conclusion: Although intravenous administration is very effective, oral administration tends to exhibit variable success in long term suppression of ILVT. Radiofrequency (RF) ablation has been reported to have a higher success, lesser procedure time and fluoroscopy time.
PP 31. Interaction Between Chronic Neuroinflammation and Supraventricular Tachycardia
Michael Jonatan 1 , Ricardo Adrian Nugraha1, Rina Judiwati2
1 Faculty of Medicine, Universitas Airlangga — Surabaya
2 Department of Biomedics, Faculty of Medicine, Universitas Airlangga — Surabaya
Introduction: There is a strong relationship between autonomic nervous system and immune systems playing a prominent role in the initiation and maintenance of paroxysmal supraventricular tachycardia (PSVT) and significantly contributes to cardiovascular mortality. PSVT could be associated with neuroinflammation and increased sympathetic tone. Studies have shown consistent association between PSVT, proinflammatory cytokines and the cells of the innate and adaptive immune systems. Overactivity of the symphatetic nervous system, oxidative stress, and cyclooxygenases (COX) in the brain are implicated in the pathogenesis of PSVT.
Methods: We appraised several trials from Pubmed and Cochrane database to examine sources of heterogeneity, including difference in
clinical outcomes and exposure measurements. For studies that used similar sources of data over concurrent periods and similar age range, only the study with the largest data set was included in the meta-analysis.
Results: SNS overactivty, prorenin and norepinephrine cause T cells and monocytes/macrophages to accumulate in the brain and their vascularization. These cells release inflammatory cytokines, such as IL- 6, interferon-γ, and IL-17 that stimulate positive chronotropic to cardiac pacemaker. In rat models, PSVT exhibited significantly higher levels of TLR4 in the hypothalamus, especially in Paraventricular Nuclei (PVN). TLR4 inhibition within the PVN attenuated MAP, lowering heartbeat, reduced TNF-α, IL-1β, iNOS levels, and NFκB activity in SHR but not in WKY rats. These results were associated with a reduction in plasma NE and HMGB1 levels and an increase in IL-10 levels in SHR. We also found that chronic neuroinflammation, induced by either proinflammatory cytokine or l-NG-nitro-l-arginine methyl ester is accompanied by microglial activation as manifested by microgliosis and cathecolamine receptor upregulation in cardiac pacemaker cells.
Discussion: Inflammation of forebrain and hindbrain nuclei controlling the sympathetic nervous system (SNS) outflow from the brain to the periphery represents an emerging concept of the pathogenesis of neurogenic PSVT. Cathecolamine and prorenin were shown to increase production of reactive oxygen species and pro-inflammatory cytokines (interleukin-1 beta (IL-1β), interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α)) while simultaneously decreasing production of interleukin-10 (IL-10) in the paraventricular nucleus of the hypothalamus and the rostral ventral lateral medulla. Peripheral chronic neuroinflammation and SNS activity seem to share a common central mechanism contributing to an increase in sympathetic tone to SA node and AV node, entailing PSVT. Age, hypertension, diabetes mellitus could facilitate the penetration of peripheral immune cells in the brain parenchyma.
Conclusion: PSVT alone can facilitate the penetration of peripheral immune cells in the brain parenchym. We suggest that symphatetic overactivity itself encompasses feedback and feedforward mechanisms in the development of neurogenic PSVT while low-intensity, chronic peripheral inflammation of any origin may serve as a model of a feedforward mechanism in this condition.
Keywords: Neuroinflammation, Hypothalamus, PSVT, Symphatetic Overactivity.
PP 32. Late Presentation of Arrhythmogenic Right Ventricular Cardiomyopathy: An Unusual Case Report
Safir Sungkar, Faizal Yuwono, Pipin Ardhianto, Muhammad Arif Nugroho
Departement of Cardiology and Vascular Medicine, Faculty of Medicine, Diponegoro University Dr.Kariadi Hospital, Semarang, Central Java, Indonesia
Background: Arrhythmogenic right ventricular cardiomyopathy (ARVC) is an inherited myocardial disease affecting predominantly young people and manifests as sustained ventricular tachycardia with left bundle branch block morphology, sudden death or isolated right or biventricular heart failure. However, its first manifestation as sustained ventricular tachycardia in older patients without preceding symptoms of heart failure is infrequent. We report a 65 year old man presenting with ventricular tachycardia because of ARVC without preceding symptoms of heart failure.
Case Presentation: A 65 year old man was admitted to the hospital with symptoms of palpitation, chest discomfort and near syncope. The 12 lead electrocardiogram in the emergency departement showed a sustained ventricular tachycardia with left bundle branch block morphology and inferior axis. Because of hemodynamic instability, the patient was cardioverted to sinus rhytm with a single 150 J biphasic shock. Post cardioversion ECG showed sinus bradicardia with an epsilon wave in right precordial leads. Transthoracic echocardiography revealed extensive RV enlargement with regional wall motion abnormalities, reduce RV function (FAC 24.9%, TAPSE 1.02 cm) as well as LV function (ejection fraction 33%). Coronary angiography was performed and showed no abnormalities. Our patient had three major (RV aneurysm, epsilon wave and T wave inversion in right precordial leads) and one minor criteria (sustained LBBB type-VT with inferior axis) making the diagnosis of ARVC definite according to the revised Task Forced Criteria.
Discussion: ARVC is an inherited myocardial disease primarily affecting the right ventricle and is characterized by the gradual replacement of myocytes by adipose and fibrous tissue. At least 80% of cases are diagnosed before the age of 40, while our patient the diagnosis was made at 65 because of prior asimptomatic condition. Epsilon wave which found in 30% cases of ARVC was also present to our patient. The management of patients with ARVC is targeted toward prevention of sudden cardiac death and treatment of symptoms of heart failure. The three main treatments are antiarrhythmic drugs, catheter ablation and use of implantable cardioverter defibrillator (ICD). Beta blocker and ACE inhibitor was given to the patient and further planned for ICD implantation.
PP 33. The First Atrial Fibrillation Ablation in Tangerang General Hospital: A Case Report
Suryani LD, Tedjasukmana F, Yansen I, Priatna H, Rahasto P, Nauli SE
Department Of Cardiology and Vascular Medicine Faculty of Medicine Universitas Indonesia/ Tangerang General Hospital
Introduction: Atrial fibrillation (AF) is the most common cardiac tachyarrythmia and represents a major burden to healthcare systems. AF is associated with 4- to 5-fold increased risk of thromboembolic stroke. It is characterized by rapid (100-60 bpm), and irregular atrial fibrillatory waves (f wave) with an undulating baseline. AF is classified as paroxysmal, persistent, and permanent. Most episodes of paroxysmal AF are initiated from a focal source, usually in one of the pulmonary veins. Pulmonary vein isolation is recognized as potentially curative treatment for AF.
Case presentation: A 48 year-old woman admitted to outpatient clinic of Tangerang General Hospital with chief complaint of palpitation accompanied with shortness of breath since 1 month before admission. From previous hospital, she has been diagnosed with paroxysmal atrial fibrillation (AF), treated with verapamil 2x40 mg and planned for ablation. She had normal physical examination, the blood pressure on admission was 132/82 mmHg, resting ecg showed normal sinus rhythm. Transthoracal echocardiography revealed normal cardiac chambers without left atrial dilatation, good LV function (EF 68%), good RV function and no sign of thrombus formation. After exclude left atrial (LA) appendage thrombus with transesophageal echocardiography, we then decided to perform electrophysiology study and catheter ablation. Using double transeptal puncture with Brockenbrogh needle, we placed halo catheter in left atrium (LA) to constructed LA geometry and identified right and left pulmonary vein. We performed PV isolation (PVI) at the PV-LA junction (annulus PV) from left to right pulmonary vein. Evaluation after PVI showed entrance and exit block, and there was no inducible arrhythmia.
Conclusion: This is the first catheter ablation for AF that we performed in Tangerang General Hospital. Using double transeptal puncture, we did the PVI at the PV annulus to this patient and came with good result.
Keywords: atrial fibrillation, catheter ablation, pulmonary vein isolation.
PP 34. Mortality in ST-elevation Myocardial Infarction Complicating High-degree Atrioventricular Block Underwent Revascularization: A Meta Analysis
Oryza Gryagus Prabu MD, Ervan Zuhri MD
Faculty of Medicine Universitas Indonesia
Background: Acute coronary syndrome is a major cause of mortality around the globe especially in ST elevation myocardial infarction (STEMI) cases. However, it can be reduced if the treatment strategy was done in the effective way such as revascularization therapy with the choice of thrombolytic or percutaneous coronary intervention (PCI). High-degree atrioventricular block (HAVB) was likely be found in those patients. Thus, limited data was found in mortality rate of STEMI patients complicating HAVB who were underwent the revascularization treatment.
Objective: The purpose of this study is to compare the mortality rate among patients with STEMI who were underwent the revascularization treatment with either complicated with high-degree atrioventricular block or no atrioventricular block.
Method: We conducted a search for all published articles in Pubmed, yEmbase, and Cochrane databases with the specific terms and similar phrases of STEMI patients with complicating high degree atrioventricular block and did the revascularization strategy. The primary outcome is to determine the all-cause mortality in patients who were complicated with high degree atrioventricular block compared to the patients who were absent of the atrioventricular block. The results then presented in relative risk (RR) and 95% confidence interval (CI).
Result: Five observational studies were eligible for this study in which three of them did the PCI treatment while the other two did the thrombolytic treatment instead. The all-cause mortality in PCI studies were higher in HAVB-complicated patients than in no HAVB patients with RR 3.19 (95% CI 2.35-4.34, I2:58%). Furthermore, in the thrombolytic studies, same value was observed with higher mortality was found in HAVB-complicated patients with RR 3.40 (95% CI 2.12-5.45, I2:84%). While the cumulative revascularization therapy with RR 3.27 (95% CI 2.524.25, I2:64%).
Conclusion: Patients with STEMI complicating high-degree atrioventricular block had significant higher mortality compared to no high-degree atrioventricular block among patients who were underwent the revascularization therapy. However, more studies are needed especially in comparing the reperfusion or no reperfusion strategy among patient with HAVB-complicated STEMI.
PP 35. Suggested Viral Infection-induced Supraventricular Tachycardia (SVT) in Children: a Case Report
Satyadharma Michael Winata, Sari Novia Arifin
General Practioner Budhi Asih General Hospital, Jakarta
Introduction: Supraventricular tachycardia (SVT) is a rapid, paroxysmal regular tachyarrhythmia originates above the level of the Bundle of His that commonly involves the atrioventricular (AV) conduction system and an accessory pathway. This is the most frequent sustained dysrhytmia in children.1 Although some mechanism of SVT are associated with congenital heart disease, most children with SVT have structurally normal heart.2
Case: An 8 years old girl was admitted to our emergency medicine department with chief complaint of palpitation at rest and chest pain. Since two days prior admission, she had fever and productive cough. No limitation in activity before or any growth abnormalities. She was once experiencing the same symptoms but resolved spontaneously. She was stable, HR was > 150/minute, regular; no murmurs audible on cardiac physical examination. No sign of thyroid abnormalities. Complete blood count showed normal leukocyte level with slightly lymphopenia; normal electrolyte studies and chest x-ray. ECG revealed regular narrow complex tachycardia at 180/min and there were no P waves following the QRS complexes thus confirming SVT. Since vagal maneuver failed to change the heart rate, intravenous bolus of adenosine 0.05 mg/kg was given followed by a push of 10 ml normal saline. Rhythm reverted to sinus; simultaneously running ECG documented the change without any suggested pre-excitation. The child was started on bisoprolol 1,25 mg once daily and symptomatic medication; discharged the next day and advised a follow up one week later. During follow up, her echocardiogram showed structurally normal heart and no recurrent event complained. Bisoprolol then was discontinued and further evaluation needed if the symptoms reoccur.
Discussion: SVT is the most common symptomatic tachydysrhythmia in childhood and usually well tolerated in older children, although it can lead to cardiovascular collaps. Older children may complain of dizziness, chest pain or shortness of breath.3
Dual AV node pathways occurred significantly more often in older children.4 We found that this patient has a structurally normal heart, normal thyroid examination and electrolyte studies; also no recent medication has been used. In this case she has slightly lymphopenia which may suggested viral infection. Further viral culture needed to identify the viral type. Some cases reporting Respiratory Syncytial Virus may induce SVT in children but the mechanism are unclear.5The precipitating factor is often difficult to identify, but occasionally a febrile illness may precipitate an episode.6
Many re-entrant tachycardias can be managed with vagal maneuver. If fail then intravenous adenosine should be administered which is showed a high success rate(80%-100%) with minor and transient side effect.2,4 Beta blocker can be used for chronic management of SVT.2
Conclusion: SVT is an important condition for primary care clinicians to recognize and manage. Further evaluation of patient history and other examination needed to identify the etiology of patient with SVT that occurs or persists above 1 year of age due to its higher recurrency rate.7 The wide range of potential causes, beside congenital heart disease, like viral infection may induce SVT in structurally normal heart children.
PP 36. Electrophysiological Characteristics of Right Ventricular Outflow Tract and Left Ventricular Outflow Tract Origin Ventricular Premature Contractions at National Cardiovascular Centre Harapan Kita Jakarta From 2013-2014
AA SG Mas Meiswaryasti-P 1, Dicky A.H2 , Yoga Y2
1 Departement of Cardiology and Vascular Medicine, Faculty of Medicine, Udayana University
2 Departement of Electrophysiology and Arrhythmia, Faculty of Medicine, Indonesia University
Background: A ventricular premature contraction (VPCs) is the most common cardiac arrhythmia in patients with or without any kind of diagnosed cardiac diseases. It is an extra heart beat originates from the ventricles and comes before the normal heart beat. A VPCs is relatively a common event where the heartbeat is initiated by the other pathway rather than by the sinoatrial node (SA node), the normal heartbeat initiator. Determining VPCs electrophysiological characteristics is important for ablation procedure and it can help in pre-procedural planning and potentially may improve ablation outcome.
Objective: The objective of this study was to define the electrophysiological characteristics of right ventricular outflow tract (RVOT) and left ventricular outflow tract (LVOT) origin VPCs.
Methods: Sixty three patients who underwent radiofrequency catheter ablation (RFCA) for VPCs/VT from 2013 until 2014 at electrophysiology and arrhythmia department of National Cardiovascular Centre (NCC) Harapan Kita Jakarta were consecutive selected. The electrophysiological data were analyzed using SPSS 17.0 to find the difference of characteristics.
Results: There were fifty four patients with RVOT origin VPCs and nine patients with LVOT origin VPCs. We analyzed QT, QT corrected (QTc), right ventricular effective refractory period (RVERP), earliest activation (EA), and site of ablation from both RVOT and LVOT origin PVCs. There were significantly associated in QT and QTc between both groups (P = 0.0074, P = 0.0336, respectively); no significant association in RVERP and EA between both groups (P = 0.4101, P = 0.3843, respectively). Site ablation of RVOT origin VPCs mostly at anteroseptal (44%) and site ablation of LVOT origin VPCs mostly at non-coronary cups (NCC) (44%).
Conclussion: This study reavealed RVOT origin VPCs have longer QT and QTc interval than LVOT origin VPCs.
PP 37. Multiple Ablations in Wollf-Parkinson-White Syndrome: A Case Report
Tedjasukmana F, Suryani LD, Yansen I, Priatna H, Rahasto P, Nauli SE
Department of Cardiology and Vascular Medicine Faculty of Medicine Universitas Indonesia, Tangerang General Hospital
Introduction: It is estimated that the prevalence of paroxysmal supraventricular tachycardia (SVT) is 2,25/1000 persons in the United States. Atrioventricular reentrant tachycardia (AVRT) due to Wollf-Parkinson-White (WPW) syndrome is the second most common cause of SVT. Clinical decisions about the management of patients with WPW syndrome is based on whether the patient is symptomatic or asymptomatic. The radiofrequency ablation (RFA) is the method of choice in managing patients with WPW syndrome. The ablation of accessory pathways has greater possibility to recur than atrioventricular junction or atrioventricular nodal reentrant tachycardia leading to the need of multiple ablations.
Case Illustration: A 47 year old woman admitted to Tangerang General Hospital with a chief complains of palpitation. The complaint was not accompanied by chest discomfort or shortness of breath. She did have a history of hospitalization due to SVT. She was diagnosed with WPW syndrome. The physical examination was unremarkable. Her ECG showed a sinus tachycardia with short PR interval (0,10 s) and delta wave was noted. A positive delta wave and QRS complex in the V1, isoelectric delta wave in I and aVL were noticed suggesting an AVRT with a left lateral accessory pathway. The patient was then scheduled for ablation of the accessory pathway. The procedure was done by first inserting the quadripolar catheter to the His and right ventricle via left subclavian vein. We tried to canulate the coronary sinus (CS) to insert the decapolar catheter but we failed. The entrainment maneuver and right ventricular pacing were done, and it was confirmed that it was an AVRT. The ablation was done via retrograde approach. However, the ablation was failed and from the evaluation, the delta waves still existed. The second ablation was done one month after the first one. We punctured the right jugular vein and right femoral vein. We successfully canulated the CS and inserted the decapolar catheter. From the electrogram (EGM), it showed that the earliest point was coming from CS 1-2, confirming the left lateral accessory pathway. We used the transeptal approach and we did the ablation to the left lateral of the mitral valve annulus. The evaluation showed that there was no delta waves, there was a retrograde and antegrade block. The ablation was deemed successful. Two months after the ablation, the patient came back yet with another SVT episode, but the ECG showed no delta waves, suggesting that the previous ablation was successfully blocked the antegrade pathway but the retrograde pathway was still there. Then the third ablation was scheduled and done. We did the transeptal puncture, and the ablation was done in the area of left lateral of the mitral valve annulus. The evaluation showed that there was a retrograde block through the accessory pathway. In the follow-up, the patient had not had any episodes of SVT and the ECG was normal.
Conclusions: Multiple ablations were done successfully to block the antegrade and retrograde track of the left lateral accessory pathway in patients with WPW syndrome.
Keywords: Wollf-Parkinson-White Syndrome, supraventricular tachycardia, multiple ablations.
PP 38. Narrow QRS Tachycardia in a man presenting with Congestive Heart Failure: a case report
Wira Kimaseha Anggoro, Galuh YF, Ardian Rizal, Pawik Supriadi
Departement of Cardiology and Vascular Medicine, Faculty of Medicine Brawijaya University, Saiful Anwar General Hospital
Background: Arrhythmia is a condition where there is an abnormality in the rhythm of the heart, either its regularity or its heart rate. Tachyarrhythmia is the term to define a heart rate that is faster than normal and bradyarrhythmia is the opposite. Tachyarrhythmia can occur in patients with heart abnormalities, particularly congestive heart failure. It can definitely worsen the underlying congestive heart failure and also lead to death. Immediate and prompt treatment should be given.
Case report: A 35 year old male was admitted to the hospital with a complain of progressive shortness of breath for several days. One day prior to his admission, he complained of palpitation. He was not a drug user and also denied any history of syncope or other comorbidities. The initial ECG showed a narrow QRS tachycardia with a ventricular rate of 180 beat per minute. Immediate cardioversion could not be peformed. Intravenous adenosine bolus was administered three times with a doses of 6 mg, 8 mg, and 8 mg. It failed to convert the rhythm. Ten miligrams diltiazem was given intreavenously, but it also didn’t succeed. Amiodarone was chosen as the last line of therapy, where bolus of amiodarone was given intravenously and followed by 24 hours of maintenance. The rhythm convert to atrial fibrillation with rapid ventricular response and it persisted until the amiodarone maintenance drip was finished. Rapid digitalization was given to control the rate and then switched to oral digoxin. Concomitant heart failure therapies were also given. The last ECG before discharge showed atrial flutter with a ventricular rate of 97 beat per minute. The patient was discharged with bisoprolol 5 mg once daily, captopril 50 mg three times daily, spironolactone 25 mg once daily, and furosemid 40 mg once daily.
Conclusion: Tachyarrhythmia was commonly found in patient with congestive heart failure. In this case, we presented a case of narrow QRS tachycardia. Adenosine was not successful in converting the rhythm, suggesting that reentry supraventricular tachycardia was unlikely. The rhythm converted to atrial fibrillation only after the administration of amiodarone. Then it converted to atrial flutter after digoxin administration and persisted until discharge.
Keywords: ECG, palpitation, narrow QRS tachycardia, atrial flutter, congestive heart failure.
PP 39. Non Responder CRT in Dilated Cardiomyopathy Patient with Atrial Fibrillation A 35 Years Old Men: A Case report
Hendiperdana MR 1 , Eganata1, Yugo D2
1 Internship doctor at Pupuk Kaltim Hospital, Bontang, East Kalimantan.
2 Cardiologist at Tarakan General Hospital, Tarakan, North Kalimantan
Introduction: In multiple meta-analysis, CRT showed a promising treatment modalities in reducing mortality and rehospitalization rate. Even so, CRT candidates are mandated to a strict prequisites before implantation. De novo implantation of CRT in patients that indicated for PPM is still unclear.
Case Presentation: A 35 year-old male, diagnosed as dilated cardiomyopathy (EF 25%) since 2011. He also has slow ventricular response AF and a large LA thrombus. The patient is indicated for PPM implantation. Thus he undergone a de novo CRT implantation and AV nodal ablation due to his AV node dysfunction, AF, and low cardiac performance. After CRT implantation the patient condition still have a frequent re-hospitalization rate with low NYHA functional class.
Discussion: The additional benefit of biventricular pacing should be considered in patients requiring permanent RV pacing for bradycardia, who have symptomatic HF and low LVEF. That is the main reason for this patient whose QRS duration is < 120 ms without LBBB morphology to have this CRT implantation. Multiple clinical trials showed that an upgraded CRT from conventional PPM or a de novo CRT implantation showed a better outcomes in terms of mortality, clinical outcomes, and rehospitalization rate. In those trials, the patient has conventional bradycardia indications, severe symptoms of HF, and depressed EF, similar to this patient. But this patient has no AV synchrony due to AV nodal ablation. The AV synchrony might have a significant role in CRT implantation. The lack of large prospective trials in this area have to count into consideration.
Conclusion: The beneficial effect of CRT implantation in population is based on several preexisting condition. QRS duration < 120 ms, non-LBBB ECG pattern, and loss of AV synchrony have no proven evidence of beneficial effect.
PP 40. Predicting Left Atrial Enlargement by Electrocardiography from Echocardiography Finding
Jomansyah MUA 1 , Bagaswoto HP2, Mumpuni H2, Maharani E3
1 Department of Cardiology and Vascular Medicine, Faculty of Medicine, Gadjah Mada University, Yogyakarta
2 Echocardiography Division, Department of Cardiology and Vascular Medicine, Faculty of Medicine, Gadjah Mada University, Yogyakarta
3 Arrhythmia Division, Department of Cardiology and Vascular Medicine, Faculty of Medicine, Gadjah Mada University, Yogyakarta
Background: Mitral P wave and negative deflection of P wave in electrocardiography (ECG) have been well-recognized as a marker for left atrial enlargement (LAE). Left atrial enlargement frequently occurs in patient with heart failure. Beside electrocardiography, left atrial enlargement can be measured by echocardiography with left atrial diameter measurement or left atrial volume index (LAVI) measurement. Left atrial diameter measurement has been done more often than LAVI measurement. This study aims to knowing which of these echocardiography measurement, Left atrial diameter or LAVI, are more predict left atrial enlargement in electrocardiography
Method: we performed crosssectional analytic study by analyzing ECG and echocardiography data from 110 subjects with chronic heart failure patients hospitalized at Sardjito General Hospital since April 2015. LAE in electrocardiography was marked by mitral P wave in lead II or negative deflection of P wave in lead V1. LAE in echocardiography was measured by left atrial volume index and LA diameter in parasternal long axis view.
Result: among the 110 subjects, 28 people have LeftAtrial Enlargement which measured by electrocardiography. Mean LAVI of all subjects was 41.36 ± 12.68 and mean LA diameter 38.26 ± 6.74 mm. logistic regression suggested that there is strong correlation between LA diameter and LAVI (R2 0.36 and P value < 0.001). Based on ROC curve analysis, obtained that LAE by ECG was correlated with LAVI > 44.5 (P 0.003) with sensitivity 46.67%, specificity 82.5%, positive predictive value 50%, negative predictive value 80.48% and accuracy 72.72%, meanwhile LAE by ECG was correlated with LA diameter > 40.5 mm (P 0.007) with sensitivity 40%, specificity 84.6%, positive predictive value 64.28%, negative predictive value 64.7% and accuracy 66.36%.
Conclusion: In our study, there is strong correlation between LA diameter and LAVI but both of these echocardiography measurement can not predict LAE in heart failure patient electrocardiography because of unsatisfactory sensitivity.
PP 41. Profile of WPW (Wolff-Parkinson-White) Syndrome and WPW Syndrome with Atrial Fibrillation in Electrophysiology Patients
Real Marsam 1 , Bagus H.Kuncahyo2, Dicky A. Hanafy3, Yoga Yuniadi3
1 Departement of Cardiology and Vascular Medicine, Faculty of Medicine Sebelas Maret University
2 Departement of Cardiology and Vascular Medicine, Faculty of Medicine
3 Brawijaya University 3 Departement of Cardiology and Vascular Medicine, Faculty of Medicine University of Indonesia
Background & Objectives: Atrial fibrillation (AF) is the second most frequent tachyarrhythmia in patient with Wolff Parkinson White (WPW) syndrome. Shortest pre-excited RR interval (SPERRI) has been known can predict outcomes of WPW in relation to AF, but other electrophysiology characteristics are rarely presented. In this study we sought to compare the electrophysiology characteristics of WPW patients with and without AF.
Methods: Fourty three WPW patients were consecutive selected among ablation patients within January 2013 until February 2014 at Arrhythmia Department of National Cardiovascular Center Harapan Kita Hospital. Data were analyzed using SPSS 15.
Result: Among 43 WPW syndrome patients there are 12 patients with AF. Clinical characteristic are not significantly difference between groups. PP interval in AF group is sugnificantly longer compare to non-AF group (764.25 ± 105.43 ms vs. 678.03 ± 155.78 ms, p = 0.046). In non-AF group, accessory pathway location is dominantly right posteroseptal (32.3%) while the AF group is dominantly has right anteroseptal accessoty pathway (25%). All patients in AF group suffered from orthrodromic atrioventricular reciprocating tachycardia (AVRT) in contrast to those in non-AF group who has 23% antidromic AVRT. The results of successfull radiofrequency ablation are 75% and 93.5.% in AF and non-AF groups respectively.
Conclusion: Interval of PP is longer in non-AF group and right anteroseptal accessory pathway is more dominant in AF group. Successful radiofrequency ablation is high among the groups.
Keyword: Wolff Parkinson White syndrome, atrial fibrillation, electrophysiology characteristics.
PP 42. Radio Frequency Ablation Therapy for Symptomatic Ventricular Extra Systole: Early Experience
Steven Rudy Utomo, Astri Astuti, Irlandi Suseno, Steven R Utomo, Doni Friadi, Muhammad Iqbal, Beny Hartono, Muhammad Munawar
Resident of Cardiology, Faculty of Medicine Sam Ratulangi University, Binawaluya Cardiac center
Background: Ventricular extra systole (VES) is commonly encountered in clinical practice. Usually it is not associated with life-threatening consequences in the absence of structural heart disease. However, frequent VES can be highly symptomatic and even incapacitating in some patients. This is our early experiensce of patients with VES, who has symptomatic VES, who underwent radiofrequency ablation therapy at our hospital.
Methods: All patients are having symptomatic VES who undergo radiofrequency ablation at our hospital is included. Echocardiography was performed in all patients. We use two methods of ablationc i.e. convensional and 3D electroanatomical mapping.
Results: During the period of January 2013 to September 2015, a total 47 patients were included in this study. There were 36 female (77%) and 11 male (23%) and their age was 53,51 ± 13,37 years (range 15 to 73). Ninety one percent have complaint frequent palpitation and 9% lightheadedness. Convensional mapping was performed in 36 patients (77%) and 3D electroanatomical mapping in 11 patients (23%). The origin of VES, mostly from anteroseptal RV and posteroseptal RV (17 (36%) and 18 (38%)). Other site were posterior free wall, LVOT RCC, LVOT LCC, mitral area and multi site (2%, 4%, 2%, 4% and 8%, respectively). No complication was found. All patients were successfully ablated. During three to six months follow up, there were 1 recurences (2%).
Conclusion: RF ablation therapy is alternative therapy for symptomatic VES. This modality seem to be effective and safe procedure.
PP 43. Radiofrequency Catheter Ablation for Atrial Fibrillation in Single Center Hospital, Jakarta: Short-term evaluation
Astri Astuti, Irlandi Suseno, Steven R Utomo, Doni Friadi, Muhammad Iqbal, Beny Hartono, Muhammad Munawar
Binawaluya Cardiac center
Background and Objectives: Atrial fibrillation (AF) is the most common arrhythmia found in clinical practice. It increases mortality and morbidity by increasing risk of stroke, heart failure, hospitalization, and also reducing quality of life. Patients whose refracter simptomatic or intolerant to antiaarrrhythmic medication have been indicated to undergo AF catheter ablation. It is also an initial treatment option in recurent symptomatic paroxysmal AF. The study is designed to describe characteristic of patients underwent AF ablation procedure, its diagnostic, therapetic process, and outcomes in our hospital.
Methods: This is a single centre, retrospective, and descriptive study. All patients are symptomatic AF, either paroxysmal or persistent. All are done for trans-esophageal echocardiography for detecting thrombus within left atrium. Either Carto 3D mapping or NavX system were used. Left atrial CT is also used for merging or combining CT and the 3D reconstruction of the left atrium. All underwent general anasthesia and were anticoagulated and the ACT was kept around 250. Post ablation all patients were given PPI intra-venously for 3 days.
Results: During period of January 2012 to August 2015, all patients were included. There were 68 patients included in the study and 85% of them was male. The mean age was 55.5 ± 10.8 years. Most of patients (90%) underwent first procedure. Paroxysmal AF was seen in 68% patients. Hypertension, the most demonstrated comorbid conditions, was noticed in 60% patients, followed by hyperlipidemia (49.3%), coronary artery disease (31%), diabetes melitus (14.9%), and congestive heart failure (11.9%). There was 23.5% lone AF patients. CHA2DS2VASc score 2 or more was seen in 38% patients. There was 10% ofpatients whom echocardiography features didn’t documented. Mean left atrial (LA) dimension from echocardiography was 38.6 ± 7.1 mm, with 34% had LA dilation. Pulmonary vein isolation was performed in all of the patients. The most ablated adjunctive substrate site was cavo tricuspid isthmus (38.8%), followed by complex fractionated atrial electrogram, left atrial roof line, and mitral isthmus line, respectively. Total terminated AF rate was 65%, while in paroxysmal AF was 80.4%, and only 31.8% in persistent AF. Total non terminated AF cases were consisting of 25% patients converted to sinus rhythm by cardioversion, 7% patients remained AF, and 3% of patients was canceled due to complication. Acute complication was occured in 6% of patients, of which 3% was tamponade, 1.5% was cardiac perforation, and 1.5% was bradycardia. There were no in hospital death following the procedure. At discharge, 90% of patients were in sinus rhythm. Anticoagulant were given in 46% of patients, of which 19% were given vitamin K antagonist and 27% were given novel oral anticoagulant. Oral antiarrhythmias (OAA) were given in 89.6% patients, which the most given OAA was amiodarone (67.2%). Recurrent AF patients who experienced left atrial appendage closure were 15.6% from all the procedures since 2012.
Conclusion: The RF AF ablation is safe procedure. The acute success rate of the procedure is quite high (90%) and therfore these modality maybe the procedure of choice of paroxysmal and persistent AF patients.
PP 44. Successfull Ablation of Atypical Left Anterior Wall Atrial Flutter
Dedie Setiadi 1 , Yosman Freedy S1, Dicky Armein Hanafy2, Yoga Yuniadi2
1 Resident of Cardiology and Vascular Medicine, Faculty of Medicine University of Diponegoro, Semarang
2 Department of Cardiology and Vascular Medicine, Faculty of Medicine University of Indonesia, Jakarta
Background: Typical right atrial flutter (AFL) has been extensively studied, but little data is available on the mapping of atypical left AFL. An anterior wall circuit of left AFL is an atypical AFL. Identification of this atypical AFL prior to the electrophysiology study is potentially useful because it allows appropriate procedural planning, success rates and risks of the procedure.
Case Report: We reported a 68-year-old male underwent three-dimensional (3D) mapping system using EnSite™ NavX™ Navigation & Visualization Technology by St. Jude Medical at National Cardiovascular Center Harapan Kita (NCCHK). Previously patient had three times ablation procedures for Atrial Fibrillation (AF) and mitral annulus left atypical AFL. He also had twice DC cardioversions history during symptomatic AFL. Risk factor of coronary artery disease (CAD) was hypertension and dyslipidemia. Preprocedural ECG revealed atypical left AFL with positive flutter waves in inferior and V6 leads, and negative flutter waves in lead aVL. An echocardiogram showed no LA thrombus with normal dimensions, ejection fraction, and valves. The 3D mapping was performed. Propagation of impuls showed zone of slow conduction at anterior wall of Left Atrium (LA) between two scar area, and clockwise activation pattern was appeared. Multiple Radiofrequency Ablation (RFA) was performed at this site. Ablation procedure of atypical left anterior wall AFL was successfull without any complication and ECG revealed Sinus Rhythm (SR).
Keywords: atypical left atrial flutter, anterior wall, the 3D mapping system, multiple radiofrequency ablation.
PP 45. Effect of Phase II Cardiac Rehabilitation on Improvement of Spatial QRS – T angle in Post Revascularization Patients
Giky Karwiky, Aninka Saboe, Badai Batara Tiksnadi, Chaerul Ahmad,
Sunaryo Sastradimaja, Augustine Purnomowati, Toni Mustahsani Aprami
Department of Cardiology and Vascular Medicine, Faculty of Medicine, Padjadjaran University, Bandung, Indonesia
Background and Objectives: Spatial QRS-T angle is an independent predictor of cardiovascular death in general population and patients with heart diseases. Benefit of cardiac rehabilitation has already proven in stable coronary artery disease (CAD) patient. To date, no studies have investigated the benefit of cardiac rehabilitation on ischemic burden in CAD patients assesed by spatial QRS-T angle. Aim of this study is to evaluate effect of phase II cardiac rehabilitation in spatial QRS-T angle in CAD patients that have undergone complete revascularization.
Methods: This was a prospective study conducted between September 2014 – May 2015. The inclusion criterias were patients that have undergone complete revascularization (PCI or CABG) that enter phase II cardiac rehabilitation. The exclusion criterias were patients with disabilities or having technical difficulties that can compromise the standard protocol exercise. Exercise prescription was determined based treadmill test that conducted in initial phase II cardiac rehabilitation, measured by treadmill or ergocycle with intensity of 50 - 80% heart rate reserved, 30 minutes each, two times a week, up to 12 supervised exercise completed in six to eight weeks. Functional capacities were also being evaluated at the end of phase II rehabilitation. All patients have 12-lead ECG recorded before and after phase II cardiac rehabilitation. Spatial QRS-T angle was measured by Kors visual transform applications. Statistical analysis were performed with paired sample T-test.
Results: Fourty-one patients were recruited consecutively and 4 patients were dropped out due to incomplete phase II cardiac rehabilitation. Baseline characteristics: median age: 56 years (Q1 = 37, Q3 = 73), 81% male, 52% post acute coronary syndrome patients, and 48% stable CAD patients. Complete revascularizations were achieved by CABG on 21.6% patients and PCI on 78.4% patients. All patients had significant improvement on functional capacity (mean: 1.86 ± 1.28 METs, p = 0.00). Seventy -eight percent patients had significant improvement in spatial QRS - T angle marked by decreased of spatial angle (mean 16.21 ± 19.99, p = 0.00). There were significant differences of QRS-T angle before and after procedure marked by mean spatial QRS-T angle pre-rehabilitation 76.73 ± 48.45 and mean spatial QRS-T angle post-rehabilitation 60.52 ± 42.81.
Conclusion: Phase II cardiac rehabilitation improves spatial QRS-T angle in CAD patient with complete revascularization.
PP 46. Atrial Fibrillation Registry in a Single Centre: Demographic and Clinical Characteristics
Angeline Nifiani M Wibowo 1 , K Marwali2, SA Yuwono1, D Hadi1, RW Putra1, Sunanto Ng1,2
1 Faculty of Medicine, Universitas Pelita Harapan
2 Siloam General Hospital, Tangerang, Indonesia
Background & Objective: Incidence ofatrial fibrillation is increasing; hence, the complication of atrial fibrillation is also increasing. The aim of this study is to describe the demographic and clinical characteristics of atrial fibrillation patients in a local secondary institution.
Methods: Study was designed as cross-sectional, consecutive from January to July 2015. We collected gender, age, body mass index, etiology, signs and symptoms, and outcome of the patients.
Results: Forty patients were included: female 22/55% with median age of 59 (min-max: 34-94) years old, and median BMI 21.96 (minmax: 13.33-29.76) kg/m2. The most common etiology of atrial fibrillation was hypertension (15/37.5%), followed by valvular (12/30%), heart failure (9/22.5%), cardiomyopathy (7/17.5%), coronary arterial disease (6/15%), and chronic renal failure (6/15%). Most patients were admitted with symptoms of dyspnea on exertion (23/57.5%); chest discomfort (15/37.5%); bloated (13/32.5%); decrease exercise tolerance (12/30%); paroxysmal nocturnal dyspnea (10/25%); orthopnea (10/25%); ischemic chest pain (7/17.5%); and palpitation (7/17.5%). Clinical findings on admission are presented as follows (median [min-max]): heart rate 125 (58-196) bpm, respiratory rate 25 (14-50)x/min, systolic blood pressure 130 (90-220) mmHg with diastolic blood pressure 87 (55-140) mmHg. The cardiothoracic ratio (CTR) was 65 (52-85) % and Left Ventricle Ejection Fraction was 50 (20-71) %. Outcome in our study were that death during hospitalization 5/12.5%, and stroke during hospitalization 1/2.5%
Conclusion: In our local secondary institution, the most common related finding was hypertensive arterial disease and the symptom was dyspnea on exertion.
PP 47. Correlation of Left Ventricular Ejection Fraction and Spatial QRS-T Angle in Post Revascularization Patients
Indy Mashfufah, Giky Karwiky, Chaerul Ahmad, Augustine Purnomowati, Toni Mustahsani Aprami
Department of Cardiology and Vascular Medicine, Padjadjaran University, Bandung
Background and Objectives: Spatial QRS-T angle, defined as the angle between the mean QRS and T vectors, is a strong independent predictor of incident coronary heart disease (CHD) and cardiovascular death. Recent study shows the spatial QRS-T angle calculations can be obtained from the ECG 12 lead with Kors visual transform applications closest to Frank lead system. The aim of this study was to evaluate the usefulness of spatial QRS-T in detecting cardiac dysfunction assessed with Left Ventricular Ejection Fraction (LVEF).
Methods: This was a crossectional study conducted between September - Desember 2014. The inclusion criterias were coronary artery disease (CAD) patients that have undergone complete revascularization (PCI or CABG). The exclusion criteria were patient with cardiac valve dysfunction, pulmonary heart disease, congenital heart disease, infectious endocarditis, pericardial disease, acute left cardiac dysfunction, arrhythmia and left or right complete bundle branch block (QRS duration > 120 ms). All patients have 12 -lead ECG recorded and echocardiography examination simultaneously after underwent coronary revascularization (PCI or CABG). Spatial QRS - T angle was measured by Kors visual transform applications. Statistical analyses were performed on the results using Spearman correlation and multivariate analysis with linear regression.
Results: Forty patients recruited consecutively and meet inclusion criteria. Baseline characteristics: mean age 56.38 ± 7 years, 80% male, 52.5% post acute coronary syndrome patients, and 47.5% stable CAD patients. Complete revascularization was achieved by CABG on 20% patients or PCI on 80% patients. Median spatial QRS-T was 62.74 ° (Q1 = 6.2, Q3 = 166.73), with mean LVEF 56.73 ± 11.741. The spatial QRS-T angle and LVEF was negative correlation (r = -0.747, p < 0.01). The Spatial QRS-T angle and LVEF of patients with coronary artery disease is negative correlation, the larger spatial QRS-T angle, the lower the LVEF. After adjusted with age, sex and LVH, QTc, reduction of LVEF is only independent predictor of wider spatial QRST angle.
Conclusion: The spatial QRS-T angle and LVEF of patients with coronary artery disease had negative correlation. Spatial QRS-T angle may be an easier index for assessing cardiac dysfunction in patients with coronary artery disease.
PP 48. Reversible Secondary Prolonged QT Interval and T Wave Alternans Caused by Hypoparathyroidism Induced Hypocalcemia
Asmoko Resta Permana, Dicky A. Hanafy, Dafsah A. Juzar, Daniel P.L Tobing, Irmalita
Division of Arrhythmia, Department of Cardiology and Vascular Medicine, University of Indonesia/National Cardiovascular Center Harapan Kita
Background: Prolonged QT interval may cause sudden death due to ventricular arrhythmias. Prolonged QT interval and T wave alternans caused by hypoparathyroidism induced hypocalcemia is a rare and potentially reversible condition.
Objectives: To present a rare case of a 52-year-old woman who developed prolonged QT interval and chronic heart failure associated with a hypoparathyroidism induced hypocalcemia after thyroidectomy. Case Illustration: A 52-year-old female presented with a history and physical findings for congestive heart failure. Electrocardiography showed sinus tachycardia, T wave alternans and prolonged QT interval without any Q waves or ST segment changes. In addition hypocalcemia and low level of parathyroid hormone were detected and coroangiography revealed normal coronary arteries. She developed cardiac arrest and CPR was done with immediate return of spontaneous circulation. Correction of hypocalcemia, treatment with diuretics, beta blocker and angiotensin converting enzyme inhibitor resulted in improvement of clinical symptoms and QT interval of the patient. A thorough history of the patient revealed thyroidectomy 10 years before.
Discussion: The acquired form of long QT Syndrome can be caused by severe hypocalcemia. Hypocalcemia itself may be induced by various condition including hypoparathyroidism. Our patient presented with classic features of congestive heart failure, prolonged QT interval and T wave alternans but without any clear history and evidence of ischemic or inflammatory etiology. A very thorough history taking, physical and laboratory examination are needed to help determine the cause of prolonged QT interval in this patient.
Summary: A female patient with prolonged QT interval, T wave alternans developed congestive heart failure and cardiac arrest associated with hypoparathyroidism induced hypocalcemia was adequately managed and showed improvement with pharmacological therapy.
Keywords: Long QT Syndrome, heart failure, hypocalcemia, hypoparathyroidism.
PP 49. Subclavian Balloon Venoplasty Procedure Facilitating Pacemaker Lead Implant in Patient with Chronic Total Occlusion (CTO) of Left Subclavian Vein
Angga Pramudita Pudianto 1 , Simon Salim2,Muhammad Yamin2
1 Cardiology Division, Departement of Internal Medicine, Faculty of Medicine, University of Indonesia
2 Staff Cardiology Division, Departement of Internal Medicine, Faculty of Medicine, University of Indonesia
Subclavian venous occlusion is an unexpected finding during pacemaker lead implant procedure as many patients are asymptomatic. This is due to the collaterals that have been frequently formed in chronic total occlusion. Current approaches recommend contralateral access and surgical intervention. Subclavian balloon venoplasty is an alternative to surgery and have been found to be safe and effective for subclavian venous occlusion.
We report a subclavian vein venoplasty proceeding a permanent pacemaker lead implantation performed in one procedure. A 76 year old woman prepared for permanent pacemaker lead implant procedure after an emergency temporary pacemaker had been implanted earlier due to symptomatic junctional bradycardia which after subsequent observation revealed to be a bradyarrhythmic episode of sick sinus syndrome. After performing venous cutdown and cannulation of the left cephalic vein we encounter an obstruction upon entering the subclavian vein hence our guidewire could not be advanced further beyond the left subclavian vein. Iodine contrast injection during venography imaging revealed a filling defect in proximal subclavian vein and contrast flow was rerouted to fill the collateral veins. The CTO was succesfully penetrated using the Terumo wire and then we performed venoplasty using REEF HP balloon 4.0 x 40 mm that was inflated to 10 - 20 atm for 10 to 20 seconds. Pacemaker implantation procedure was then completed without further dificulty and there were no complications afterwards.
PP 50. Reel Syndrome in an Obese Woman with Total Atrioventricular Block – A Case Report
Putri Septiani, Risalina Myrtha, Heru Sulastomo, M Triadhy Nugraha
Department of Cardiology and Vascular Medicine, Faculty of Medicine, Universitas Sebelas Maret
Background: Pacemaker implantation may cause undesirable complications. The complications include bleeding, infection, dislodgement, skin erosion, etc. Reel syndrome is one kind of lead retraction and dislodgement.
Case Illustration: A 31 years old obese postpartum woman came with shortness of breath for 3 days after delivering baby with caesarean section. She was referred to our hospital with the diagnosis of third degree atrioventricular block. The physical examination and chest radiography revealed bradycardia (50 beats/min), tachypnea and signs of congestion. The electrocardiogram (ECG) showed total atrioventricular block (TAVB) with P rate 110 bpm and QRS rate 50 bpm. A concentric left ventricular hypertrophy with ejection fraction 54% was found from echocardiography. After therapy, there was an improvement for the heart failure but the TAVB still persisted without any symptom. The patient got a permanent pacemaker (PPM) then. One month after the implantation, we found her ECG recording of TAVB again. The following chest radiography revealed the reeling and retraction of the lead around the generator. We diagnosed reel syndrome and we did lead repositioning.
Discussion: This case showed one of PPM implantation complications, a reel syndrome. Reel syndrome is a lead retraction and dislodgement because of generator rotation over its sagittal/ transversal axis, which causes lead reeling around the generator. The risk factors of this complication are female gender, large pocket, obesity, older people and dementia. This syndrome commonly occurs within a month of implantation and usually there is no damage of the lead. Reposition of the lead is the treatment, no need to change the lead.
Summary: Chest radiography is used to detect retraction and dislodgement of PPM lead, such as reel syndrome. In this syndrome, usually there is no damage of the lead, so the treatment is lead repositioning.
PP 51. Tachycardia Mediated Cardiomyopathy due to Atrioventricular Reentrant Tachycardia and Atrial Fibrillation: Serial Cases
Novi Ariyanti, Dicky A. Hanafy, Sunu Budhi Raharjo, Yoga Yuniadi
Division of Arrhythmia, Department of Cardiology and Vascular Medicine, University of Indonesia/National Cardiovascular Center Harapan Kita
Background: Tachycardia mediated cardiomyopathy (TMC) is a reversible form of dilated cardiomyopathy that can occur with most supraventricular and ventricular arrhythmias. It is usually seen in patients with no previous structural heart disease, it may be responsible for ventricular dysfunction aggravation in those with underlying heart disease. Tachycardia mediated cardiomyopathy remains poorly understood and is likely under-diagnosed.
Case Illustration: The first case, a 28 year old man with chief complaint palpitation came to emergency department of National Cardiovascular Center Harapan Kita (NCCHK). His electrocardiography (ECG) showed narrow QRS complex tachycardia suggesting SVT and there is delta wave during sinus rhytm, so we diagnosed as Wolff-Parkinson-White (WPW) syndrome. Echocardiography revealed dilated left ventricle (LV) with 33% ejection fraction (EF). Angiography showed non significant stenosis. Right anterior accessory pathway ablation was performed. During follow up, electrocardiography (ECG) showed disappearance of delta wave, normal PR interval and QRS duration and echocardiogram showed improvement LVEF. Second case, a 59 year old male came to the outpatient clinic NCCH with a chief complain of irregular palpitation since more than 1 year ago. ECG revealed atrial fibrillation with normal ventricular response. His coroangiogaphy showed normal coroner. Echocardiogram showed dilated left ventricle (LV) with 36% ejection fraction and dilated left atrium diameter. Three dimension AF ablation was done, rhythm converted to sinus rhythm. Follow up echocardiogram 3 months after ablation showed reduced end diastolic diameter (EDD), LA diameter and improvement function with ejection fraction of 50%. All patients were therapy with ACEi or ARB and betablocker. In AF patients was also given anticoagulant.
In summary, we reported serial cases of tachycardia mediated cardiomyopathy due to supravetntricular tachycardia WPW syndrome and atrial fibrillation. Tachycardia mediated cardiomyopathy is a reversible form of dilated cardiomyopathy. More commonly, the diagnosis is made after observing improvement in ventricular function following rate or rhythm control. It should be considered in all patients whose systolic dysfunction is diagnosed subsequent to or concomitant with atrial fibrillation or chronic tachyarrhythmia.
Keyword: Tachycardia mediated cardiomyopathy, WPW, Atrial fibrillation.
PP 52. Post Ablation Procedure in Patient with Type A WPW Whom Showing a Rapid Ventricular Rate of Atrial Fibrillation with Aberrancy
I Nyoman Indrawan Mataram, AA Istri Murwitha Prasanthi, I Wayan Wita
Departement of Cardiology and Vascular Medicine, Faculty of Medicine, Udayana University
Background: Wolff Parkinson White (WPW) Syndrome is a clinical entity characterized by preexcitation by presenting a bypass tract which is connects atriums directly to ventricles. The atrial impulse therefore is able to reach the ventricles not only through the AV node, but also through the bypass tract. This accessory pathway can cause premature activation of the ventricles. It can also serve as a pathway for reentry, which may result in clinical symptoms of paroxysmal tachycardia.
Case Illustration: Patient is male, 32 years old, an army member, complained about recurrent palpitation since 2 hours prior to admission. The same complaint occurred 5 months ago, which is patient has already diagnosed as WPW syndrome. On that time patient undergo the regular medical check up. Several work up diagnostic procedures has already done in this patient; echocardiography full study conclude that no abnormality in cardiac dimensions, normal LVEF (63%), PR mild, and global normokinetic. Treadmill stress test revealed that patient with N-1 functional capacity and negative for ischemia myocardial sign. Due to diagnostic work up and also occupational requirement, the patient has referred to Harapan Kita Hospital Jakarta to do an EP study and catheter ablation procedure; the results are normal SA and AV node function, WPW at right and left posteroseptal accessory pathway, partial successful ablation at right and left posteroseptal accessory pathway, no inducible AVRT, and non-sustained typical atrial flutter. On emergency unit, patient present with hemodynamically stable; BP 110/80 mmHg, HR 180 bpm, others examination were normal, and ECG clearly showing an irregular rhytm of AF RVR with aberrancy; patient was diagnosed an AF RVR with abberancy on WPW Syndrome. Amiodarone IV on continuous infusion rate was given with following doses: 150 mg in 10 minutes, 360 mg in 6 hours, and continued 540 mg in 18 hours. During observation, heart rate was gradually decreases until it convert into sinus rhytm with Type A WPW pattern and the complaint is also felt improved.
Case Discussion: WPW withAF is a specific concern and challenging because of the potential risk for progression into ventricular fibrillation due to rapidly anterograde accessory pathways. The risk of developing AF in 10 years in WPW patient is estimated 15%. The efficacy and safety of ablation procedure of accessory pathways does not prevent AF event completely, especially in an older age.
During AF, the ventricular rate is determined by competing conduction over the AV node and accessory pathways; AF with WPW with hemodynamically compromised still have an indication for cardioversion. In a stable patient, IV Ibutilide and Procainamide can be used, because those drugs did not available in our hospital, we used IV Amiodarone with its complex anti-arrhythmic activity, it lengthens the effective refractory period by prolonging action potential duration including bypass tract.
Conclusion: We reported a case of 52 years old male with WPW type A whom showing a AF RVR with abberant conduction.
PP 53. Clinical and Electrophysiology Characteristics of Outflow Tract and Fascicular Ventricular Tachycardia
Widyo mahargo, Sunu Budhi Raharjo, Dicky Armein Hanafy, Yoga Yuniadi
Division of Arrhythmia Department Cardiology and Vascular Medicine University of Indonesia; National Cardiovascular Center Harapan Kita Hospital
Background: Idopathic ventricular tachycardia (VT) or ventricular premature contraction (VPC) in patients with an anatomically normal heart is different from VT associated with structural heart disease. Two of the most frequent idiopathic VT/VPC were outflow tract VT and fascicular VT. The purpose of this study was to compare the characteristics of RVOT and ILVT at National Cardiovascular Center Harapan Kita Hospital Jakarta.
Methods: All patients with idiophatic VT who underwent radio frequency ablation (RFA) in 2012 were analyzed. Patients were clasified by type of VT; RVOT VT and ILVT.
Results: A total of 126 patients were included. Comparison sex distribution; male; 25 (19.8%) vs 27 (21.4%) p = 0.004 and age of the two kind idiopathic VT 43.81 ± 13.2 vs. 38.64 ± 15.3 years; p = 0.048, RVOT VT and ILVT respectively. Electrophysiology parameter (in ms) were compared and there were not significant difference; SCL (740.1 ± 163.8 vs. 998.6 ± 1228.6), AH (80.02 ± 17.1 vs. 119.3 ± 178.3), HV (50.2 ± 11.3 vs. 53.21 ± 11.0), antegrade AVN ERP (289.63 ± 88.3 vs. 301.42 ± 75.1), atrial ERP (244.80 ± 128.7 vs. 224.60 ± 32.1), Retrograde AVN ERP (278.12 ± 140.5 vs. 295.0 ± 90.0), except antegrade WP (339.09 ± 79.6 vs. 386.11 ± 68,7; p = 0.04).
Conclusions: We observed that ILVT occured more frequently in male and younger age.
PP 54. A Comparison of Atrial Tachycardia in Young Children and Adolescent: Electrophysiology Study
Isyana M Kurniawan 1,2 , Dicky A Hanafy1, Sunu B Rahardjo1, Yoga Yuniadi1
1 Department of Cardiology and Vascular Medicine, Faculty of Medicine Universitas Indonesia - National Cardiovascular Center Harapan Kita Hospital-Jakarta
2 Resident of Department of Cardiology and Vascular Medicine, Faculty of Medicine Universitas Sebelas Maret
Backgrounds: Atrial tachycardia (AT) typically occurs in adolescents and adults with limited data regarding AT in young Children
Methods: All patients with AT who underwent electrophysiology study and ablation between 2013-2014 were retrospectively studied. Patients were stratified by age < 15 years (young AT) or > 15 years (older AT). All measured values were reported as mean ± standard deviation (continues variables). Independent T test analysis was done for this study (p < 0.05 was considered as significant).
Results: A total of 36 patients were evaluated including 6 young AT patients (9.3 ± 3.1) and 30 older AT patients (42.4 ± 16.5 years). Electrophysiologic parameters showed that atrial effective refractory period were longer in young AT (250.00 ± 21.60 ms) than older AT (208.46 ± 32.36 ms) (p = 0,03). Other electrophysiologic parameters (SCL, AH interval, HV interval, wenckebach points, AV node effective refractory period, and ventricular effective refractory period) were similar in both groups.
Conclusion: Although electrophysiologic parameters in atrial tachycardia almost similar, but atrial effective refractory periode in young AT ( < 15 years) was longer than older AT ( > 15 years).
Keyword: Atrial tachycardia, atrial effective refractory period, electrophysiology study.
PP 55. Arrhythmogenic Right Ventricular Cardiomyopathy: A Unique Case with Specific Electrocardiographic and Voltage Map Findings
Ade Imasanti, Sunu B. Raharjo, Dicky A. Hanafy, Yoga Yuniadi
Division of Arrhythmia, Department of Cardiology and Vascular Medicine, University of Indonesia/ National Cardiovascular Center Harapan Kita
Background: Arrhythmogenic right ventricular cardiomyopathy (ARVC) is an inherited disorder characterized by progressive replacement of ventricular myocardium by fibrofatty tissue that predisposes patients to ventricular arrhythmias, heart failure and sudden death. Common arrhythmias in patients with ARVC include frequent premature ventricular complexes (PVCs), non-sustained ventricular tachycardia (VT) and sustained VT. Careful analysis of the electrocardiographic characteristics of the patient’s provide important clues to the diagnosis, while three dimensional (3D) mapping strategy allowed us to give better diagnostic and therapeutic option for the patients.
Case Illustration: A 55-year-old female with chief complain of palpitation and dizziness since 2 years before hospitalization. The patient had history of syncope in the previous hospitalization. Electrocardiography (ECG) finding showed sinus rhythm with complex monomorphic PVC’s with the LBBB morphology and superior axis, suggesting an RV apex origin. From the latest algorithm, we found this ECG finding was relevant with ECG characteristic in ARVC patient, i.e. the presence of anterior T-wave inversions (V1-V3) in sinus rhythm (3 points), lead I QRS duration of the VT/VPC of > 120 ms (2 points), QRS notching of the VT/VPC in multiple leads (2 points) and V5 transition or later (1 point). Therefore, in total the patient’s ECG has total points of 8 (a maximum points) which indicate a very high likelihood of ARVC. A 3D mapping and ablation using CARTO version 3.2 was then performed. Voltage mapping in the right ventricle area showed low voltage area in the basal free wall and mid to basal inferior of the RV which relevant with the ARVC substrate. Activation mapping of the VPC indicated the earliest activation area was in the mid inferior of the RV. Multiple radiofrequency ablation was delivered in this area and successfully eliminated the VPC. Post ablation, programmed electrical stimulation and isuprel administration could not induce any VPC/VT.
Keyword: Arrhythmogenic right ventricular cardiomyopathy, premature ventricular complexes, ECG characteristic, 3D mapping.
Author information
Authors and Affiliations
Consortia
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
ASEAN Federation of Cardiology. Abstracts of the 3rd Annual Scientific Meeting Indonesian Heart Rhythm Society, October 23 – 24, 2015. Asean Heart J 23, 4 (2015). https://doi.org/10.7603/s40602-015-0004-x
Published:
DOI: https://doi.org/10.7603/s40602-015-0004-x