Abstract
Patients with β-thalassaemia, sickle cell disease (SCD) and myelodysplastic syndromes (MDS) require chronic blood transfusions, which can lead to iron overload and substantial morbidity and mortality. To reduce the excess iron and its deleterious effects, available iron chelation therapy (ICT) in the US includes oral deferasirox or infusional deferoxamine (DFO). The aim of this study was to review and synthesize the available pharmacoeconomic evidence on ICT in patients with β-thalassaemia, SCD and MDS in the US.
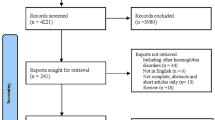
We systematically identified and reviewed pharmacoeconomic studies of ICT in patients with β-thalassaemia, SCD and MDS that either were published in MEDLINE-indexed, English-language journals from 1999 to 2009, or appeared in medical society websites and scientific meeting abstracts. We assessed available cost-of-illness, cost-of-treatment, cost-consequence, cost-effectiveness, utility and patient-satisfaction studies.
The majority of the 20 identified studies assessed cost of treatment, mainly focusing on acquisition and administration costs of ICTs. Gaps in the published literature include current data on direct medical costs for patients with MDS, direct medical costs associated with complications of iron overload, direct non-medical costs, indirect costs and patient utilities. Different underlying model assumptions, methodologies and comparators were found in the cost-effectiveness studies, which yielded a broad range of incremental cost-effectiveness ratios for different ICTs.
Comprehensive cost-of-illness studies are needed to address data gaps in the published literature regarding the economic burden of iron overload. Comparative-effectiveness studies that evaluate clinical, economic and patient-reported outcomes would help the medical community to better understand the value of different ICTs.
Similar content being viewed by others
References
Dipiro J, Talbert R, Yee G, et al. Pharmacotherapy: a pathophysiologic approach. 5th ed. New York: McGraw-Hill Medical, 2002
Cappellini MD, Cohen A, Eleftheriou A, et al. Guidelines for the clinical management of thalassemia. 2nd rev. ed. Nicosia: Thalassemia International Federation, 2010
National Cancer Institute. Myelodysplastic syndromes treatment (PDQ®): general information about myelodysplastic syndromes [online]. Available from URL: http://www.nci.nih.gov/cancertopics/pdq/treatment/myelodysplastic/healthprofessional/ [Accessed 2009 Jul 2]
Exjade® (deferasirox) [package insert]. East Hanover (NJ): Novartis Pharmaceutical Corporation, 2010
Desferal® (deferoxamine) [package insert]. East Hanover (NJ): Novartis Pharmaceutical Corporation, 2008
WHO. Genes and human disease: monogenic diseases [online]. Available from URL: http://www.who.int/genomics/public/geneticdiseases/en/index2.html/ [Accessed 2011 Mar 16]
Cunningham MJ, Nathan DG. New developments in iron chelators. Curr Opin Hematol 2005; 12: 129–34
Borgna-Pignatti C, Rugolotto S, De SP, et al. Survival and complications in patients with thalassemia major treated with transfusion and deferoxamine. Haematologica 2004; 89: 1187–93
Kushner JP, Porter JP, Olivieri NF. Secondary iron overload. Hematology Am Soc Hematol Educ Program 2001; 47–61
Wayne AS, Kevy SV, Nathan DG. Transfusion management of sickle cell disease. Blood 1993; 81: 1109–23
Hofmann WK, Koeffler HP. Myelodysplastic syndrome. Annu Rev Med 2005; 56: 1–16
Malcovati L, Porta MG, Pascutto C, et al. Prognostic factors and life expectancy in myelodysplastic syndromes classified according to WHO criteria: a basis for clinical decision making. J Clin Oncol 2005; 23: 7594–603
Fung EB, Harmatz P, Milet M, et al. Morbidity and mortality in chronically transfused subjects with thalassemia and sickle cell disease: a report from the multi-center study of iron overload. Am J Hematol 2007; 82: 255–65
Vichinsky E, Butensky E, Fung E, et al. Comparison of organ dysfunction in transfused patients with SCD or beta thalassemia. Am J Hematol 2005; 80: 70–4
Delea TE, Hagiwara M, Phatak PD. Retrospective study of the association between transfusion frequency and potential complications of iron overload in patients with myelodysplastic syndrome and other acquired hematopoietic disorders. Curr Med Res Opin 2009; 25: 139–47
US Bureau of Labor Statistics. Medical care component of consumer price index, 2009 [online]. Available from URL: http://www.bls.gov/cpi/cpid09av.pdf[Accessed 2011 Mar 16]
Delea TE, Thomas SK, Baladi JF, et al. Utilization and costs of deferoxamine in patients with thalassemia, sickle cell disease, or myelodysplastic syndrome receiving transfusions [abstract no. 5583]. 47th American Society of Hematology Annual Meeting and Exposition; 2005 Dec 10–13; Atlanta (GA)
Delea TE, Hagiwara M, Thomas SK, et al. Outcomes, utilization, and costs among thalassemia and sickle cell disease patients receiving deferoxamine therapy in the United States. Am J Hematol 2008; 83: 263–70
Renfroe LJ, Forbes P, Braunstein J, et al. Relationship of transfusion and iron-related complications to cost of care in thalassemia [abstract no. 2240]. 47th American Society of Hematology Annual Meeting and Exposition; 2005 Dec 10–13; Atlanta (GA)
Wayne AS, Schoenike SE, Pegelow CH. Financial analysis of chronic transfusion for stroke prevention in sickle cell disease. Blood 2000; 96: 2369–72
Payne KA, Desrosiers MP, Caro JJ, et al. Clinical and economic burden of infused iron chelation therapy in the United States. Transfusion 2007; 47: 1820–9
Greenberg PL, Cosler LE, Ferro SA, et al. The costs of drugs used to treat myelodysplastic syndromes following National Comprehensive Cancer Network Guidelines. J Natl Compr Canc Netw 2008; 6 (9): 942–53
Cappellini MD, Bejaoui M, Agaoglu L, et al. Prospective evaluation of patient-reported outcomes during treatment with deferasirox or deferoxamine for iron overload in patients with beta-thalassemia. Clin Ther 2007; 29: 909–17
Scalone L, Mantovani LG, Krol M, et al. Costs, quality of life, treatment satisfaction and compliance in patients with beta-thalassemia major undergoing iron chelation therapy: the ITHACA study. Curr Med Res Opin 2008; 24: 1905–17
Vichinsky E, Pakbaz Z, Onyekwere O, et al. Patient-reported outcomes of deferasirox (Exjade, ICL670) versus deferoxamine in sickle cell disease patients with transfusional hemosiderosis: substudy of a randomized open-label phase II trial. Acta Haematol 2008; 119: 133–41
Delea T, Sofrygin O, Thomas S, et al. Cost-effectiveness of once-daily oral therapy with deferasirox in transfusion-dependent thalassemic patients [abstract no. 1341]. 47th American Society of Hematology Annual Meeting and Exposition; 2005 Dec 10–13; Atlanta (GA)
Delea TE, Sofrygin O, Thomas SK, et al. Costs and consequences of inadequate compliance with deferoxamine therapy in patients with transfusion-dependent thalassemia [abstract no. 7637]. ISPOR 11th Annual International Meeting; 2006 May 20–24; Philadelphia (PA)
Delea TE, Sofrygin O, Thomas SK, et al. Cost effectiveness of once-daily oral chelation therapy with deferasirox versus infusional deferoxamine in transfusion-dependent thalassaemia patients: US healthcare system perspective. Pharmacoeconomics 2007; 25 (4): 329–42
Delea T, Sofrygin O, Baladi JF, et al. Chelation therapy with deferasirox versus deferoxamine in transfusion-dependent sickle-cell disease: a cost effectiveness analysis from the US perspective. 11th Congress of the European Hematology Association; 2006 Jun 15–18; Amsterdam
Migliaccio-Walle K, Baladi JF. Economic implications of iron chelation in patients with refractory anemia related to myelodysplastic syndrome [abstract no. 18118]. ISPOR 11th Annual European Congress; 2008 Nov 8–11; Athens
Delea T, Baladi JF, Thomas S, et al. Cost-effectiveness of chelation therapy with deferasirox versus deferoxamine in transfusion-dependent myelodysplastic syndrome. 11th Congress of the European Hematology Association; 2006 Jun 15–18; Amsterdam
Bozkaya D, Migliaccio-Walle K, Baladi JF. Impact of management of iron overload in patients with myelodysplastic syndromes [abstract no. 1308]. 50th Annual American Society of Hematology; 2008 Dec 6–9; San Francisco (CA)
Hirth RA, Chernew ME, Miller E. Willingness to pay for a quality adjusted life year: in search of a standard. Med Decis Making 2000; 20: 332–42
Ubel PA, Hirth RA, Chernew ME. What is the price of life and why doesn’t it increase at the rate of inflation? Arch Int Med 2003; 163: 1637–41
McLeod C, Fleeman N, Kirkham J, et al. Deferasirox for the treatment of iron overload associated with regular blood transfusions (transfusional haemosiderosis) in patients suffering with chronic anaemia: a systematic review and economic evaluation. Health Technol Assess 2009; 13: iii–xi, 1
Tolley K, Oyee J, Knight H, et al. UK community-derived utilities using time trade-off for oral versus subcutaneous iron chelation therapy for the treatment of chronic iron overload [abstract no. 14941]. ISPOR 10th Annual European Congress; 2007 Oct 20–23; Dublin
Osborne RH, De Abreu Lourenco R, Dalton A, et al. Quality of life related to oral versus subcutaneous iron chelation: a time trade-off study. Value Health 2007; 10: 451–6
Payne KA, Rofail D, Baladi JF, et al. Iron chelation therapy: clinical effectiveness, economic burden and quality of life in patients with iron overload. Adv Ther 2008; 25: 725–42
Telfer PT, Prestcott E, Holden S, et al. Hepatic iron concentration combined with longterm monitoring of serum ferritin to predict complications of iron overload in thalassaemia major. Br J Haematol 2000; 110: 971–7
Kim J, Kim Y. Economic evaluation of oral deferasirox versus infusional deferoxamine [abstract no. 17525]. ISPOR 3rd Asia Pacific Congress; 2008 Sep 7–9; Seoul
Ladis V, Chouliaras G, Berfousi H, et al. Longitudinal study of survival and causes of death in patients with thalassemia major in Greece. Ann N Y Acad Sci 2005; 1054: 445–50
Taher A, Cappellini MD. Update on the use of deferasirox in the management of iron overload. Ther Clin Risk Manag 2009; 5: 857–68
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, B., Donga, P.Z., Corral, M. et al. Pharmacoeconomic Considerations in Treating Iron Overload in Patients with β-Thalassaemia, Sickle Cell Disease and Myelodysplastic Syndromes in the US. Pharmacoeconomics 29, 461–474 (2011). https://doi.org/10.2165/11589250-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11589250-000000000-00000