Abstract
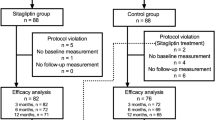
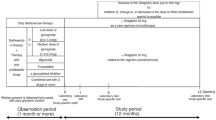
Background: Few studies have investigated the factors related to improvement and maintenance of glycemic control with sitagliptin in Type 2 diabetes (T2D) patients. Aim: To identify factors contributing to reaching and maintaining glycated hemoglobin (HbA1c) <7% with sitagliptin in Japanese T2D patients. Subjects and methods: This study included 1327 patients who were: taking sitagliptin as monotherapy; switched to sitagliptin; or taking sitagliptin in combination therapy. At baseline and 1, 3, 6, and 12 months after starting sitagliptin, weight, body mass index (BMI), HbA1c, fasting plasma glucose (FPG), and post-prandial plasma glucose (PPG) were measured. The subjects were divided into a group that achieved HbA1c<7% at 12 months, a poor control group(HbA1c≥8% at 12 months), and a discontinued group. Multiple regression analysis was performed to identify factors contributing to long-term control and maintenance with sitagliptin treatment. Results: HbA1c decreased significantly from 8.0% at baseline to 7.3%, but weight was unchanged. FPG and PPG improved significantly. The HbA1c<7% group had a significantly higher age and a significantly lower BMI at baseline than the HbA1c≥8% group and the discontinued group. On multivariate regression analysis, baseline HbA1c, baseline BMI, and Δbody weight after 12 months were significantly related to HbA1c reduction. The most common adverse event was hypoglycemia, and the most common adverse event responsible for discontinuation was constipation. Conclusions: HbA1c<7.0% was achieved in 31 % of T2D patients who had poor control with conventional treatment. Weight management is important for maintaining good long-term control with sitagliptin.
Similar content being viewed by others
References
Iwamoto Y, Tajima N, Kadowaki T, et al. Efficacy and safety of sitagliptin monotherapy compared with voglibose in Japanese patients with type 2 diabetes mellitus: a randomized double-blind trial. Diabetes Obes Metab 2010, 12: 613–22.
Nonaka K, Kakikawa T, Sato A, et al. Efficacy and safety of sitagliptin monotherapy in Japanese patients with type 2 diabetes. Diabetes Res Clin Pract 2008, 79: 291–8.
Tajima N, Kadowaki T, Odawara M, et al. Addition of sitagliptin to ongoing glimepiride therapy in Japanese patients with type 2 diabetes over 52 weeks leads to improved glycemic control. Diabetol Int 2011, 2: 32–44.
Drucker DJ, Nauck MA. GLP-1R agonists (incretin mimetics) and DPP-4 inhibitors (incretin enhancers) for the treatment of type 2 diabetes. Lancet 2006, 368: 1696–705.
Elrick H, Stimmler L, Hland CJ jr, Arai Y. Plasma insulin response to oral and intravenous glucose administration. J Clin Endocrinol Metab 1964, 24: 1076–82.
McIntyre N, Holdsworth CD, Turner DS. Intestinal factors in the control of insulin secretion. J Clin Endocrinol Metab 1965, 25: 1317–24.
Maeda H, Kubota A, Tanaka Y, Terauchi Y, Matsuba I; ASSET-K Study group. The safety, efficacy and predictors for HbA1c reduction of sitagliptin in the treatment of Japanese type 2 diabetes. Diabetes Res Clin Pract 2012, 95: e20–2.
Kubota A, Maeda H, Kanamori A, et al. Efficacy and safety of sitagliptin monotherapy and combination therapy in Japanese type 2 diabetes patients. J Diabetes Invest (in press).
Kubota A, Maeda H, Kanamori A, et al. Pleotropic effects of sitagliptin in the treatment of type 2 diabetes mellitus patients. J Clin Med Res 2012, 4: e309–13.
Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of Hyperglycemia in Type 2 Diabetes: A Patient-Centered Approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2012, 35: 1364–79.
American Diabetes Association. Standard of medical care in diabetes-2011. Diabetes Care 2011, 34(Suppl. 1): S11–61.
Esposito K, Cozzolino D, Bellastella G, et al. Dipeptidyl peptidase-4 inhibitors and HbA1c target of <7% in type 2 diabetes: meta-analysis of randomized controlled trials. Diabetes Obes Metab 2011, 13: 594–603.
Tajiri Y, Munehisa T, Ohki T, et al. Long-term efficacy of sitagliptin for the treatment of type 2 diabetic patients in Japan. Endocr J 2012, 59: e197–204.
Yoshinaga H, Kosaka K. Heterogeneous relationship of early insulin response and fasting insulin level with development of noninsulin-dependent diabetes mellitus in non-diabetic Japanese subjects with or without obesity. Diabetes Res Clin Pract 1999, 44: 129–36.
Arai K, Matoba K, Hirao K, et al. Present status of sulfonylurea treatment for type 2 diabetes in Japan: second report of a cross-sectional survey of 15, 652 patients. Endocr J 2010, 57: 499–507.
Iwasaki M, Hoshian F, Tsuji T, et al. Predicting efficacy of dipeptidyl peptidase-4 inhibitors in patients with type 2 diabetes: Association of glycated hemoglobin reduction with serum eicosapentaenoic acid and docosahexaenoic acid levels. J Diabetes Invest 2012, 3: 464–7.
Menotti A, Kromhout D, Blackburn H, et al. Food intake patterns and 25-year mortality from coronary heart disease: cross-cultural correlations in the Seven Countries Study. The Seven Countries Study Research Group. Eur J Epidemiol 1999, 15: 507–15.
Muscelli E, Mari A, Casolaro A, et al. Separate impact of obesity and glucose tolerance on the incretin effect in normal subject and type 2 diabetic patients. Diabetes 2008, 57: 1340–8.
Vollmer K, Holst JJ, Baller B, et al. Predictors of incretin concentrations in subjects with normal, impaired, and diabetic glucose tolerance. Diabetes 2008, 57: 678–87.
Nauck MA, Vardarli I, Deacon CF, Holst JJ, Meier JJ. Secretion of glucagon-like peptide-1 (GLP-1) in type 2 diabetes: what is up, what is down? Diabetologia 2011, 54: 10–8.
Højberg PV, Vilsbøll T, Rabøl R, et al. Four weeks of near-normalisation of blood glucose improves the insulin response to glucagon-like peptide-1 and glucose-dependent insulinotropic polypeptide in patients with type 2 diabetes. Diabetologia 2009, 52: 199–20.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Maeda, H., Kubota, A., Kanamori, A. et al. Long-term efficacy and safety of sitagliptin in the treatment of Japanese Type 2 diabetes (ASSET-K1) to a target of HbA1c<7%. J Endocrinol Invest 36, 568–573 (2013). https://doi.org/10.3275/8819
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.3275/8819