Abstract
Background
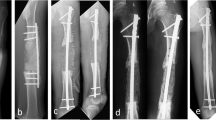
Open fractures are a difficult entity, often complicated by infection and nonunion. Bone loss in such fractures adds to the complexity. Conventional techniques of bone defect management are mainly directed toward fracture union but not against preventing infection or joint stiffness. In this case series, we evaluated Masquelet’s technique for management of open fractures with bone loss.
Materials and Methods
Twenty seven open fractures with bone defect, which presented within 3 days of trauma were planned for treatment by Masquelet’s technique. Followup ranged from 21 to 60 months.
Results
Average length of bone defect was 6 cm. Radiological union was obtained at a mean of 280 days since first stage of surgery. Time for union was not related to the size of defect. Union was faster in metaphyseal region (265.6 ± 38.8 days) as compared to diaphysis (300.9 ± 58.6 days). No patient had residual infection after stage 1. All the patients were able to mobilize with full weight bearing after radiological union with a satisfactory range of motion of adjacent joints.
Conclusion
This technique can be routinely applied in compound fractures with bone loss with good results. Chances of infection are reduced using antibiotic cement spacer as an adjunct to thorough debridement. Induced biomembrane revascularizes the graft. Union can be expected in most of the cases, however, long time to union is a limitation. Technique is cost-effective and does not require special training or instrumentation. Although it is a two-stage surgery, requirement of multiple surgeries, as may be needed in conventional methods, is avoided.
Similar content being viewed by others
References
Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: Retrospective and prospective analyses. J Bone Joint Surg Am 1976;58:453–8.
Gustilo RB, Gruninger RP, Davis T. Classification of type III (severe) open fractures relative to treatment and results. Orthopedics 1987;10:1781–8.
Zalavras CG, Marcus RE, Levin LS, Patzakis MJ. Management of open fractures and subsequent complications. J Bone Joint Surg Am 2007;89:884–95.
Cross WW 3rd, Swiontkowski MF. Treatment principles in the management of open fractures. Indian J Orthop 2008;42:377–86.
Paley D. Problems, obstacles, and complications of limb lengthening by the ilizarov technique. Clin Orthop Relat Res 1990;250:81–104.
Oostenbroek HJ, Brand R, van Roermund PM. Lower limb deformity due to failed trauma treatment corrected with the Ilizarov technique: Factors affecting the complication rate in 52 patients. Acta Orthop 2009;80:435–9.
Minami A, Kasashima T, Iwasaki N, Kato H, Kaneda K. Vascularised fibular grafts. An experience of 102 patients. J Bone Joint Surg Br 2000;82:1022–5.
Bumbasirevic M, Stevanovic M, Bumbasirevic V, Lesic A, Atkinson HD. Free vascularised fibular grafts in orthopaedics. Int Orthop 2014;38:1277–82.
Masquelet AC, Begue T. The concept of induced membrane for reconstruction of long bone defects. Orthop Clin North Am 2010;41:27–37.
DeCoster TA, Gehlert RJ, Mikola EA, Pirela-Cruz MA. Management of posttraumatic segmental bone defects. J Am Acad Orthop Surg 2004;12:28–38.
Anagnostakos K, Wilmes P, Schmitt E, Kelm J. Elution of gentamicin and vancomycin from polymethylmethacrylate beads and hip spacers in vivo. Acta Orthop 2009;80:193–7.
Chong KW, Woon CY, Wong MK. Induced membranes – A staged technique of bone-grafting for segmental bone loss: Surgical technique. J Bone Joint Surg Am 2011;93 Suppl 1:85–91.
Pelissier P, Masquelet AC, Bareille R, Pelissier SM, Amedee J. Induced membranes secrete growth factors including vascular and osteoinductive factors and could stimulate bone regeneration. J Orthop Res 2004;22:73–9.
Pelissier P, Martin D, Baudet J, Lepreux S, Masquelet AC. Behaviour of cancellous bone graft placed in induced membranes. Br J Plast Surg 2002;55:596–8.
Christou C, Oliver RA, Yu Y, Walsh WR. The masquelet technique for membrane induction and the healing of ovine critical sized segmental defects. PLoS One 2014;9:e114122.
Aho OM, Lehenkari P, Ristiniemi J, Lehtonen S, Risteli J, Leskelä HV, et al. The mechanism of action of induced membranes in bone repair. J Bone Joint Surg Am 2013;95:597–604.
Moris V, Loisel F, Cheval D, See LA, Tchurukdichian A, Pluvy I, et al. Functional and radiographic evaluation of the treatment of traumatic bone loss of the hand using the Masquelet technique. Hand Surg Rehabil 2016;35:114–21.
Flamans B, Pauchot J, Petite H, Blanchet N, Rochet S, Garbuio P, et al. Use of the induced membrane technique for the treatment of bone defects in the hand or wrist, in emergency. Chir Main 2010;29:307–14.
Apard T, Bigorre N, Cronier P, Duteille F, Bizot P, Massin P, et al. Two-stage reconstruction of posttraumatic segmental tibia bone loss with nailing. Orthop Traumatol Surg Res 2010;96:549–53.
Wang X, Luo F, Huang K, Xie Z. Induced membrane technique for the treatment of bone defects due to posttraumatic osteomyelitis. Bone Joint Res 2016;5:101–5.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kasha, S., Rathore, S.S. & Kumar, H. Antibiotic Cement Spacer and Induced Membrane Bone Grafting in Open Fractures with Bone Loss: A Case Series. JOIO 53, 237–245 (2019). https://doi.org/10.4103/ortho.IJOrtho_110_17
Published:
Issue Date:
DOI: https://doi.org/10.4103/ortho.IJOrtho_110_17