Abstract
Background
Cardiac arrest due to torsades de pointes (TdP) is a rare but catastrophic event in hospitals. Patients admitted to cardiac units are at higher risk of drug-induced QT interval prolongation and TdP, due to a preponderance of risk factors. Few data exist regarding the prevalence of QT interval prolongation in patients admitted to cardiac units or the frequency of administering QT interval-prolonging drugs to patients presenting with QT interval prolongation.
Objective
The aim of this study was to determine the prevalence of Bazett’s-corrected QT (QTc) interval prolongation upon admission to cardiac units and the proportion of patients presenting with QTc interval prolongation who are subsequently administered QT interval-prolonging drugs during hospitalization.
Methods
This was a prospective, observational study conducted over a 1-year period (October 2008–October 2009) in 1159 consecutive patients admitted to two cardiac units in a large urban academic medical centre located in Indianapolis, IN, USA. Patients were enrolled into the study at the time of admission to the hospital and were followed daily during hospitalization. Exclusion criteria were age <18 years, ECG rhythm of complete ventricular pacing, and patient designation as ‘outpatient’ in a bed and/or duration of stay <24 hours. Data collected included demographic information, past medical history, daily progress notes, medication administration records, laboratory data, ECGs, telemetry monitoring strips and diagnostic reports. All patients underwent continuous cardiac telemetry monitoring and/or had a baseline 12-lead ECG obtained within 4 hours of admission. QT intervals were determined manually from lead II of 12-lead ECGs or from continuous lead II telemetry monitoring strips. QTc interval prolongation was defined as ≥470 ms for males and ≥480 ms for females. In both males and females, QTc interval >500 ms was considered abnormally high. A medication was classified as QT interval-prolonging if there were published data indicating that the drug causes QT interval prolongation and/or TdP. Study endpoints were (i) prevalence of QTc interval prolongation upon admission to the Cardiac Medical Critical Care Unit (CMCCU) or an Advanced Heart Care Unit (AHCU); (ii) proportion of patients admitted to the CMCCU/AHCU with QTc interval prolongation who subsequently were administered QT interval-prolonging drugs during hospitalization; (iii) the proportion of these higher-risk patients in whom TdP risk factor monitoring was performed; (iv) proportion of patients with QTc interval prolongation who subsequently received QT-prolonging drugs and who experienced further QTc interval prolongation.
Results
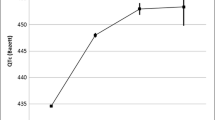
Of 1159 patients enrolled, 259 patients met exclusion criteria, resulting in a final sample size of 900 patients. Patient characteristics: mean (± SD) age, 65 ±15 years; female, 47%; Caucasian, 70%. Admitting diagnoses: heart failure (22%), myocardial infarction (16%), atrial fibrillation (9%), sudden cardiac arrest (3%). QTc interval prolongation was present in 27.9% of patients on admission; 18.2% had QTc interval >500ms. Of 251 patients admitted with QTc interval prolongation, 87 (34.7%) were subsequently administered QT interval-prolonging drugs. Of 166 patients admitted with QTc interval >500ms, 70 (42.2%) were subsequently administered QT interval-prolonging drugs; additional QTc interval prolongation ≥60 ms occurred in 57.1% of these patients.
Conclusions
QTc interval prolongation is common among patients admitted to cardiac units. QT interval-prolonging drugs are commonly prescribed to patients presenting with QTc interval prolongation.







Similar content being viewed by others
References
Gupta A, Lawrence AT, Krishnan K, et al. Current concepts in the mechanisms and management of drug-induced QT prolongation and torsade de pointes. Am Heart J 2007; 153(6): 891–9
Bauman JL, Bauernfeind RA, Hoff JV, et al. Torsade de pointes due to quinidine: observations in 31 patients. Am Heart J 1984; 107: 425–30
Tisdale JE. Ventricular arrhythmias. In: Tisdale JE, Miller DA, editors. Drug-induced diseases: prevention, detection and management, 2nd ed. Bethesda (MD): American Society of Health-System Pharmacists, 2010: 485–515
Drew BJ, Ackerman MJ, Funk M, et al., On behalf of the American Heart Association Acute Cardiac Care Committee of the Council on Clinical Cardiology, the Council on Cardiovascular Nursing, and the American College of Cardiology Foundation. Prevention of torsade de pointes in hospital settings: a scientific statement from the American Heart Association and the American College of Cardiology Foundation. Circulation 2010; 121(8): 1047–60
Bazett HC. An analysis of time relationships of the electrocardiogram. Heart 1920; 7: 353–70
Roden DM, Woosley RL, Primm RK. Incidence and clinical features of the quinidine-associated long QT syndrome: implications for patient care. Am Heart J 1986; 111(6): 1088–93
Woosley RL, Chen Y, Freiman JP, et al. Mechanism of the cardiotoxic actions of terfenadine. JAMA 1993; 269(12): 1532–6
De Bruin ML, Langendijk PN, Koopmans RP, et al. Inhospital cardiac arrest is associated with use of nonantiarrhythmic QTc-prolonging drugs. Br J Clin Pharmacol 2007; 63(2): 216–23
Surawicz B, Childers R, Deal BJ, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram, part III: intraventricular conduction disturbances: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Circulation 2009; 119(10): e235–40
Lubart E, Segal R, Yearovoi A, et al. QT interval disturbances in hospitalized elderly patients. Isr Med Assoc J 2009; 11(3): 147–50
Dumontet J, Malyuk R, Kiang G, et al. Corrected QT intervals in newly admitted geriatric psychiatric patients: an examination of risk factors. Can J Psychiatry 2006; 51(6): 371–6
Seftchick MW, Adler PH, Hsieh M, et al. The prevalence and factors associated with QTc prolongation among emergency department patients. Ann Emerg Med 2009; 54(6): 763–8
Golazari GH, Dawson NV, Speroff T, et al. Prolonged QTc intervals on admission electrocardiograms: prevalence and correspondence with admission electrolyte abnormalities. Conn Med 2007; 71(7): 389–97
Pasquier M, Pantet O, Hugli O, et al. Prevalence and determinants of QT interval prolongation in medical inpatients. Intern Med J. Epub 2011 Feb 8
Darpö B. Spectrum of drugs prolonging QT interval and the incidence of torsades de pointes. Eur Heart J Suppl 2001; 3 Suppl. K: K70–80
Hodges M. Rate correction of the QT interval. Card Electrophysiol Rev 1997; 1: 360–3
Chiladakis J, Kalogeropoulos A, Arvanitis P, et al. Preferred QT correction formula for the assessment of drug-induced QT interval prolongation. J Cardiovasc Electrophysiol 2010; 21: 905–13
Drew BJ, Califf RM, Funk M, et al. Practice standards for electrocardiographic monitoring in hospital settings: an American Heart Association scientific statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Young. Circulation 2004; 110(17): 2721–46
Acknowledgements
This work was supported in part by a grant from the Lilly Endowment, Inc., to the Purdue University College of Pharmacy, and by National Institutes of Health grant [K08 HL095655] (Dr Overholser).
The funding organizations had no role in the design and conduct of the study, collection, management, analysis and interpretation of data, or preparation, review or approval of the manuscript.
Dr Kovacs has served as an advisor to Eli Lilly & Co., Essentialis, Xenoport, Inc., and Synosia Therapeutics regarding issues related to the QT interval in drug development. All other authors have no conflicts of interest to declare.
Presented at the 59th Annual Scientific Sessions of the American College of Cardiology, 15 March 2010.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tisdale, J.E., Wroblewski, H.A., Overholser, B.R. et al. Prevalence of QT Interval Prolongation in Patients Admitted to Cardiac Care Units and Frequency of Subsequent Administration of QT Interval-Prolonging Drugs. Drug Saf 35, 459–470 (2012). https://doi.org/10.2165/11598160-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11598160-000000000-00000