Abstract
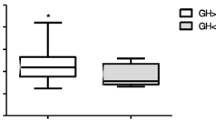
Background: Our aim was to retrospectively evaluate the possibility to reduce the number of GH analyses during clonidine and glucagon tests without compromising accuracy. Subjects and methods: Two hundred and forty-five tests were performed in a total of 188 children and adolescents with a mean age of 9.93±2.88 yr in a single center during the last 5 yr. Results: Ninety-one out of 158 (57.59%) clonidine tests and 47/87 (54.02%) glucagon tests had at least one sample >10 µg/l (negative). For clonidine tests, not measuring GH at 30 min would have resulted in only one negative test missed (0.63% false positive result), whereas not measuring GH both at 0 and 30 min would have increased the false positive percentage to 2.53%. Ending clonidine tests at 90 min would have resulted in 7 negative tests missed (4.43% false positive results). For glucagon tests, more than half of the tests peaked at 120 min (56.32%). Skipping sampling at 0, 60 and 180 min provided a false positive rate of 5.75%. Conclusions: For clonidine tests we can omit blood sampling at time points 0 and 30 min without significantly compromising accuracy.
Similar content being viewed by others
References
Richmond EJ, Rogol AD. Growth hormone deficiency in children. Pituitary 2008, 11: 115–20.
Growth Hormone Research Society. Consensus guidelines for the diagnosis and treatment of growth hormone (GH) deficiency in childhood and adolescence: summary statement of the GH Research Society. GH Research Society. J Clin Endocrinol Metab 2000, 85: 3990–3.
Badaru A, Wilson DM. Alternatives to growth hormone stimulation testing in children. Trends Endocrinol Metab 2004, 15: 252–8.
Gandrud LM, Wilson DM. Is growth hormone stimulation testing in children still appropriate? Growth Horm IGF Res 2004, 14: 185–94.
Sizonenko PC, Clayton PE, Cohen P, Hintz RL, Tanaka T, Laron Z. Diagnosis and management of growth hormone deficiency in childhood and adolescence. Part 1: diagnosis of growth hormone deficiency. Growth Horm IGF Res 2001, 11: 137–65.
Stanley T. Diagnosis of growth hormone deficiency in childhood. Curr Opin Endocrinol Diabetes Obes 2012, 19: 47–52.
Morris AH, Harrington MH, Churchill DL, Olshan JS. Growth hormone stimulation testing with oral clonidine: 90 minutes is the preferred duration for the assessment of growth hormone reserve. J Pediatr Endocrinol Metab 200, 14: 1657–60.
Galluzzi F, Stagi S, Parpagnoli M, et al. Oral clonidine provocative test in the diagnosis of growth hormone deficiency in childhood: should we make the timing uniform?. Horm Res 2006, 66: 285–8.
Muster L, Zangen DH, Nesher R, Hirsch HJ, Muster Z, Gillis D. Arginine and clonidine stimulation tests for growth hormone deficiency revisited—do we really need so many samples?. J Pediatr Endocrinol Metab 2009, 22: 215–23.
Strich D, Terespolsky N, Gillis D. Glucagon stimulation test for childhood growth hormone deficiency: timing of the peak is important. J Pediatr 2009, 154: 415–9.
Silva EG, Slhessarenko N, Arnhold IJ, et al. GH values after clonidine stimulation measured by immunofluorometric assay in normal prepubertal children and GH-deficient patients. Horm Res 2003, 59: 229–33.
Batista MC, Arnhold IJ, Mendonca BB, D’Abronzo FH, Bloise W, Nicolau W. Low-dose oral clonidine: effective growth hormone releasing agent in children but not in adolescents. J Pediatr 1987, 111: 564–7.
Stanley TL, Levitsky LL, Grinspoon SK, Misra M. Effect of body mass index on peak growth hormone response to provocative testing in children with short stature. J Clin Endocrinol Metab 2009, 94: 4875–81.
Loche S, Guzzetti C, Pilia S, et al. Effect of body mass index on the growth hormone response to clonidine stimulation testing in children with short stature. Clin Endocrinol (Oxf) 2011, 74: 726–31.
Secco A, di Iorgi N, Napoli F, et al. The glucagon test in the diagnosis of growth hormone deficiency in children with short stature younger than 6 years. J Clin Endocrinol Metab 2009, 94: 4251–7.
Chanoine JP, Rebuffat E, Kahn A, Bergmann P, Van Vliet G. Glucose, growth hormone, cortisol, and insulin responses to glucagon injection in normal infants, aged 0.5–12 months. J Clin Endocrinol Metab 1995, 80: 3032–5.
Johnstone HC, Cheetham TD. GH and cortisol response to glucagon administration in short children. Horm Res 2004, 62: 27–32.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Christoforidis, A., Triantafyllou, P., Slavakis, A. et al. Clonidine and glucagon stimulation for testing growth hormone secretion in children and adolescents: Can we make it with fewer samples?. J Endocrinol Invest 36, 1046–1050 (2013). https://doi.org/10.3275/9061
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.3275/9061