Abstract
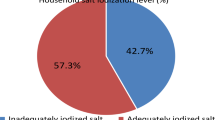
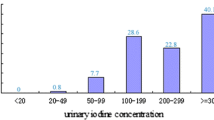
Background: Iran has long been recognized as a country of iodine sufficiency; however, recent studies show that the proportion of subjects with insufficient urinary iodine is gradually increasing in Tehran capital city. Aim: The aim of this study was to evaluate differences between individuals with sufficient and deficient urinary iodine in Tehran. Material and methods: In this cross-sectional study, 639 Tehranian adult subjects, aged ≥19 yr (242 males, 397 females), were enroled through randomized cluster sampling. A 24-h urine sample was collected for measurement of urinary iodine, sodium and creatinine concentrations using the digestion method, flame photometry and autoanalizer assay, respectively. Salt intake was estimated and iodine content of household salt was measured by titration. Results: Medians (interquartile range) of 24-h urinary iodine concentrations in subjects with sufficient and deficient urinary iodine were 163.0 (126.0–235.0) and 44.0 (26.0–67.0) µg/l, p<0.001, respectively. Salt with iodine content of >20 parts per million was consumed by 77.4 and 38.3% of subjects with sufficient and deficient urinary iodine, respectively (p<0.001). Median daily salt intake in subjects with sufficient urinary iodine was significantly higher than in those with deficient urinary iodine (8.1 vs 7.3 g, p<0.001). No significant differences in the mentioned variables were observed between males and females. Fifty and 30% of subjects with insufficient and sufficient urinary iodine had <7 yr education, respectively (p<0.001). Conclusions: Iodine content of salt, the amount of salt intake and education levels differ greatly between subjects with sufficient and deficient urinary iodine in Tehran.
Similar content being viewed by others
References
Andersson M, Takkouche B, Egli I, Allen HE, de Benoist B. Current global iodine status and progress over the last decade towards the elimination of iodine deficiency. Bull World Health Organ 2005, 83: 518–25.
Jooste PL, Zimmermann MB. Progress towards eliminating iodine deficiency in South Africa. S Afr J Clin Nutr 2008, 21: 8–14.
WHO, UNICEF, ICCIDD. Assessment of iodine deficiency disorders and monitoring their elimination. A guide for programme managers. 3rd ed. Geneva: WHO, 2007.
World Health Organization. Iodine deficiency in Europe: A continuing public health problem. Geneva: WHO. 2007.
Emami A, Shahbazi H, Sabzevari M, et al. Goiter in Iran. Am J Clin Nutr 1969, 22: 1584–8.
Azizi F, Kimiagar M, Nafarabadi M, Yassai M. Current status of iodine deficiency in Islamic Republic of Iran. EMR Health Serv J 1990, 8: 23–7.
Azizi F, Sheikholeslam R, Hedayati M, et al. Sustainable control of iodine deficiency in Iran: beneficial results of the implementation of the mandatory law on salt iodization. J Endocrinol Invest 2002, 25: 409–13.
Azizi F, Mehran L, Sheikholeslam R, et al. Sustainability of a wellmonitored salt iodization program in Iran: marked reduction in goiter prevalence and eventual normalization of urinary iodine concentrations without alteration in iodine content of salt. J Endocrinol Invest 2008, 31: 422–31.
Nazeri P, Mirmiran P, Mehrabi Y, Hedayati M, Delshad H, Azizi F. Evaluation of iodine nutritional status in Tehran, Iran: Iodine deficiency within iodine sufficiency. Thyroid 2010, 20: 1399–406.
Dunn JT. Complacency: the most dangerous enemy in the war against iodine deficiency. Thyroid 2000, 10: 681–3.
Intersalt Cooperative Research Group. Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour sodium and potassium excretion. BMJ 1988, 297: 319–28.
Stamler J. The INTERSALT Study: background, methods, findings, and implications. Am J Clin Nutr 1997, 65 (Suppl): S626–42.
Stamler J, Elliot P, Dennis B, et al. for INTERMAP Research Group. INTERMAP: background, aims, design, methods, and descriptive statistics (nondietary). J Hum Hypertens 2003, 17: 591–608.
De Maeyer EM, Lowenstein FW, Thilly CH. The control of endemic goiter. Geneva: World Health Organization. 1979. Available at http://Hatnim.co.kr/new/data/titration.pdf (accessed December 2009).
Sandell EB, Koltoff IM. Micro determination of iodine by a catalytic method. Mikrochemica Acta 1937, 1: 9–25.
Rego-Iraeta A, Pérez-Fdez R, Cadarso-Suárez C, et al. Iodine nutrition in the adult population of Galicia (Spain). Thyroid 2007, 17: 161–7.
Zimmermann MB, Wegmuller R, Zeder C, Torresani T, Chaouki N. Rapid relapse of thyroid dysfunction and goiter in school-age children after discontinuation of salt iodization. Am J Clin Nutr 2004, 79: 642–5.
Dunn JT. What’s happening to our iodine? J Clin Endocrinol Metab 1998, 83: 3398–400.
Zimmermann MB. Assessing iodine status and monitoring progress of iodized salt programs. Am J Clin Nutr 2004, 134: 1673–7.
Markou KB, Georgopoulos NA, Makri M, et al. Iodine deficiency in Azerbaijan after the discontinuation an iodine prophylaxis program: reassessment of iodine intake and goiter prevalence in schoolchildren. Thyroid 2001, 11: 1141–6.
Dasgupta P K, Liu Y, Dyke A. Iodine nutrition: Iodine content of iodized salt in the United State. Environ Sci Technol 2008, 42: 1315–23.
Rana R. Iodine losses from iodized salt during different cooking methods. Proceeding of the 14th International Thyroid Congress, Paris, France, September 11–16, 2010.
Stimec M, Kobe H, Smole K, et al. Adequate iodine intake of Slovenian adolescents is primarily attributed to excess salt intake. Nutr Res 2009, 29: 888–96.
World Health Organization. Reducing salt intake in populations. Report of WHO forum and technical meeting. Paris, France, October 5–7, 2006; Geneva, Switzerland, 2007. Available at www.who.int/dietphysicalactivity/Salt_Report_VC_april07.pdf (accessed December, 2009).
Mustafa A, Muslimatun S, Untoro J, Lan MC, Kristianto Y. Determination of discretionary salt intake in a iodine deficient area of East Java Indonesia using three different methods. Asia Pac J Clin Nutr 2006, 15: 362–7.
Melse-Boonstra A, Rozendaal M, Rexwinkel H, et al. Determination of discretionary salt intake in rural Guatemala and Benin to determine the iodine fortification of salt required to control iodine deficiency disorders: studies using lithium-labeled salt. Am J Clin Nutr 1998, 68: 636–41.
Temple V, Mapira P, Adeniyi K, Sims P. Iodine deficiency in Papua New Guinea (sub-clinical iodine deficiency and salt iodization in the highlands of Papua New Guinea). J Public Health 2005, 27: 45–8.
Amoa B, Pikire T, Tine P. Iodine content of salt in Lae city of Papua New Guinea. Asia Pac J Clin Nutr 1998, 7: 128–30.
Rafiei M, Boshtam M, Sarraf-Zadegan N, Seirafian S. The relation between salt intake and blood pressure among Iranian. Kuwait Med J 2008, 40: 191–5 (abstract).
Rahmani M, Koohkan A, Allahverdian S, Hedayati M, Azizi F. Comparison of dietary iodine intake and urinary excretion in urban and rural households of Ilam in 2000. Iranian Journal of Endocrinology and Metabolism 2000, 1: 31–7 (in Farsi).
Tayie FA, Jourdan K. Hypertension, dietary salt restriction, and Iodine Deficiency among Adults. Am J Hypertens 2010, 23: 1095–102.
Azizi F, Ghanbarian A, Momenan AA, et al; Tehran Lipid and Glucose Study Group. Prevention of non-communicable disease in a population in nutrition transition: Tehran Lipid and Glucose Study phase II. Trials 2009, 10: 5.
Jooste PL, Upson N, Charlton KE. Knowledge of iodine nutrition in the South African adult population. Public Health Nutr 2005, 8: 382–6.
Bulliyya G, Dwibedi B, Mallick G, Sethy PG, Kar Sk. Determination of iodine nutrition and community knowledge regarding iodine deficiency disorders in selected tribal blocks of Orissa, India. J Pediatr Endocrinol Metab 2008, 21: 79–87.
Mohapatra SS, Bulliyya G, Kerketta AS, Geddam JJ, Acharya AS. Elimination of iodine deficiency disorders by 2000 and its bearing on the people in a district of Orissa, India: a knowledge-attitude-practice study. Asia Pac J Clin Nutr 2001, 10: 58–62.
Abuye C, Berhane Y. The goiter rate, its association with reproductive failure, and the knowledge of iodine deficiency disorders (IDD) among women in Ethiopia: cross-section community based study. BMC Public Health 2007, 7: 316.
Charlton KE, Yeatman HR, Houweling F. Poor iodine status and knowledge related to iodine on the eve of mandatory iodine fortification in Australia. Asia Pac J Nutr 2010, 19: 250–5.
Charlton KE, Gemming L, Yeatman H, Ma G. Suboptimal iodine status of Australian pregnant women reflects poor knowledge and practices related to iodine nutrition. Nutrition 2010, 26: 963–8.
Vejbjerg P, Knudsen N, Perrild H, et al. Estimation of iodine intake from various urinary iodine measurements in population studies. Thyroid 2009, 19: 1281–6.
Knudsen N, Bulow I, Jorgensen T, Perrild H, Ovesen L, Laurberg P. Serum Tg- a sensitive marker of thyroid abnormalities and iodine deficiency in epidemiological studies. J Clin Endocrinol Metab 2001, 86: 3599–603.
Zimmermann MB, de Benoist B, Corigliano S, et al. Assessment of iodine status using dried blood spot thyroglobulin: development of reference material and establishment of an international reference range in iodine-sufficient children. J Clin Endocrinol Metab 2006, 91: 4881–7.
Vejbjerg P, Knudsen N, Perrild H, et al. Thyroglobulin as a marker of iodine nutrition status in the general population. Eur J Endocrinol 2009, 161: 475–81.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nazeri, P., Mirmiran, P., Asghari, G. et al. Differences between subjects with sufficient and deficient urinary iodine in an area of iodine sufficiency. J Endocrinol Invest 34, e302–e307 (2011). https://doi.org/10.3275/7839
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.3275/7839