Abstract
Background
The Oxford unicompartmental knee replacement (OUKR) has achieved excellent functional outcomes and long term survivorship in many single center and single surgeon series. However, in national registries, the failure rates are up to three times higher than total knee replacement. This is at least in part due to difficulty experienced by low-volume surgeons in implanting the prosthesis accurately. A new instrumentation system (Microplasty) was introduced to help surgeons achieve better component positioning, however, it is not known whether the new instruments achieve that goal. This study investigates whether the new system achieves better component positioning and whether it improves the clinical outcomes when compared to the existing instruments.
Materials and Methods
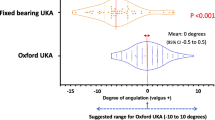
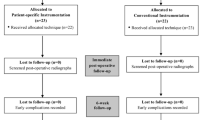
This retrospective cohort study compared 50 consecutive OUKR implanted using the conventional Phase 3 instrumentation with 100 consecutive OUKR implanted using the new Microplasty instrumentation. Component orientation was measured on postoperative radiographs, and the percentage outside the recommended range was identified. Intraoperative data and retrospectively collected clinical data were also analyzed.
Results
Femoral component alignment improved significantly, and there were no outliers in the Microplasty group. Although there were fewer tibial component alignment outliers with Microplasty, the difference was not significant. The intraoperative incidence of tibial recut, patient satisfaction and patient expectations was significantly better in the Microplasty group. The Oxford Knee Scores were also better with Microplasty, however, the difference was not significant.
Conclusion
Microplasty instrumentation helps the surgeon achieve optimal component positioning and reduces the need for tibial recut. The clinical outcomes are also better with the Microplasty instrumentation.
Similar content being viewed by others
References
Liddle AD, Judge A, Pandit H, Murray DW. Adverse outcomes after total and unicompartmental knee replacement in 101,330 matched patients: A study of data from the National Joint Registry for England and Wales. Lancet 2014;384:1437–45.
Liddle AD, Pandit H, Judge A, Murray DW. Patient-reported outcomes after total and unicompartmental knee arthroplasty: A study of 14,076 matched patients from the National Joint Registry for England and Wales. Bone Joint J 2015;97-B: 793–801.
Lisowski LA, van den Bekerom MP, Pilot P, van Dijk CN, Lisowski AE. Oxford phase 3 unicompartmental knee arthroplasty: Medium-term results of a minimally invasive surgical procedure. Knee Surg Sports Traumatol Arthrosc 2011;19:277–84.
Murray DW, Goodfellow JW, O’Connor JJ. The Oxford medial unicompartmental arthroplasty: A ten-year survival study. J Bone Joint Surg Br 1998;80:983–9.
Price AJ, Svard U. A second decade lifetable survival analysis of the Oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res 2011;469:174–9.
Rajasekhar C, Das S, Smith A. Unicompartmental knee arthroplasty 2- to 12-year results in a community hospital. J Bone Joint Surg Br 2004;86:983–5.
Svärd UC, Price AJ. Oxford medial unicompartmental knee arthroplasty. A survival analysis of an independent series. J Bone Joint Surg Br 2001;83:191–4.
Liddle AD, Pandit H, Judge A, Murray DW. Effect of surgical caseload on revision rate following total and unicompartmental knee replacement. J Bone Joint Surg Am 2016;98:1–8.
Fisher DA, Watts M, Davis KE. Implant position in knee surgery: A comparison of minimally invasive, open unicompartmental, and total knee arthroplasty. J Arthroplasty 2003;18:2–8.
Pandit H, Jenkins C, Barker K, Dodd CA, Murray DW. The Oxford medial unicompartmental knee replacement using a minimally-invasive approach. J Bone Joint Surg Br 2006;88:54–60.
Pandit H, Hamilton TW, Jenkins C, Mellon SJ, Dodd CA, Murray DW, et al. The clinical outcome of minimally invasive phase 3 Oxford unicompartmental knee arthroplasty: A 15-year followup of 1000 UKAs. Bone Joint J 2015;97-B:1493–500.
Price AJ, Webb J, Topf H, Dodd CA, Goodfellow JW, Murray DW, et al. Rapid recovery after Oxford unicompartmental arthroplasty through a short incision. J Arthroplasty 2001;16:970–6.
Shakespeare D, Ledger M, Kinzel V. Accuracy of implantation of components in the Oxford knee using the minimally invasive approach. Knee 2005;12:405–9.
Clarius M, Hauck C, Seeger JB, Pritsch M, Merle C, Aldinger PR, et al. Correlation of positioning and clinical results in Oxford UKA. Int Orthop 2010;34:1145–51.
Müller PE, Pellengahr C, Witt M, Kircher J, Refior HJ, Jansson V, et al. Influence of minimally invasive surgery on implant positioning and the functional outcome for medial unicompartmental knee arthroplasty. J Arthroplasty 2004;19:296–301.
Hurst JM, Berend KR. Mobile-bearing unicondylar knee arthroplasty: The Oxford experience. Clin Sports Med 2014;33:105–21.
Hurst JM, Berend KR, Adams JB, Lombardi AV Jr. Radiographic comparison of mobile-bearing partial knee single-peg versus twin-peg design. J Arthroplasty 2015;30:475–8.
Goodfellow J, O’Connor J, Pandit H, Dodd CA, Murray D. Unicompartmental Arthroplasty with the Oxford Knee. 2nd ed. Oxford: Goodfellow Publishers Limited, Oxford University Press; 2015.
Dawson J, Fitzpatrick R, Murray D, Carr A. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br 1998;80:63–9.
Murray DW, Fitzpatrick R, Rogers K, Pandit H, Beard DJ, Carr AJ, et al. The use of the Oxford hip and knee scores. J Bone Joint Surg Br 2007;89:1010–4.
Kalairajah Y, Azurza K, Hulme C, Molloy S, Drabu KJ. Health outcome measures in the evaluation of total hip arthroplasties – A comparison between the harris hip score and the Oxford hip score. J Arthroplasty 2005;20:1037–41.
Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the knee society clinical rating system. Clin Orthop Relat Res 1989;248:13–4.
Scuderi GR, Bourne RB, Noble PC, Benjamin JB, Lonner JH, Scott WN. The new knee society knee scoring system. Clinical Orthopaedics and Related Research® 2012;470:3–19.
Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 1985;198:43–9.
Mukherjee K, Pandit H, Dodd CA, Ostlere S, Murray DW. The Oxford unicompartmental knee arthroplasty: A radiological perspective. Clin Radiol 2008;63:1169–76.
Rees JL, Price AJ, Beard DJ, Robinson BJ, Murray DW. Defining the femoral axis on lateral knee fluoroscopy. Knee 2002;9:65–8.
Yoo JH, Chang CB, Shin KS, Seong SC, Kim TK. Anatomical references to assess the posterior tibial slope in total knee arthroplasty: A comparison of 5 anatomical axes. J Arthroplasty 2008;23:586–92.
Tu Y, Xue H, Ma T, Wen T, Yang T, Zhang H, et al. Superior femoral component alignment can be achieved with Oxford microplasty instrumentation after minimally invasive unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2017;25:729–35.
Koh IJ, Kim JH, Jang SW, Kim MS, Kim C, In Y, et al. Are the Oxford(®) medial unicompartmental knee arthroplasty new instruments reducing the bearing dislocation risk while improving components relationships? A case control study. Orthop Traumatol Surg Res 2016;102:183–7.
Gulati A, Chau R, Simpson DJ, Dodd CA, Gill HS, Murray DW, et al. Influence of component alignment on outcome for unicompartmental knee replacement. Knee 2009;16:196–9.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Malhotra, R., Kumar, V., Wahal, N. et al. New Instrumentation Improves Patient Satisfaction and Component Positioning for Mobile-Bearing Medial Unicompartmental Knee Replacement. JOIO 53, 289–296 (2019). https://doi.org/10.4103/ortho.IJOrtho_172_17
Published:
Issue Date:
DOI: https://doi.org/10.4103/ortho.IJOrtho_172_17