Abstract
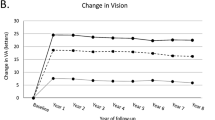
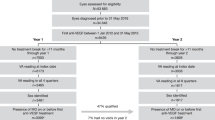
Central retinal vein occlusion (CRVO) remains an important cause of visual loss. Impaired venous drainage leads to retinal hypoxia with upregulation and release of vascular endothelial growth factor (VEGF). VEGF increases vascular permeability and leads to the breakdown of the blood-retinal barrier, with the development of macular oedema. Treatment strategies for macular oedema in CRVO currently under evaluation focus on VEGF blockage. Bevacizumab is a humanized monoclonal antibody that blocks VEGF. It has been evaluated in a clinical trial that compared intravitreal injections of bevacizumab 1.25 mg with sham injections every 6 weeks. At the end of a 24-week follow-up period, 60.0% of patients in the bevacizumab group had gained ≥15 letters compared with 20.0% in the control group (p = 0.003). Aflibercept (previously VEGF Trap-Eye) is a 115kD decoy receptor fusion protein. Aflibercept is capable of binding both VEGF and placental growth factor (PlGF). By blocking both VEGF and PlGF, aflibercept could be more effective than other anti-VEGF drugs. Two clinical trials have evaluated the efficacy of aflibercept for the treatment of macular oedema in CRVO: COPERNICUS and GALILEO. Both included a similar 6-month phase, during which patients were randomized to receive either an intravitreal injection of aflibercept 2 mg or a sham injection every month. In a second 6-month phase of the GALILEO study, patients in the treatment group were treated on an as needed (PRN) basis with aflibercept, while patients in the placebo group continued with sham injections. In the second 6-month phase in the COPERNICUS study, all patients were treated with aflibercept on a PRN basis. Treatment with aflibercept led to an improvement in visual acuity of ≥15 letters in 55.3% (COPERNICUS) and 60.2% of patients (GALILEO). Patients initially in the placebo group and then treated PRN gained only a mean of 3.8 letters, with 30.1% achieving a visual gain of ≥15 letters (COPERNICUS). The percentage of patients that improved by ≥15 letters was 32.4% for the group receiving sham injections throughout the GALILEO study.
In summary, VEGF blockage has been proven to improve visual outcomes in patients with macular oedema due to CRVO. However, an important disadvantage of anti-VEGF drugs is the need for frequent reinjections and even more frequent control visits. Further advances are needed in order to improve quality of life and reduce the burden to healthcare systems.






Similar content being viewed by others
References
Rogers S, McIntosh RL, Cheung N, et al. The prevalence of retinal vein occlusion: pooled data from population studies from the United States, Europe, Asia, and Australia. Ophthalmology 2010; 117: 313–9
McIntosh RL, Rogers SL, Lim L, et al. Natural history of central retinal vein occlusion: an evidence-based systematic review. Ophthalmology 2010; 117: 1113–23
No authors listed. Evaluation of grid pattern photocoagulation for macular edema in central vein occlusion. The Central Vein Occlusion Study Group M report. Ophthalmology 1995; 102: 1425–33
No authors listed. A randomized clinical trial of early panretinal photocoagulation for ischemic central vein occlusion. The Central Vein Occlusion Study Group N report. Ophthalmology 1995; 102: 1434–44
Aiello LP, Avery RL, Arrigg PG, et al. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med 1994; 331: 1480–7
Boyd SR, Zachary I, Chakravarthy U, et al. Correlation of increased vascular endothelial growth factor with neovascularization and permeability in ischemic central vein occlusion. Arch Ophthalmol 2002; 120: 1644–50
Noma H, Funatsu H, Mimura T, et al. Vitreous levels of interleukin-6 and vascular endothelial growth factor in macular edema with central retinal vein occlusion. Ophthalmology 2009; 116: 87–93
Brown DM, Michels M, Kaiser PK, et al. Ranibizumab versus verteporfin photodynamic therapy for neovascular age-related macular degeneration: two-year results of the ANCHOR study. Ophthalmology 2009; 116: 57–65
Rosenfeld PJ, Brown DM, Heier JS, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med 2006; 355: 1419–31
Algvere PV, Epstein D, von WG, et al. Intravitreal bevacizumab in central retinal vein occlusion: 18-month results of a prospective clinical trial. Eur J Ophthalmol 2011; 21: 789–95
Figueroa MS, Contreras I, Noval S, et al. Results of bevacizumab as the primary treatment for retinal vein occlusions. Br J Ophthalmol 2010; 94: 1052–6
Priglinger SG, Wolf AH, Kreutzer TC, et al. Intravitreal bevacizumab injections for treatment of central retinal vein occlusion: six-month results of a prospective trial. Retina 2007; 27: 1004–12
Rensch F, Jonas JB, Spandau UH. Early intravitreal bevacizumab for non-ischaemic central retinal vein occlusion. Acta Ophthalmol 2009; 87: 77–81
Epstein DL, Algvere PV, von WG, et al. Bevacizumab for macular edema in central retinal vein occlusion: a prospective, randomized, double-masked clinical study. Ophthalmology 2012; 119: 1184–9
Brown DM, Campochiaro PA, Singh RP, et al. Ranibizumab for macular edema following central retinal vein occlusion: six-month primary end point results of a phase III study. Ophthalmology 2010; 117: 1124–33
Haller JA, Bandello F, Belfort Jr R, et al. Dexamethasone intravitreal implant in patients with macular edema related to branch or central retinal vein occlusion twelve-month study results. Ophthalmology 2011; 118: 2453–60
Yeh WS, Haller JA, Lanzetta P, et al. Effect of the duration of macular edema on clinical outcomes in retinal vein occlusion treated with dexamethasone intravitreal implant. Ophthalmology 2012; 119: 1190–8
Scott IU, VanVeldhuisen PC, Oden NL, et al. Baseline predictors of visual acuity and retinal thickness outcomes in patients with retinal vein occlusion: Standard Care Versus COrticosteroid for REtinal Vein Occlusion Study report 10. Ophthalmology 2011; 118: 345–52
Bakri SJ, Snyder MR, Reid JM, et al. Pharmacokinetics of intravitreal bevacizumab (Avastin). Ophthalmology 2007; 114: 855–9
Economides AN, Carpenter LR, Rudge JS, et al. Cytokine traps: multi-component, high-affinity blockers of cytokine action. Nat Med 2003; 9: 47–52
Holash J, Davis S, Papadopoulos N, et al. VEGF-Trap: a VEGF blocker with potent antitumor effects. Proc Natl Acad Sci U S A 2002 Aug 20; 99(17): 11393–8
Stewart MW, Rosenfeld PJ. Predicted biological activity of intravitreal VEGF Trap. Br J Ophthalmol 2008; 92: 667–8
Heier JS, Boyer D, Nguyen QD, et al. The 1-year results of CLEAR-IT 2, a phase 2 study of vascular endothelial growth factor trap-eye dosed as-needed after 12-week fixed dosing. Ophthalmology 2011; 118: 1098–106
Chong V. Biological, preclinical and clinical characteristics of inhibitors of vascular endothelial growth factors. Ophthalmologica 2012; 227 Suppl. 1: 2–10
Boyer D, Heier J, Brown DM, et al. Vascular endothelial growth factor Trap-Eye for macular edema secondary to central retinal vein occlusion: six-month results of the phase 3 COPERNICUS study. Ophthalmology 2012; 119: 1024–32
Brown DM, Haller JA, Boyer DS, et al. Intravitreal aflibercept injection in central retinal vein occlusion: 1-year results of the phase 3 COPERNICUS study [poster 936/D980; online]. Available from URL: http://www.abstractsonline.com/Plan/ViewAbstract.aspx?sKey=bbef02a2-33ce-49b8-9f80-df7344f29dd9&cKey=78d01ea9-f56f-447e-905b-b8bcf022799e&mKey={F0FCE029-9BF8-4E7C-B48E-9FF7 711D4A0E} [Accessed 2012 Sep 24]
Holz FG, Ogura Y, Roider J, et al. Intravitrial aflibercept injection for macular edema in central retinal vein occlusion: 1-year results of the phase 3 GALILEO study [poster 6929; online]. Available from URL: http://www.abstractsonline.com/Plan/ViewAbstract.aspx?sKey=814fffc0-cf7f-4105-8512-7c3124959453&cKey=79b91efa-d330-461e-a9fa-4f5d6905dc36&mKey={F0FCE029-9BF8-4E7C-B48E-9FF 7711D4A0E} [Accessed 2012 Sep 24]
Comparison of Age-related Macular Degeneration Treatments Trials (CATT) Research Group. Ranibizumab and bevacizumab for treatment of neovascular age-related macular degeneration: two-year results. Ophthalmology 2012 Jul; 119(7): 1388–98
Genentech. Ranibizumab DosE Comparison and the Role of LAser in REtinal Vein Occlusions (RELATE) [Clinical-Trials.gov identifier NCT01003106]. US National Institutes of Health, ClinicalTrials.gov [online]. Available from URL: http://www.clinicaltrials.gov [Accessed 2012 Sep 15]
Acknowledgements
No funding was received for the preparation of this manuscript. The authors have no conflict of interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Figueroa, M.S., Contreras, I. Potential Anti-Vascular Endothelial Growth Factor Therapies for Central Retinal Vein Occlusion. Drugs 72, 2063–2071 (2012). https://doi.org/10.2165/11640820-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11640820-000000000-00000