Abstract
Arising in settings of CNS insult, pseudobulbar affect (PBA) consists of uncontrollable episodes of crying or laughter incongruent to the patient’s mood. The syndrome has been described by a plethora of names, including pathological laughing and crying, emotional lability, emotionalism and emotional incontinence, which hampers efforts to survey published assessments of pharmacological intervention. Still, until quite recently, all treatment has unavoidably been off-label, chiefly involving antidepressants. Using PBA and other syndrome names as search terms, a PubMed search for English-language case reports and therapeutic trials involving at least five patients identified 22 such publications from 1980 through to 2010. Among the seven randomized, double-blind, antidepressant studies with placebo control, two trials assessed 106 and 123 subjects, respectively. However, the other five assessed only 12–28 subjects, and only one of these seven trials (with 28 subjects) measured change in syndrome severity using a validated scale. The three randomized, double-blind studies of dextromethorphan plus quinidine assessed 129, 150 and 326 subjects. Among these studies, two were placebo-controlled and all three used a validated severity scale. Across all placebo-controlled trials, response to active treatment — either an antidepressant or dextromethorphan/quinidine — has in general been significantly greater than response to placebo, but placebo response has sometimes been substantial, suggesting caution in interpreting uncontrolled findings. In October 2010, dextromethorphan/quinidine received approval from the US FDA as first-in-class PBA pharmacotherapy. Advocates of a continuing role for antidepressants, notably selective serotonin reuptake inhibitors, can point to numerous positive case reports and trials, the potential benefit of attempting to treat PBA and concomitant depression without using multiple drugs, and the ever-present need to tailor treatment to the individual patient.


Similar content being viewed by others
References
Schiffer R, Pope LE. Review of pseudobulbar affect including a novel and potential therapy. J Neuropsychiatry Clin Neurosci 2005 Fall; 17(4): 447–54
Parvizi J, Arciniegas DB, Bernardini GL, et al. Diagnosis and management of pathological laughter and crying. Mayo Clin Proc 2006 Nov; 81(11): 1482–6
House A, Dennis M, Molyneux A, et al. Emotionalism after stroke. BMJ 1989 Apr 15; 298(6679): 991–4
Brooks N. Personality change after severe head injury. Acta Neurochir Suppl (Wien) 1988; 44: 59–64
Starkstein SE, Migliorelli R, Teson A, et al. Prevalence and clinical correlates of pathological affective display in Alzheimer’s disease. J Neurol Neurosurg Psychiatry 1995 Jul; 59(1): 55–60
Miller RG, Jackson CE, Kasarskis EJ, et al. Practice parameter update: the care of the patient with amyotrophic lateral sclerosis: multidisciplinary care, symptom management, and cognitive/behavioral impairment (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2009 Oct 13; 73(15): 1227–33
Feinstein A, Feinstein K, Gray T, et al. Prevalence and neurobehavioral correlates of pathological laughing and crying in multiple sclerosis. Arch Neurol 1997 Sep; 54(9): 1116–21
Gallagher JP. Pathologic laughter and crying in ALS: a search for their origin. Acta Neurol Scand 1989 Aug; 80(2): 114–7
Wilson SAK. Some problems in neurology, II: pathological laughing and crying. J Neurol Psychopathol 1924; IV: 299–333
Darwin C. The expression of the emotions in man and animals. New York: D Appelton and Company, 1872
Lawson IR, MacLeod RD. The use of imipramine (‘Tofranil’) and other psychotropic drugs in organic emotionalism. Br J Psychiatry 1969 Mar; 115(520): 281–5
Wolf JK, Santana HB, Thorpy M. Treatment of ‘emotional incontinence’ with levodopa. Neurology 1979 Oct; 29(10): 1435–6
Udaka F, Yamao S, Nagata H, et al. Pathologic laughing and crying treated with levodopa. Arch Neurol 1984 Oct; 41(10): 1095–6
Brooks BR, Thisted RA, Appel SH, et al. Treatment of pseudobulbar affect in ALS with dextromethorphan/quinidine: a randomized trial. Neurology 2004 Oct 26; 63(8): 1364–70
Pioro EP, Brooks BR, Cummings J, et al. Dextromethorphan plus ultra low-dose quinidine reduces pseudobulbar affect. Ann Neurol 2010 Nov; 68(5): 693–702
Panitch HS, Thisted RA, Smith RA, et al. Randomized, controlled trial of dextromethorphan/quinidine for pseudobulbar affect in multiple sclerosis. Ann Neurol 2006 May; 59(5): 780–7
Cummings JL, Arciniegas DB, Brooks BR, et al. Defining and diagnosing involuntary emotional expression disorder. CNS Spectr 2006 Jun; 11(6): 1–7
Komurasaki Y, Yokoyama T, Ogura J, et al. Treatment of pathologic emotionality with thyrotropin-releasing hormone. Jpn J Psychiatry Neurol 1989 Dec; 43(4): 665–8
Pringle CE, Hudson AJ, Munoz DG, et al. Primary lateral sclerosis: clinical features, neuropathology and diagnostic criteria. Brain 1992 Apr; 115 (Pt 2): 495–520
Menza MA, Cocchiola J, Golbe LI. Psychiatric symptoms in progressive supranuclear palsy. Psychosomatics 1995 Nov–Dec; 36(6): 550–4
Kim JS. Pathologic laughter after unilateral stroke. J Neurol Sci 1997 May 1; 148(1): 121–5
Nahas Z, Arlinghaus KA, Kotrla KJ, et al. Rapid response of emotional incontinence to selective serotonin reuptake inhibitors. J Neuropsychiatry Clin Neurosci 1998 Fall; 10(4): 453–5
Hargrave DR, Mabbott DJ, Bouffet E. Pathological laughter and behavioural change in childhood pontine glioma. J Neurooncol 2006 May; 77(3): 267–71
Parvizi J, Joseph J, Press DZ, et al. Pathological laughter and crying in patients with multiple system atrophycerebellar type. Mov Disord 2007 Apr 30; 22(6): 798–803
Seliger GM, Hornstein A, Flax J, et al. Fluoxetine improves emotional incontinence. Brain Inj 1992 May–Jun; 6(3): 267–70
Sloan RL, Brown KW, Pentland B. Fluoxetine as a treatment for emotional lability after brain injury. Brain Inj 1992 Jul-Aug; 6(4): 315–9
Iannaccone S, Ferini-Strambi L. Pharmacologic treatment of emotional lability. Clin Neuropharmacol 1996 Dec; 19(6): 532–5
Müller U, Murai T, Bauer-Wittmund T, et al. Paroxetine versus citalopram treatment of pathological crying after brain injury. Brain Inj 1999 Oct; 13(10): 805–11
Schiffer RB, Herndon RM, Rudick RA. Treatment of pathologic laughing and weeping with amitriptyline. N Engl J Med 1985 Jun 6; 312(23): 1480–2
Robinson RG, Parikh RM, Lipsey JR, et al. Pathological laughing and crying following stroke: validation of a measurement scale and a double-blind treatment study. Am J Psychiatry 1993 Feb; 150(2): 286–93
Andersen G, Vestergaard K, Riis JO. Citalopram for poststroke pathological crying. Lancet 1993 Oct 2; 342(8875): 837–9
Brown KW, Sloan RL, Pentland B. Fluoxetine as a treatment for post-stroke emotionalism. Acta Psychiatr Scand 1998 Dec; 98(6): 455–8
Burns A, Russell E, Stratton-Powell H, et al. Sertraline in stroke-associated lability of mood. Int J Geriatr Psychiatry 1999 Aug; 14(8): 681–5
Murray V, von Arbin M, Bartfai A, et al. Double-blind comparison of sertraline and placebo in stroke patients with minor depression and less severe major depression. J Clin Psychiatry 2005 Jun; 66(6): 708–16
Choi-Kwon S, Han SW, Kwon SU, et al. Fluoxetine treatment in poststroke depression, emotional incontinence, and anger proneness: a double-blind, placebo-controlled study. Stroke 2006 Jan; 37(1): 156–61
Moore SR, Gresham LS, Bromberg MB, et al. A self report measure of affective lability. J Neurol Neurosurg Psychiatry 1997 Jul; 63(1): 89–93
Panzer MJ, Mellow AM. Antidepressant treatment of pathologic laughing or crying in elderly stroke patients. J Geriatr Psychiatry Neurol 1992 Oct–Dec; 5(4): 195–9
Tsai WC, Lai JS, Wang TG. Treatment of emotionalism with fluoxetine during rehabilitation. Scand J Rehabil Med 1998 Sep; 30(3): 145–9
Mukand J, Kaplan M, Senno RG, et al. Pathological crying and laughing: treatment with sertraline. Arch Phys Med Rehabil 1996 Dec; 77(12): 1309–11
Okun MS, Riestra AR, Nadeau SE. Treatment of ballism and pseudobulbar affect with sertraline. Arch Neurol 2001 Oct; 58(10): 1682–4
Okun MS, Heilman KM, Vitek JL. Treatment of pseudobulbar laughter after gamma knife thalamotomy. Mov Disord 2002 May; 17(3): 622–4
Derex L, Ostrowsky K, Nighoghossian N, et al. Severe pathological crying after left anterior choroidal artery infarct: reversibility with paroxetine treatment. Stroke 1997 Jul; 28(7): 1464–6
Kosaka H, Omata N, Omori M, et al. Abnormal pontine activation in pathological laughing as shown by functional magnetic resonance imaging. J Neurol Neurosurg Psychiatry 2006 Dec; 77(12): 1376–80
Andersen G, Stylsvig M, Sunde N. Citalopram treatment of traumatic brain damage in a 6-year-old boy. J Neurotrauma 1999 Apr; 16(4): 341–4
Kaschka WP, Meyer A, Schier KR, et al. Treatment of pathological crying with citalopram. Pharmacopsychiatry 2001 Nov; 34(6): 254–8
Allman P. Drug treatment of emotionalism following brain damage. J R Soc Med 1992 Jul; 85(7): 423–4
Parvizi J, Schiffer R. Exaggerated crying and tremor with a cerebellar cyst. J Neuropsychiatry Clin Neurosci 2007 Spring; 19(2): 187–90
Zellers GL, Frank M, Dougherty J. Pathological laughter. Ann Emerg Med 1990 Mar; 19(3): 327–9
Ramasubbu R. Lamotrigine treatment for post-stroke pathological laughing and crying. Clin Neuropharmacol 2003 Sep–Oct; 26(5): 233–5
Kubo T, Kobayashi O, Nozaki M, et al. Successful thyrotropinreleasing hormone therapy for emotional incontinence and amnesia resulting from mumps encephalitis. Pediatr Infect Dis J 2004 Dec; 23(12): 1175–6
Kim SW, Shin IS, Kim JM, et al. Mirtazapine treatment for pathological laughing and crying after stroke. Clin Neuropharmacol 2005 Sep–Oct; 28(5): 249–51
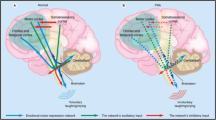
Andersen G, Ingeman-Nielsen M, Vestergaard K, et al. Pathoanatomic correlation between poststroke pathological crying and damage to brain areas involved in serotonergic neurotransmission. Stroke 1994 May; 25(5): 1050–2
Parvizi J, Coburn KL, Shillcutt SD, et al. Neuroanatomy of pathological laughing and crying: a report of the American Neuropsychiatric Association Committee on Research. J Neuropsychiatry Clin Neurosci 2009 Winter; 21: 75–87
Parvizi J, Damasio AR. Neuroanatomical correlates of brainstem coma. Brain 2003 Jul; 126 (Pt 7): 1524–36
McCall RB, Aghajanian GK. Serotonergic facilitation of facial motoneuron excitation. Brain Res 1979 Jun 15; 169(1): 11–27
Moller M, Andersen G, Gjedde A. Serotonin 5HT1A receptor availability and pathological crying after stroke. Acta Neurol Scand 2007 Aug; 116(2): 83–90
Brown JW. Physiology and phylogenesis of emotional expression. Brain Res 1967 May; 5(1): 1–14
Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry 1960 Feb; 23(1): 56–62
Beck AT, Ward CH, Mendelson M, et al. An inventory for measuring depression. Arch Gen Psychiatry 1961 Jun; 4: 561–71
Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry 1979 Apr; 134: 382–9
Choi DW, Peters S, Viseskul V. Dextrorphan and levorphanol selectively block N-methyl-D-aspartate receptormediated neurotoxicity on cortical neurons. J Pharmacol Exp Ther 1987 Aug; 242(2): 713–20
Klein M, Musacchio JM. High affinity dextromethorphan binding sites in guinea pig brain: effect of sigma ligands and other agents. J Pharmacol Exp Ther 1989 Oct; 251(1): 207–15
DeCoster MA, Klette KL, Knight ES, et al. Sigma receptormediated neuroprotection against glutamate toxicity in primary rat neuronal cultures. Brain Res 1995 Feb 6; 671(1): 45–53
Wroblewski JT, Danysz W. Modulation of glutamate receptors: molecular mechanisms and functional implications. Annu Rev Pharmacol Toxicol 1989; 29: 441–74
Askmark H, Aquilonius SM, Gillberg PG, et al. A pilot trial of dextromethorphan in amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry 1993 Feb; 56(2): 197–200
Blin O, Azulay JP, Desnuelle C, et al. A controlled one-year trial of dextromethorphan in amyotrophic lateral sclerosis. Clin Neuropharmacol 1996 Apr; 19(2): 189–92
Vetticaden SJ, Cabana BE, Prasad VK, et al. Phenotypic differences in dextromethorphan metabolism. Pharm Res 1989 Jan; 6(1): 13–9
Zhang Y, Britto MR, Valderhaug KL, et al. Dextromethorphan: enhancing its systemic availability by way of lowdose quinidine-mediated inhibition of cytochrome P4502D 6. Clin Pharmacol Ther 1992 Jun; 51(6): 647–55
Smith RA, Moore S, Gresham L, et al. The treatment of affective lability with dextromethorphan. American Academy of Neurology 47th Annual Meeting [abstract no. 604P]. Neurology 1995; 45 Suppl. 4: A330
Holford NH, Coates PE, Guentert TW, et al. The effect of quinidine and its metabolites on the electrocardiogram and systolic time intervals: concentration-effect relationships. Br J Clin Pharmacol 1981 Feb; 11(2): 187–95
Smith RA, Berg JE, Pope LE, et al. Validation of the CNS emotional lability scale for pseudobulbar affect (pathological laughing and crying) in multiple sclerosis patients. Mult Scler 2004 Dec; 10(6): 679–85
Brooks BR, Cummings J, Pioro EP, et al. Pharmacokinetic/pharmacodynamic modeling of dextromethorphan/quinidine for a study in pseudobulbar affect [abstract T 172]. Presented at the American Neurological Association’s 133rd Annual Meeting; 2008 Sep 21–24; Salt Lake City (UT)
Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio (TX): Psychological Corporation, 1996
Pioro EP, Brooks BR, Cummings J, et al. Persistent efficacy of dextromethorphan/quinidine for pseudobulbar affect: results from a 12-week, open-label extension study [poster P02.295]. Presented at the 62nd Annual Meeting of the American Academy of Neurology; 2010 Apr 10–17; Toronto (ON)
Ware Jr JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992 Jun; 30(6): 473–83
Swinkels JA, de Jonghe F. Safety of antidepressants. Int Clin Psychopharmacol 1995 Jan; 9 Suppl. 4: 19–25
Pollock BG, Mulsant BH, Nebes R, et al. Serum anticholinergicity in elderly depressed patients treated with paroxetine or nortriptyline. Am J Psychiatry 1998 Aug; 155(8): 1110–2
Anderson IM. Selective serotonin reuptake inhibitors versus tricyclic antidepressants: a meta-analysis of efficacy and tolerability. J Affect Disord 2000 Apr; 58(1): 19–36
De Ponti F, Poluzzi E, Montanaro N. QT-interval prolongation by non-cardiac drugs: lessons to be learned from recent experience. Eur J Clin Pharmacol 2000 Apr; 56(1): 1–18
Haiman G, Pratt H, Miller A. Brain responses to verbal stimuli among multiple sclerosis patients with pseudo-bulbar affect. J Neurol Sci 2008 Aug 15; 271(1-2): 137–47
Haiman G, Pratt H, Miller A. Effects of dextromethorphan/quinidine on auditory event-related potentials in multiple sclerosis patients with pseudobulbar affect. J Clin Psychopharmacol 2009 Oct; 29(5): 444–52
Acknowledgements
Preparation of this review was supported by Avanir Pharmaceuticals. Editorial assistance in the form of substantive editing, copy editing and styling was provided by Michael Feirtag of The Curry Rockefeller Group, LLC, Tarrytown, NY. Dr Pioro has received research support and compensation for consulting from Avanir Pharmaceuticals.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pioro, E.P. Current Concepts in the Pharmacotherapy of Pseudobulbar Affect. Drugs 71, 1193–1207 (2011). https://doi.org/10.2165/11591450-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11591450-000000000-00000