Abstract
Background: The continuous erythropoietin receptor activator (C.E.R.A.) has a long half-life, a relatively low binding affinity for the erythropoiesis receptor and low systemic clearance. These characteristics permit once-monthly dosing, which could reduce staffing requirements and be advantageous for patients. However, outcomes observed during controlled trials of C.E.R.A. have not been assessed under everyday clinical conditions in which physicians make all therapeutic decisions based on their own experience, rather than according to a pre-defined protocol.
Objective: This study aimed to assess whether the efficacy and safety of C.E.R.A. reported during controlled trials are reproducible under routine clinical conditions.
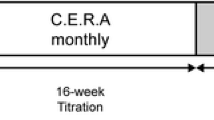
Methods: This was a non-interventional, single-cohort, multicentre study carried out in 92 specialist nephrology clinics and private practices in Germany. The study included patients with non-dialysis chronic kidney disease and anaemia, with or without current erythropoiesis stimulating agent (ESA) therapy. C.E.R.A. initiation and dosing was at the discretion of the physician. The primary efficacy variable was the proportion of patients for whom all measured haemoglobin (Hb) values during months 7–9 were within the range 11–12g/dL (‘responders’).
Results: 335 patients received ≥1 dose of C.E.R.A.; 150 had previously received ESA therapy. The mean number of doses was 7.6 per patient over a mean follow-up of 7.9 months. Mean ± SD Hb was 10.7 ± 1.1 g/dL at baseline and 11.3 ± 1.1 g/dL at the final visit (efficacy population, n = 205). The primary endpoint, all measured Hb values during months 7–9 within the range 11–12 g/dL, was achieved by 19.0% (39/205) of patients, increasing to 41.5% for Hb 11–13 g/dL, 42.0% for 10–12 g/dL and 76.6% for Hb ≥10g/dL. Hb fluctuation during months 7–9 was ≤1 g/dL in 185/205 patients (90.2%). C.E.R.A. was well tolerated without novel safety concerns.
Conclusion: Hb levels remained stable during routine use of C.E.R.A. in an unselected population of non-dialysis chronic kidney disease patients with anaemia. C.E.R.A. was administered approximately monthly compared with 3–7 doses per month on previous ESA therapy.






Similar content being viewed by others
References
McClellan W, Aronoff SL, Bolton WK, et al. The prevalence of anemia in patients with chronic kidney disease. Curr Med Res Opin 2004; 20(9): 1501–10
Valderrábano F, Hörl WH, Macdougall IC, et al. PREdialysis survey on anaemia management. Nephrol Dial Transplant 2003; 18(1): 89–100
Finkelstein FO, Story K, Firanek C, et al. Health-related quality of life and hemoglobin levels in chronic kidney disease patients. Clin J Am Soc Nephrol 2009; 4(1): 33–8
Fishbane S. Anemia and cardiovascular risk in the patient with kidney disease. Heart Fail Clin 2008; 4(4): 401–10
Kovesdy CP, Trivedi BK, Kalantar-Zadeh K, et al. Association of anemia with outcomes in men with moderate and severe chronic kidney disease. Kidney Int 2006; 69(3): 560–4
Locatelli F, Pisoni RL, Combe C, et al. Anaemia in haemodialysis patients of five European countries: association with morbidity and mortality in the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol Dial Transplant 2004; 19(1): 121–32
KDOQI. Clinical practice guideline and clinical practice recommendations for anemia in chronic kidney disease, 2007 update of hemoglobin target. Am J Kidney Dis 2007; 50(3): 471–30
Locatelli F, Covic A, Eckardt KU, et al. ERA-EDTA ERBP Advisory Board Anaemia management in patients with chronic kidney disease: a position statement by the Anaemia Working Group of European Renal Best Practice (ERBP). Nephrol Dial Transplant 2009; 24(2): 348–54
Locatelli F, Covic A, Macdougall IC, et al., ORAMA Study Group. ORAMA: a study to investigate EBPG impact on renal anaemia. Design and baseline data. J Nephrol 2008; 21(4): 592–603
Handelman GJ, Levin NW. Iron and anemia in human biology: a review of mechanisms. Heart Fail Rev 2008; 13(4): 393–404
Fishbane S, Berns JS. Hemoglobin cycling in hemodialysis patients treated with recombinant human erythropoietin. Kidney Int 2005; 68(3): 1337–43
Yang W, Israni RK, Brunelli SM, et al. Hemoglobin variability and mortality in ESRD. J Am Soc Nephrol 2007; 18(12): 3164–70
Rossert J, Gassmann-Mayer C, Frei D, et al. Prevalence and predictors of epoetin hyporesponsiveness in chronic kidney disease patients. Nephrol Dial Transplant 2007; 22(3): 794–800
De Cock E, Van Bellinghen L, Standaert B. Assessing provider time for anaemia management of dialysis patients using time and motion methods: a multi-centre observational study in Europe [abstract]. Value Health 2002; 5: 581
Wish JB, Coyne DW. Use of erythropoiesis-stimulating agents in patients with anemia of chronic kidney disease: overcoming the pharmacological and pharmacoeconomic limitations of existing therapies. Mayo Clin Proc 2007; 82(11): 1371–80
Macdougall IC, Robson R, Opatrna S, et al. Pharmaco-kinetics and pharmacodynamics of intravenous and subcutaneous continuous erythropoietin receptor activator (C.E.R.A.) in patients with chronic kidney disease. Clin J Am Soc Nephrol 2006; 1(6): 1211–5
Locatelli F, Villa G, de Francisco ALM, et al., BA16286 study investigators. Effect of a continuous erythropoietin receptor activator (C.E.R.A.) on stable haemoglobin in patients with CKD on dialysis: once monthly administration. Curr Med Res Opin 2007; 23(5): 969–79
Levin NW, Fishbane S, Cañedo FV, et al., MAXIMA Study Investigators. Intravenous methoxy polyethylene glycolepoetin beta for haemoglobin control in patients with chronic kidney disease who are on dialysis: a randomised non-inferiority trial (MAXIMA). Lancet 2007; 370(9596): 1415–21
Sulowicz W, Locatelli F, Ryckelynck JP, et al., PROTOS Study Investigators. Once-monthly subcutaneous C.E.R.A. maintains stable hemoglobin control in patients with chronic kidney disease on dialysis converted directly from epoetin one to three times weekly. Clin J Am Soc Nephrol 2007; 2(4): 637–46
Roger SD, Locatelli F, Woitas RP, et al. C.E.R.A. once every 4 weeks corrects anaemia and maintains haemoglobin in patients with chronic kidney disease not on dialysis. Nephrol Dial Transplant 2011. Epub ahead of print
Macdougall IC, Walker R, Provenzano R, et al., ARCTOS Study Investigators. C.E.R.A. corrects anemia in patients with chronic kidney disease not on dialysis: results of a randomized clinical trial. Clin J Am Soc Nephrol 2008; 3(2): 337–47
Kessler M, Martinez-Castelao A, Siamopoulos KC, et al. C.E.R.A. once every 4 weeks in patients with chronic disease not on dialysis: the ARCTOS extension study. Hemodial Int 2010; 14(2): 233–9
Drueke TB, Locatelli F, Clyne N, et al., CREATE Investigators. Normalization of hemoglobin level in patients with chronic kidney disease and anemia. N Eng J Med 2006; 335(20): 2071–84
Singh AK, Szczech L, Tang KL, et al., CHOIR Investigators. Correction of anemia with epoetin alfa in chronic kidney disease. N Eng J Med 2006; 335(20): 2085–98
Hörl WH. A need for an individualized approach to endstage renal disease patients. Nephrol Dial Transplant 2002; 17Suppl. 6: 17–21
Locatelli F, Aljama P, Canaud B, et al., Anaemia Working Group of European Renal Best Practice (ERBP). Target haemoglobin to aim for with erythropoiesis-stimulating agents: a position statement by ERBP following publication of the trial to reduce cardiovascular events with Aranesp therapy (TREAT) study. Nephrol Dial Transplant 2010; 25(9): 2846–50
Macdougall IC. Individualizing target haemoglobin concentrations: tailoring treatment for renal anaemia. Nephrol Dial Transplant 2001; 6Suppl. 7: 9–14
Klinger M, Arias M, Vargemezis V, et al. Efficacy of intravenous methoxy polyethylene glycol-epoetin beta administered every 2 weeks compared with epoetin administered 3 times weekly in patients treated by hemodialysis or peritoneal dialysis: a randomized trial. Am J Kidney Dis 2007; 50(6): 989–1000
Spinowitz B, Coyne DW, Lok CE, et al., RUBRA Study Investigators. C.E.R.A. maintains stable control of hemoglobin in patients with chronic kidney disease on dialysis when administered once every two weeks. Am J Nephrology 2008; 28(2): 280–9
Canaud B, Mingardi G, Braun J, et al., STRIATA Study Investigators. Intravenous C.E.R.A. maintains stable haemoglobin levels in patients on dialysis previously treated with darbepoetin alfa: results from STRIATA, a randomized phase III study. Nephrol Dial Transplant 2008; 23(11): 3654–61
Nissenson AR, Swan SK, Lindberg JS, et al. Randomized, controlled trial of darbepoetin alfa for the treatment of anemia in hemodialysis patients. Am J Kidney Dis 2002; 40(1): 110–8
Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron 1976; 16(1): 31–41
Eckardt KU, Berns JS, Rocco MV, et al. Definition and classification of CKD: the debate should be about patient prognosis. A position statement from KDOQI and KDIGO. Am J Kidney Dis 2009; 53(6): 915–20
Berns JS, Elzein H, Lynn RI, et al. Hemoglobin variability in epoetin treated hemodialysis patients. Kidney Int 2003; 64(4): 1514–21
Hörl WH. Non-erythropoietin-based anaemia management in chronic kidney disease. Nephrol Dial Transplant 2002; 17Suppl. 11: 35–8
Acknowledgements
The study was sponsored by Roche Pharma AG, Grenzach-Wyhlen, Germany. The sponsor contributed to the study design but was not involved in data collection, and reviewed the manuscript. Stefan Heidenreich has received lecture honoraria from Roche Pharma AG. Other than participation in the current study, no other author has any conflict of interest to declare. No other person made a substantial contribution to the work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Heidenreich, S., Leistikow, F., Zinn, S. et al. Monthly Administration of a Continuous Erythropoietin Receptor Activator Provides Efficient Haemoglobin Control in Non-Dialysis Patients during Routine Clinical Practice. Clin Drug Investig 32, 99–110 (2012). https://doi.org/10.2165/11594040-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11594040-000000000-00000