En
Abstract
Background
The diagnosis of central vestibular lesion is challenging and sometimes there is an overlap in symptoms and signs with a peripheral vestibular lesion. In some selected cases, dizziness is the only presenting symptom and in other patients, mild neurological symptoms as numbness are ignored. Videonystagmography (VNG) is considered a useful method for diagnosing vertigo of peripheral origin; however, not all the patients with central vertigo can be diagnosed easily. Benign paroxysmal positional vertigo and central positional vertigo share common criteria. The aim of the present study is to assess the usefulness of different VNG tests as predictors of central vestibular disorders, to determine the criteria that differentiate central positional nystagmus from the peripheral type, and to attempt to relate the abnormality in different VNG tests to certain central nervous system (CNS) levels.
Materials and methods
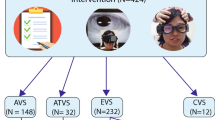
A retrospective study was carried out on 51 patients with possible central vestibular disorders from VNG tests battery and were referred for an MRI for further assessment. According to MRI results, the patients were divided into group A (31 patients), the group with manifest MRI findings, and group B, the group with free MRI (20 patients). Different VNG tests were compared between both groups.
Results
Three predictors of CNS lesion by VNG were determined: fixation index (FI), oculomotor tests, and central positional nystagmus; there was a statistically significant difference between both groups in FI, oculomotor tests, and central positional nystagmus, and apogeotropic criteria or nystagmus in multiple plains. There was no relation between any of those predictors and specific levels in the CNS.
Conclusion
VNG tests are a good diagnostic tool to differentiate between peripheral and central vestibular lesions. The inclusion of FI and positional tests to the oculomotor tests increases the sensitivity of the VNG. In some cases, it is difficult to distinguish between benign paroxysmal positional vertigo and central positional vertigo; apogeotropic nystagmus and nystagmus in multiple plains should raise the suspicion of CNS lesion. Anterior circulation ischemia may lead to chronic vertigo symptoms. Central vestibular vertigo could be caused by dysfunction or excitation of various structures in the CNS including the vestibular cortex.
Article PDF
Similar content being viewed by others
References
Mehmet Karatas. Central vertigo and dizziness: epidemiology, differential diagnosis, and common causes. Neurologist 2008;14:355–364.
Baloh RW, Honrubia V. Clinical neurophysiology of the vestibular system. Philadelphia, PA: F.A. Davis; 1979. 44–73
Hain T. Vestibular function − making the right interpretation with the right test. Hear J 2011; 64: 26–30.
Shiomi Y, Shiomi Y, Oda N, Fujihara M. Impaired visual suppression of manually rotated vestibuloocular reflex indicates the need of further evaluation by MRI and MRA in patients with vertigo. Otolaryngol Head Neck Surg 2004; 131: 930–933.
Silvoniemi P, Laurikainen E, Johansson R, KarjalainenS Electronystagmographic findings in patients with acute cerebral vascular disease and vertigo. Acta Otolaryngol Suppl 2000; 543: 41–43.
Hathiram BT, Khattar VS. Videonystagmography. Int J Otorhinolaryngol Clin 2012; 4: 17–24.
Buttner U, Helmchen C, Brandt T. Diagnostic criteria for central versus peripheral positioning nystagmus and vertigo: a review. Acta Otolaryngol 1999; 119: 1–5.
Neuhauser HK, Lempert T. Diagnostic criteria for migrainous vertigo. Acta Otolaryngol 2005; 125: 1247–1248.
Silman S, Silverman CA. Electronystagmography. In:. Silman S, Silverman CA editor. Auditory diagnosis principles and applications. San Diego, CA: Academic Press; 1991. 298–331.
Eggers SD, Zee DS. Evaluating the dizzy patient: bedside examination and laboratory assessment of the vestibular system. Semin Neurol 2003; 23: 47–58.
Cogan DG. Dissociated nystagmus with lesions in the posterior fossa. Arch Ophthalmol 1963; 70: 361–368.
Califano L, Capparuccia PG, Bojano A, Di Maria D, Villari G. Vertical nystagmus induced by the head-shaking test: 10 cases. Acta Otorhinolaryngol Ital 1999;19:297–302.
Choi JY, Kim JH, Kim HJ, Glasauer S, Kim JS. Central paroxysmal positional nystagmus: characteristics and possible mechanisms. Neurology 2015; 84: 2238–2246.
De Stefano A, Kulamarva G, Dispenza F. Malignant paroxysmal positional vertigo. Auris Nasus Larynx 2012; 39: 378–382.
Hotson JR, Baloh RW. Acute vestibular syndrome. N Engl J Med 1998; 339: 680–685.
Edlow JA, Newman-Toker DE, Savitz SI. Diagnosis and initial management of cerebellar infarction. Lancet Neurol 2008; 7: 951–964.
Rosenberg ML, Gizzi M. Neuro-otologic history. Otolaryngol Clin North Am 2000; 33: 471–482.
Derebery MJ. The diagnosis and treatment of dizziness. Med Clin North Am 1999; 83: 163–177.
Kattah JC, Talkad AV, Wang DZ, HsiehYH Newman-TokerDE HINTS to diagnose stroke in the acute vestibular syndrome: three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Stroke 2009; 40: 3504–3510.
Lee H, Kim JS, Chung EJ, Yi HA, Chung IS, Lee SR, Shin JY Infarction in the territory of anterior inferior cerebellar artery: spectrum of audiovestibular loss. Stroke 2009; 40: 3745–3751.
Newman-Toker DE, Reich SG. Wrong-way nystagmus in the AICA syndrome [letter]. Laryngoscope 2008; 118: 378–379.
Lalkhen AG, McCluskey A. Clinical tests: sensitivity and specificity. Contin Educ Anaesth Crit Care Pain 2008; 8: 221–223.
Murai N, Naito Y, Funabiki K, kato N, Ito J Visual suppression testing during manual sinusoidal rotation. Equilibrium Res 2001; 60: 234–240.
Fukushima K. Corticovestibular interactions: anatomy, electrophysiology, and functional considerations. Exp Brain Res 1997; 117: 1–16.
Leigh RJ, Zee DS. The neurology of eye movements. New York, NY: Oxford University Press 2006.
Hain TC. Background and technique of ocular motility testing. In: Jacobson GP, Newman CW, Kartush JM editors. Hand book of balance function testing. St Louis, MO: Mosby Year book; 1993;83–100.
Lechner C, Taylor RL, Todd C, Macdougall H, Yavor R, Halmagyi GM, Welgampola MS Causes and characteristics of horizontal positional nystagmus. J Neurol 2014; 261: 1009–1017.
Williams LG, Brimage P, Lechner C, Taylor RL, Masters L, Welgampola MS. Lhermitte-Duclos disease presenting with atypical positional nystagmus. J Clin Neurosci 2014; 21: 1647–1649.
Nam J, Kim S, Huh Y, Kim JS. Ageotropic central positional nystagmus in nodular infarction. Neurology 2009;73:1163.
Kim HA, Yi HA, Lee H. Apogeotropic central positional nystagmus as a sole sign of nodular infarction. Neurol Sci 2012; 33: 1189–1191.
Dieterich M, Brandt T. Why acute unilateral vestibular cortex lesions mostly manifest without vertigo. Neurology 2015; 84: 1680–1684.
Author information
Authors and Affiliations
Corresponding author
Additional information
Conflicts of interest
There are no conflicts of interest.
Rights and permissions
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work noncommercially, as long as the author is credited and the new creations are licensed under the identical terms.
To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mohamed, E.S. Predictors of central vestibular disorders from videonystagmography tests. Egypt J Otolaryngol 32, 202–209 (2016). https://doi.org/10.4103/1012-5574.186534
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.4103/1012-5574.186534