Abstract
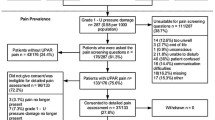
When conducting prevalence surveys pressure ulcers were found in participants clearly identified not to be at risk. This article determines and analyses persons in German hospitals and nursing homes who suffer from pressure ulcers but are not at risk. In the years 2002, 2003 and 2004 there were 7,097 nursing home residents and 23,966 hospital patients examined in annual pressure ulcer prevalence surveys. A risk assessment according to the Braden Scale was performed for each participant on the day of the survey. “Not at risk” participants were defined by Braden score cut-off > 20 points. There were 440 of 3,012 (14.6%) persons with pressure ulcer who were considered not to be at risk. In hospitals, 16.1% of all patients with pressure ulcers were not at risk, in nursing homes it was 8.2%. A high variance between medical specialties and individual institutions was found in the number of those not at risk but with pressure ulcer. In the group not at risk, persons with and without a pressure ulcer differed regarding activity and friction and shear in nursing homes. In hospitals those persons differed regarding age and all single items of the Braden scale apart from sensory perception. Pressure ulcers that are more severe, located at the hip or lower back or the origin of which is unknown are more likely to be considered to be at risk by the Braden risk assessment tool.
The results may indicate insufficient abilities of the Braden scale for certain kind of pressure ulcer wounds.
Similar content being viewed by others
References
R.N. Kumar, G.V. Gupchup, M.A. Dodd, B. Shah, M. Iskedjian, T.R. Einarson and D.W. Raisch: “Direct health care costs of 4 common skin ulcers in New Mexico Medicaid fee-for-service patients”, Adv. Skin Wound. Care, Vol. 17, (2004), pp. 143–149.
G. Bennett, C. Dealey and J. Posnett: “The cost of pressure ulcers in the UK,” Age Ageing, Vol. 33, (2004), pp. 230–235.
S.M. Gallagher: “Outcomes in clinical practice: pressure ulcer prevalence and incidence studies”, Ostomy Wound Manage, Vol. 43, (1997), pp. 28–32, 34-35, 38; quiz 39–40.
E. Kaltenthaler, M.D. Whitfield, S.J. Walters, R.L. Akehurst and S. Paisley: “UK, USA and Canada: how do their pressure ulcer prevalence and incidence data compare?”, J. Wound Care, Vol. 10, (2001), pp. 530–535.
G.J. Bours, R.J. Halfens, M.J. Candel, R.T. Grol and H.H. Abu-Saad: “A pressure ulcer audit and feedback project across multi-hospital settings in the Netherlands”, Int. J. Qual. Health Care, Vol. 16, (2004), pp. 211–218.
K.T. Whittington and R. Briones: “National Prevalence and Incidence Study: 6-year sequential acute care data”, Adv. Skin Wound Care, Vol. 17, (2004), pp. 490–494.
J. Fletcher: “How can we improve prevalence and incidence monitoring?,” J. Wound Care, Vol. 10, (2001), pp. 311–314.
F. Scott and A. Newens: “Hospital monitoring of pressure ulcers in the UK”, J. Wound Care, Vol. 8, (1999), pp. 221–224.
E. Bethell: “Incidence and prevalence data: can we ensure greater accuracy?,” J. Wound Care, Vol. 11, (2002), pp. 285–288.
NPUAP: “National pressure ulcer advisory panel, frequently asked questions: what is prevalence?”, http://www.npuap.org/FAQP&I.htm, assessed 21.05.2005.
C.A. Barczak, R.I. Barnett, E.J. Childs and L.M. Bosley: “Fourth national pressure ulcer prevalence survey”, Adv. Wound Care, Vol. 10, (1997), pp. 18–26.
M. Meraviglia, H. Becker, S.J. Grobe and M. King: “Maintenance of skin integrity as a clinical indicator of nursing care”, Adv. Skin Wound Care, Vol. 15, (2002), pp. 24–29.
K. Zulkowski: “More on pressure ulcers in long-term care”, Adv. Skin Wound Care, Vol. 17, (2004), pp. 216.
S. Biasioli, A. Destrebecq, S. Longobardo, A. Negri, P. Tacconi and A. Sponton: “Prevalence of decubitus lesions in a hospital in Lombardia”, Assist. Inferm. Ric., Vol. 21, (2002), pp. 14–16.
N.A. Lahmann, R.J. Halfens, and T. Dassen: “Prevalence of pressure ulcers in Germany”, J. Clin. Nurs., Vol. 14, (2005), pp. 165–172.
N.O. Lake: “Measuring incidence and prevalence of pressure ulcers for intergroup comparison”, Adv. Wound Care, Vol. 12, (1999), pp. 31–34.
G.J. Bours, R.J. Halfens, M.P. Berger, H. Huijer Abu-Saad and R.T. Grol: “Development of a model for case-mix adjustment of pressure ulcer prevalence rates”, Med. Care, Vol. 41, (2003), pp. 45–55.
D.R. Berlowitz, A.S. Ash, G.H. Brandeis, H.K. Brand, J.L. Halpern, and M.A. Moskowitz: “Rating long-term care facilities on pressure ulcer development: importance of case-mix adjustment”, Ann. Internal Med., Vol. 124, (1996), pp. 557–563.
A. Tannen, T. Dassen, G. Bours and R. Halfens: “A comparison of pressure ulcer prevalence: concerted data collection in the Netherlands and Germany”, Int. J. Nurs. Stud., Vol. 41, (2004), pp. 607–612.
L. Schoonhoven, J.R. Haalboom, M.T. Bousema, A. Algra, D.E. Grobbee, M.H. Grypdonck and E. Buskens: “Prospective cohort study of routine use of risk assessment scales for prediction of pressure ulcers”, Bmj, Vol. 325, (2002), pp. 797.
S. Wellard and S.K. Lo: “Comparing Norton, Braden and Waterlow risk assessment scales for pressure ulcers in spinal cord injuries”, Contemp. Nurse, Vol. 9, (2000), pp. 155–160.
G. J. Bours, R.J. Halfens, M. Lubbers and J.R. Haalboom: “The development of a national registration form to measure the prevalence of pressure ulcers in The Netherlands”, Ostomy/Wound Management, Vol. 45, (1999), pp. 28–33, 36–38, 40.
T. Defloor and L. Schoonhoven: “Inter-rater reliability of the EPUAP pressure ulcer classification system using photographs”, J. Clin. Nurs., Vol. 13, (2004), pp. 952–959.
EPUAP: “Pressure Ulcer Treatment Guidelines Treatment”, http://www.epuap.org/, assessed 08.01.2005
R.J. Halfens: “Risk assessment scales for pressure ulcers: a theoretical, methodological, and clinical perspective”, Ostomy/Wound Management, Vol. 46, (2000), pp. 36–40, 42-4.
A.R. Fisher, G. Wells and M.B. Harrison: “Factors associated with pressure ulcers in adults in acute care hospitals”, Adv. Skin Wound Care, Vol. 17, (2004), pp. 80–90.
M. Lindgren, M. Unosson, M. Fredrikson and A.C. Ek: “Immobility-a major risk factor for development of pressure ulcers among adult hospitalized patients: a prospective study”, Scand. J. Caring Sci., Vol. 18, (2004), pp. 57–64.
Author information
Authors and Affiliations
About this article
Cite this article
Lahmann, N.A., Halfens, R.J. & Dassen, T. Not at risk — Nevertheless a pressure ulcer. cent.eur.j.med 1, 270–283 (2006). https://doi.org/10.2478/s11536-006-0025-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.2478/s11536-006-0025-8