Abstract
Introduction: Venous thromboembolism (VTE) is a common and potentially avoidable cause of morbidity and mortality in patients hospitalized for acute medical illness.
Objective: Our objective was to conduct a systematic review of studies that assessed the efficacy and safety of new oral anticoagulant (OAC) drugs versus standard pharmacological drugs and/or placebo in prevention of VTE in acute medically ill patients.
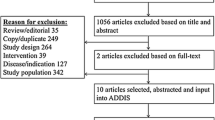
Methods: PubMed.org and ClinicalTrials.gov databases were searched to identify studies that evaluated the efficacy and safety of a new OAC versus the standard pharmacological treatment and/or placebo in the prevention of VTE in medically ill patients. Relative risks (RR), weighted means and 95% CIs were calculated. Statistical heterogeneity was evaluated using Chi2 and I2 statistics.
Two studies were included in the meta-analysis. The primary outcome in both studies was the composite of VTE-related death, symptomatic non-fatal pulmonary embolism (PE), symptomatic deep venous thrombosis (DVT) and asymptomatic proximal DVT. Both studies compared a factor (F)Xa inhibitor with enoxaparin in standard short-term thromboprophylaxis followed by a period where the FXa inhibitor was compared with placebo as prolonged thromboprophylaxis in medically ill patients. The primary major safety outcome in both studies was a composite of treatment-related major bleeding and clinically relevant non-major bleeding. A total of 14 629 patients were randomized.
Results: Compared with subjects treated with enoxaparin followed by placebo, the RR of the primary outcome during the prolonged treatment period was 0.79 (95% CI 0.66, 0.94), the RR for the primary outcome during the first short-term treatment period was 1.03 (95% CI 0.81, 1.31). For major bleeding during the prolonged treatment period, the RR was 2.69 (95% CI 1.65, 4.39) for patients treated with an FXa inhibitor compared with enoxaparin/placebo. For major bleeding during the shorter treatment period, the RR was 2.01 (95% CI 1.10, 3.65) in favour of enoxaparin.
Conclusion: In acute medically ill patients, prolonged thromboprophylaxis with an oral FXa inhibitor is more protective than regular short-term treatment with enoxaparin. However, treatment with FXa inhibitors is significantly associated with major bleeding, both in long- and short-term treatment compared with enoxaparin.









Similar content being viewed by others
References
Kahn SR, Lim W, Dunn AS, et al. Prevention of VTE in nonsurgical patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2012; 141 (2 Suppl.): e195S-226S
Piazza G, Fanikos J, Zayaruzny M, et al. Venous thromboembolic events in hospitalised medical patients. Thromb Haemost 2009; 102 (3): 505–10
Heit JA, Silverstein MD, Mohr DN, et al. Risk factors for deep vein thrombosis and pulmonary embolism. Arch Intern Med 2000; 160: 809–15
Heit JA, O’Fallon MW, Petterson TM, et al. Relative impact of risk factors for deep vein thrombosis and pulmonary embolism. Arch Intern Med 2002; 162: 1245–8
Spencer FA, Lessard D, Emery C, et al. Venous thromboembolism in the outpatient setting. Arch Intern Med 2007; 167 (14): 1471–5
White RH, Zhou H, Romano PS. Incidence of symptomatic venous thromboembolism after different elective or urgent surgical procedures. Thromb Haemost 2003; 90: 446–55
Stein PD, Henry JW. Prevalence of acute pulmonary embolism among patients in a general hospital and at autopsy. Chest 1995; 108: 978–81
Lindblad B, Eriksson A, Bergqvist D. Autopsy-verified pulmonary embolism in a surgical department: analysis of the period from 1951 to 1988. Br J Surg 1991; 78: 849–52
Sandler DA, Martin JF. Autopsy proven pulmonary embolism in hospital patients: are we detecting enough deep vein thrombosis?. J R Soc Med 1989; 82 (April): 203-5
National Quality Forum (NQF). National voluntary consensus standards for prevention and care of venous thromboembolism: policy, preferred practices, and initial performance measures. A consensus report. Washington, DC: NQF, 2006
Baglin TP, White K, Charles A. Fatal pulmonary embolism in hospitalised medical patients. J Clin Pathol 1997; 50: 609–18
Cohen AT, Tapson VF, Bergmann JF, et al. Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. Lancet 2008; 371: 387–94
Piazza G, Seddighzadeh A, Goldhaber SZ. Double trouble for 2,609 hospitalized medical patients who developed deep vein thrombosis: prophylaxis omitted more often and pulmonary embolism more frequent. Chest 2007; 132 (2): 554–61
Guyatt GH, Akl EA, Crowther M, et al. Executive summary: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2012; 141: 7S–47S
Mousa SA. Oral direct factor Xa inhibitors, with special emphasis on rivaroxaban. Methods Mol Biol 2010; 663 (1): 181–201
Davis EM, Packard KA, Knezevich JT, et al. New and emerging anticoagulant therapy for atrial fibrillation and acute coronary syndrome. Pharmacotherapy 2011; 31 (10): 975–1016
Duggan ST. Rivaroxaban: a review of its use for the prophylaxis of venous thromboembolism after total hip or knee replacement surgery. Am J Cardiovasc Drugs 2012; 12 (1): 57–72
Watson J, Whiteside G, Perry C. Apixaban first global approval. Drugs 2011; 71 (15): 2079–89
Perzborn E, Roehrig S, Straub A, et al. Rivaroxaban: a new oral factor Xa inhibitor. Arterioscler Thromb Vasc Biol 2010; 30: 376–81
Hull RD, Schellong SM, Tapson VF, et al. Extended-duration venous thromboembolism prophylaxis in acutely ill medical patients with recently reduced mobility. Ann Intern Med 2010; 153 (1): 8–18
Själander A, Janson J-H, Bergqvist D, et al. Efficacy and safety of anticoagulant prophylaxis to prevent venous thromboembolism in acutely ill medical inpatients: a meta-analysis. J Intern Med 2008; 263 (1): 52–60
Wein L, Wein S, Haas SJ, et al. Pharmacological venous thromboembolism prophylaxis in hospitalized medical patients. Arch Intern Med 2007; 167 (14): 1476–86
Goldhaber SZ, Leizorovicz A, Kakkar AK, et al. Apixaban versus enoxaparin for thromboprophylaxis in medically ill patients. N Engl J Med 2011; 365 (23): 2167–77
Cohen AT, Spiro TE, Büller HR, et al. Extended-duration rivaroxaban thromboprophylaxis in acutely ill medical patients: MAGELLAN study protocol. J Thromb Thrombolysis 2011 May; 31: 407–16
Hughes S. MAGELLAN: rivaroxaban prevents VTE in medical patients, but bleeding is an issue. 2011 [online]. Available from URL: http://www.theheart.org/article/1207331.do [Accessed 6 Feb 2012]
Connolly SJ, Eikelboom J, Joyner C, et al. Apixaban in patients with atrial fibrillation. N Engl J Med 2011; 364: 806–17
Granger CB, Alexander JH, McMurray JJV, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med 2011; 365: 981–92
Turpie AGG, Bauer KA, Davidson BL, et al. A randomized evaluation of betrixaban, an oral factor Xa inhibitor, for prevention of thromboembolic events after total knee replacement (EXPERT). Thromb Haemost 2009; 101: 68–76
Portola Pharmaceuticals. Betrixaban: long-acting, oral, direct factor Xa inhibitor [online]. Available from URL: http://www.portola.com/Betrixaban [Accessed 2012 Mar 21]
Geerts WH, Bergqvist D, Pineo GF, et al. Prevention of venous thromboembolism: American College of Chest Physicians evidence-based clinical practice guidelines (8th edition). Chest 2008 Jun; 133 (6 Suppl.): 381-453S
Roskell NS, Lip GYH, Noack H, et al. Treatments for stroke prevention in atrial fibrillation: a network meta-analysis and indirect comparisons versus dabigatran etexilate. Thromb Haemost 2010; 104: 1106–15
Edwards SJ, Clarke MJ, Wordsworth S, et al. Indirect comparisons of treatments based on systematic reviews of randomised controlled trials. Int J Clin Pract 2009; 63 (6): 841–54
Bucker HC, Guyatt GH, Griffith LE, et al. The results of direct and indirect treatment comparisons in meta-analysis of randomized controlled trials. J Clin Epidemiol 1997; 50 (6): 683–91
Acknowledgements
IEA and TFO have no conflicts of interest. TBL and LHR have served as speakers for BMS/Pfizer and Boehringer Ingelheim. GYHL has served as a consultant for Bayer, Astellas, Merck, AstraZeneca, Sanofi, BMS/Pfizer and Boehringer Ingelheim, and has been on the speaker bureau for Bayer, BMS/Pfizer, Boehringer Ingelheim and Sanofi.
IEA, TBL and GYHL provided the idea for the article and contributed to drafting and subsequent revisions. IEA performed the analyses and contributed to manuscript revisions. LHR and TFO contributed to manuscript drafts, and made critical revisions for important intellectual content. The authors take full responsibility for the content of the article.
No funding was received for the preparation of this review. This study was conducted fully independent of any industry or other grant support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Albertsen, I.E., Larsen, T.B., Rasmussen, L.H. et al. Prevention of Venous Thromboembolism with New Oral Anticoagulants versus Standard Pharmacological Treatment in Acute Medically Ill Patients. Drugs 72, 1755–1764 (2012). https://doi.org/10.2165/11635630-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11635630-000000000-00000