Abstract—
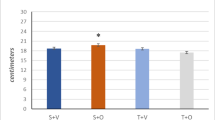
The production of reactive oxygen species (ROS) in skeletal muscle cells increases under contraction. Respiratory and locomotor muscles differ in contraction modes; therefore, ROS production and their effect on blood vessels in these functionally different types of muscles may differ. The aim of this work was to assess the role of ROS in the tone regulation of the diaphragm artery (a. phrenica) and deep brachial artery (a. profunda brachii) of the rat. The reactions of ring preparations of the arteries were studied in the isometric regimen. The NADPH oxidase (NOX) inhibitor VAS2870 caused relaxation of the preparations; the reaction magnitude of the diaphragm arteries was greater than that of the brachial arteries: at the VAS2870 concentration of 1 μM, the contraction force decreased to 33 and 91% of the precontraction level, respectively. Tiron (\({\text{O}}_{2}^{{\centerdot - }}\) scavenger) had a similar activity profile: at the concentration of 10 mM, it caused a decrease in the contraction force of the diaphragm arteries to 38% and of the brachial arteries to 66% of the initial contraction force. Catalase, which destroys H2O2, did not affect contraction of the diaphragm arteries at the concentration of 3000 U/mL but increased contraction of the deep brachial arteries. Using the method of quantitative polymerase chain reaction, it was shown that the mRNA content of NOX isoforms, p22phox, p47phox, p67phox, Poldip2, Gpx-1, SOD-1, and catalase in the tissue of two arteries does not differ, while the content of SOD-3 mRNA in the diaphragm arteries is lower than in the brachial arteries. Thus, \({\text{O}}_{2}^{{\centerdot - }}\) produced by NOX greater increases tonic contraction of the diaphragm arteries than arteries of the locomotor muscle. H2O2, on the contrary, causes relaxation of the locomotor muscle arteries but not the diaphragm arteries. A relatively low level of SOD-3 expression may be a reason for the pronounced effect of O2– in the diaphragm arteries.



Similar content being viewed by others
REFERENCES
Aldosari, S., Awad, M., Harrington, E.O., Sellke, F.W., and Abid, M.R., Subcellular reactive oxygen species (ROS) in cardiovascular pathophysiology, Antioxidants (Basel), 2018, vol. 7, no. 1, p. 14.
Tejero, J., Shiva, S., and Gladwin, M.T., Sources of vascular nitric oxide and reactive oxygen species and their regulation, Physiol. Rev., 2019, vol. 99, no. 1, pp. 311–379.
Knock, G.A., NADPH oxidase in the vasculature: Expression, regulation and signalling pathways; role in normal cardiovascular physiology and its dysregulation in hypertension, Free Radical Biol. Med., 2019, vol. 145, pp. 385–427.
Lassegue, B., Martin, A., and Griendling, K.K., Biochemistry, physiology, and pathophysiology of NADPH oxidases in the cardiovascular system, Circ. Res., 2012, vol. 110, no. 10, pp. 1364–1390.
Wang, Y., Branicky, R., Noë, A., and Hekimi, S., Superoxide dismutases: dual roles in controlling ROS damage and regulating ROS signaling, J. Cell Biol., 2018, vol. 217, no. 6, pp. 1915–1928.
Powers, S.K., Radak, Z., and Ji, L.L., Exercise-induced oxidative stress: past, present and future, J. Physiol., 2016, vol. 594, no. 18, pp. 5081–5092.
Chatterjee, S. and Fisher, A.B., Mechanotransduction in the endothelium: role of membrane proteins and reactive oxygen species in sensing, transduction, and transmission of the signal with altered blood flow, Antioxid. Redox Signaling, 2014, vol. 20, no. 6, pp. 899–913.
Hussain, S.N., Regulation of ventilatory muscle blood flow, J. Appl. Physiol., 1996, vol. 81, no. 4, pp. 1455–1468.
Polla, B., D’Antona, G., Bottinelli, R., and Reggiani, C., Respiratory muscle fibres: specialisation and plasticity, Thorax, 2004, vol. 59, no. 9, pp. 808–817.
Borzykh, A.A., Vinogradova, O.L., and Tarasova, O.S., Diaphragm: the relationship between blood supply regulation and characteristics of the contractile function, Moscow Univ. Biol. Sci. Bull., 2020, vol. 75, no. 2, pp.41–49.
Tarasova, O.S., Kalenchuk, V.U., Borzykh, A.A., Andreev-Andrievsky, A.A., Buravkov, S.V., Sharova, A.P., and Vinogradova, O.L., A comparative analysis of the vasomotor responses and innervation of small arteries in rat locomotor and respiratory muscles, Biophysics (Moscow), 2008, vol. 53, no. 6, pp. 621–625.
Mulvany, M.J. and Halpern, W., Contractile properties of small arterial resistance vessels in spontaneously hypertensive and normotensive rats, Circ. Res., 1977, vol. 41, no. 1, pp. 19–26.
Altenhöfer, S., Kleikers, P.W.M., Radermacher, K.A., Scheurer, P., Hermans, J.J.R., Schiffers, P., Ho, H., Wingler, K., and Schmidt, H.H.H.W., The NOX toolbox: validating the role of NADPH oxidases in physiology and disease, Cell Mol. Life Sci., 2012, vol. 69, no. 14, pp. 2327–2343.
Taiwo, F.A., Mechanism of tiron as scavenger of superoxide ions and free electrons, Spectroscopy, 2008, vol. 22, no. 6, pp. 491–498.
Borzykh, A.A., Andreev-Andrievskiy, A.A., Kalenchuk, V.U., Mochalov, S.V., Buravkov, S.V., Kuzmin, I.V., Borovik, A.S., Vinogradova, O.L., and Tarasova, O.S., Strategies of adaptation of small arteries in diaphragm and gastrocnemius muscle to aerobic exercise training, Hum. Physiol., 2017, vol. 43, no. 4, pp. 437–445.
Braun, D., Zollbrecht, C., Dietze, S., Schubert, R., Golz, S., Summer, H., Persson, P.B., Carlstrom, M., Ludwig, M., and Patzak, A., Hypoxia/reoxygenation of rat renal arteries impairs vasorelaxation via modulation of endothelium-independent sGC/cGMP/PKG signaling, Front. Physiol., 2018, vol. 9, p. 480.
Li, H., Wang, Y., Feng, D., Liu, Y., Xu, M., Gao, A., Tian, F., Zhang, L., Cui, Y., Wang, Z., and Chen, G., Alterations in the time course of expression of the Nox family in the brain in a rat experimental cerebral ischemia and reperfusion model: effects of melatonin, J. Pineal Res., 2014, vol. 57, no. 1, pp. 110–119.
Chen, X., Qi, L., Fan, X., Tao, H., Zhang, M., Gao, Q., Liu, Y., Xu, T., Zhang, P., Su, H., Tang, J., and Xu, Z., Prenatal hypoxia affected endothelium-dependent vasodilation in mesenteric arteries of aged offspring via increased oxidative stress, Hypertens. Res., 2019, vol. 42, no. 6, pp. 863–875.
Lima, T.I., Monteiro, I.C., Valenca, S., Leal-Cardoso, J.H., Fortunato, R.S., Carvalho, D.P., Teodoro, B.G., and Ceccatto, V.M., Effect of exercise training on liver antioxidant enzymes in STZ-diabetic rats, Life Sci., 2015, vol. 128, pp. 64–71.
Lyle, A.N., Deshpande, N.N., Taniyama, Y., Seidel-Rogol, B., Pounkova, L., Du, P., Papaharalambus, C., Lassegue, B., and Griendling, K.K., Poldip2, a novel regulator of Nox4 and cytoskeletal integrity in vascular smooth muscle cells, Circ. Res., 2009, vol. 105, no. 3, pp. 249–259.
Knock, G.A., Snetkov, V.A., Shaifta, Y., Connolly, M., Drndarski, S., Noah, A., Pourmahram, G.E., Becker, S., Aaronson, P.I., and Ward, J.P.T., Superoxide constricts rat pulmonary arteries via Rho-kinase-mediated Ca2+ sensitization, Free Radical Biol. Med., 2009, vol. 46, no. 5, pp. 633–642.
Lai, E.Y., Wellstein, A., Welch, W.J., and Wilcox, C.S., Superoxide modulates myogenic contractions of mouse afferent arterioles, Hypertension, 2011, vol. 58, no. 4, pp. 650–656.
Tsai, M-H. and Jiang, M.J., Reactive oxygen species are involved in regulating alpha1-adrenoceptor-activated vascular smooth muscle contraction, J. Biomed. Sci., 2010, vol. 17.
Bleeke, T., Zhang, H., Madamanchi, N., Patterson, C., and Faber, J.E., Catecholamine-induced vascular wall growth is dependent on generation of reactive oxygen species, Circ. Res., 2004, vol. 94, no. 1, pp. 37–45.
Shimokawa, H., Yasutake, H., Fujii, K., Owada, M.K., Nakaike, R., Fukumoto, Y., Takayanagi, T., Nagao, T., Egashira, K., Fujishima, M., and Takeshita, A., The importance of the hyperpolarizing mechanism increases as the vessel size decreases in endothelium-dependent relaxations in rat mesenteric circulation, J. Cardiovasc. Pharmacol., 1996, vol. 28, no. 5, pp. 703–711.
Garland, C.J., Plane, F., Kemp, B.K., and Cocks, T.M., Endothelium-dependent hyperpolarization: a role in the control of vascular tone, Trends Pharmacol. Sci., 1995, vol. 16, no. 1, pp. 23–30.
Kuzkaya, N., Weissmann, N., Harrison, D.G., and Dikalov, S., Interactions of peroxynitrite, tetrahydrobiopterin, ascorbic acid, and thiols: implications for uncoupling endothelial nitric-oxide synthase, J. Biol. Chem., 2003, vol. 278, no. 25, pp. 22546–22554.
Shimokawa, H., Reactive oxygen species in cardiovascular health and disease: special references to nitric oxide, hydrogen peroxide, and Rho-kinase, J. Clin. Biochem. Nutr., 2020, vol. 66, no. 2, pp. 83–91.
Knock, G.A., NADPH oxidase in the vasculature: expression, regulation and signalling pathways; role in normal cardiovascular physiology and its dysregulation in hypertension, Free Radical Biol. Med., 2019, vol. 145, pp. 385–427.
Montezano, A.C. and Touyz, R.M., Reactive Oxygen Species and the Cardiovascular System, Integrated Systems Physiology Series, Glasgow: Morgan and Claypool, 2012.
Vogel, P.A., Yang, X., Moss, N.G., and Arendshorst, W.J., Superoxide enhances Ca2+ entry through L-type channels in the renal afferent arteriole, Hypertension, 2015, vol. 66, no. 2, pp. 374–381.
Jin, L., Ying, Z., and Webb, R.C., Activation of Rho/Rho kinase signaling pathway by reactive oxygen species in rat aorta, Am. J. Physiol.: Heart Circ. Physiol., 2004, vol. 287, no. 4, pp. H1495–H1500.
Somlyo, A.P. and Somlyo, A.V., Ca2+ sensitivity of smooth muscle and nonmuscle myosin II: modulated by G proteins, kinases, and myosin phosphatase, Physiol. Rev., 2003, vol. 83, no. 4, pp. 1325–1358.
Funding
This work was financially supported by the Russian Science Foundation, project no. 19-75-00060.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests. The authors declare that they have no conflict of interests.
Statement on the welfare of animals. The experiments were carried out in compliance with the ethical standards of working with animals established by the Bioethics Commission of the Institute for Biomedical Problems of the Russian Academy of Sciences.
Statement of compliance with standards of research involving humans as subjects. This article does not contain any studies involving humans as subjects.
Additional information
Translated by D. Novikova
About this article
Cite this article
Borzykh, A.A., Shvetsova, A.A., Kuzmin, I.V. et al. The Role of Reactive Oxygen Species in the Tone Regulation of Respiratory and Locomotor Muscle Arteries of the Rat. Moscow Univ. Biol.Sci. Bull. 76, 111–117 (2021). https://doi.org/10.3103/S0096392521030020
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.3103/S0096392521030020