Abstract
Background and objective: Previous work has suggested that people with poor health-related quality of life (HR-QOL) as a result of asthma are willing to pay the most for successful therapy. There is also evidence that preferences are an important influence on adherence to therapy. We report a patient preference study using a discrete-choice experiment (DCE) to elicit willingness to pay (WTP) of patients with asthma in Spain, the Netherlands, and the UK.
Methods: The DCE survey included different attributes of asthma therapy (days with symptoms, days needing reliever medication, asthma attacks [none, attack that does not require doctor/emergency room {ER} visit, attack that requires doctor/ER visit], risk of adverse effects, number of preventer inhalers, and monthly out-of-pocket costs). Participants indicated which attribute combinations they preferred. The questionnaire survey included the mini Asthma Quality of Life Questionnaire (mAQLQ). The validity of the choice experiment has been supported by two pilot studies conducted in the UK. Preferences and WTP were estimated using a random effects probit model. Symptom days and asthma attack attributes were segmented by mAQLQ score.
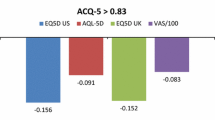
Results: Demographic and clinical data were compared between the three country samples (UK, n = 124; Spain, n = 86; the Netherlands, n = 269). All study attributes were independently significant predictors of choice. People were willing to pay €35 per month to avoid a day with symptoms, and €109 per month (year 2005 values) to avoid experiencing asthma attacks that required emergency visits to their doctor or hospital. People with the worst HR-QOL were willing to pay the least to avoid days with symptoms and asthma attacks that required visits to their doctor/ER. This was not an income-related effect.
Conclusion: Patients who reported higher HR-QOL were willing to pay more to avoid days with symptoms and asthma attacks that required visits to their doctor/ER. Hypotheses were explored to explain this effect. It is possible that people with the least impairment of HR-QOL place the greatest value on avoiding the effects of asthma and so are most willing to alter their behavior. People with the worst HR-QOL may be exhibiting a response shift type of effect whereby their internal values are shifted down by the burden of their disease. These findings may help to illuminate why there are differences in asthma treatment adherence.





Similar content being viewed by others
References
Protheroe J, Fahey T, Montgomery AA, et al. Effects of patients’s preferences on the treatment of atrial fibrillation: observational study of patient-based decision analysis. West J Med 2001; 174(5): 311–5
Rivers SE, Salovey P, Pizarro DA, et al. Message framing and Pap test utilization among women attending a community health clinic. J Health Psychol 2005; 10(1): 65–77
Sen A. Behaviour and the concept of preference. Economica 1973; 40(159): 241–59
Petrie KJ, Weinman J. Why illness perceptions matter. Clinical Medicine 2006; 6(6): 536–9
Peters J, Stevenson M, Beverly C, et al. Clinical and cost effectiveness of inhaler devices used in the routine management of chronic asthma in older children. Health Technol Assess 2002; 6(5): 1–167
Currie GP, Devereux GS, Lee DK, et al. Recent developments in asthma management. BMJ 2005; 330: 585–9
Shah S, Peat J, Mazurski E. Effect of peer led programme for asthma education in adolescents: cluster randomised controlled trial. BMJ 2001; 322: 583–7
Juniper EF, Guyatt G, Epstein RS, et al. Evaluation of impairment of health-related quality of life in asthma: development of a questionnaire for use in clinical trials. Thorax 1992; 47: 76–83
Juniper EF, Guyatt GH, Ferrie PJ, et al. Measuring quality of life in asthma. Am Rev Respir Dis 1993; 147: 832–8
Juniper EF, Guyatt GH, Cox FM, et al. Development and validation of the mini Asthma Quality of Life Questionnaire. Eur Respir J 1999; 14: 32–8
Johannsson G, Stallberg Tornling G, Anderson S, et al. Asthma treatment preference study: a conjoint analysis of preferred drug treatments. Chest 2004; 125: 916–23
Osman LM, McKenzie L, Cairns J, et al. Patient weighting of importance of asthma symptoms. Thorax 2001; 56: 138–42
Ratcliffe J, van Haselen R, Buxton M, et al. Assessing patients’ preferences for characteristics associated with homeopathic and conventional treatment of asthma: a conjoint analysis study. Thorax 2002; 57: 503–8
Lancsar EJ, Hall JP, King M, et al. Using discrete choice experiments to investigate subject preferences for preventive asthma medication. Respirology 2007; 12: 127–36
Zillich AJ, Blumenschein K, Johannesson M, et al. Assessment of the relationship between measures of disease severity, quality of life, and willingness to pay in asthma. Pharmacoeconomics 2002; 20(4): 257–65
Blumenschein K, Johannesson M. Relationship between quality of life instruments, health state utilities, and willingness to pay in patients with asthma. Ann Allergy Asthma Immunol 1998; 80: 189–94
Lloyd AJ, Mclntosh E, Rabe K, et al. Patient preferences for asthma therapy: a discrete choice experiment. Prim Care Respir J 2007; 16: 241–8
Global Initiative for Asthma (GINA). Pocket guide for asthma management and prevention, 2004 [online]. Available from URL: http://www.ginasthma.com [Accessed 2005 Mar]
Sloane NJA. A library of orthogonal arrays [online]. Available from URL: http://www.research.att.com/~njas/oadir/ [Accessed 2005 May]
Green W. LIMDEP version 8: users manual. Plainview (NY): Econometric Software Inc., 1998 [online]. Available from URL: http://www.limdep.com [Accessed 2005 Dec]
Sprangers M, Schwartz C. Adaptation to changing health: response shift in quality-of-life research. Oxford (UK): Oxford University Press, 2000
Lloyd A, Mclntosh E, Price M. The importance of drug adverse effects compared with seizure control for people with epilepsy: a discrete choice experiment. Pharmacoeconomics 2005; 23(11): 1167–81
Acknowledgements
This work was supported by GlaxoSmithKline. Angela Williams is an employee of GlaxoSmithKline and as such receives shares. Klaus Rabe has served as consultant to GlaxoSmithKline in the past. The other authors have no conflicts of interest that are directly relevant to the content of this study. The authors would like to acknowledge the help of Megan Stafford in preparing this manuscript and Scott Doyle for managing the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lloyd, A., McIntosh, E., Williams, A.E. et al. How Does Patients’ Quality of Life Guide Their Preferences Regarding Aspects of Asthma Therapy?. Patient-Patient-Centered-Outcome-Res 1, 309–316 (2008). https://doi.org/10.2165/1312067-200801040-00012
Published:
Issue Date:
DOI: https://doi.org/10.2165/1312067-200801040-00012