Abstract
Chronic heart failure (CHF) is a critical public health issue with increasing effect on the healthcare budgets of developed countries. Various decisionanalytic modelling approaches exist to estimate the cost effectiveness of health technologies for CHF. We sought to systematically identify these models and describe their structures.
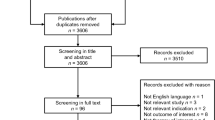
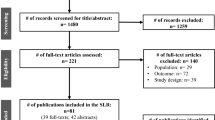
We performed a systematic literature review in MEDLINE/PreMEDLINE, EMBASE, EconLit and the Cost-Effectiveness Analysis Registry using a combination of search terms for CHF and decision-analytic models. The inclusion criterion required ‘use of a mathematical model evaluating both costs and health consequences for CHF management strategies’. Studies that were only economic evaluations alongside a clinical trial or that were purely descriptive studies were excluded.
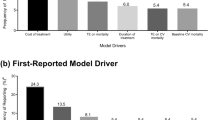
We identified 34 modelling studies investigating different interventions including screening (n = 1), diagnostics (n = 1), pharmaceuticals (n = 15), devices (n = 13), disease management programmes (n = 3) and cardiac transplantation (n = 1) in CHF. The identified models primarily focused on middle-aged to elderly patients with stable but progressed heart failure with systolic left ventricular dysfunction. Modelling approaches varied substantially and included 27 Markov models, three discrete-event simulation models and four mathematical equation sets models; 19 studies reported QALYs. Three models were externally validated. In addition to a detailed description of study characteristics, the model structure and output, the manuscript also contains a synthesis and critical appraisal for each of the modelling approaches.
Well designed decision models are available for the evaluation of different CHF health technologies. Most models depend on New York Heart Association (NYHA) classes or number of hospitalizations as proxy for disease severity and progression. As the diagnostics and biomarkers evolve, there is the hope for better intermediate endpoints for modelling disease progression as those that are currently in use all have limitations.



Similar content being viewed by others
References
McFate SW. Epidemiology of congestive heart failure. Am J Cardiol 1985; 55 Suppl. A: 3–8
Cleland JG. Health economic consequences of the pharmacological treatment of heart failure. Eur Heart J 1998; 19 Suppl. P: P32–9
Berry C, Murdoch DR, McMurray JJ. Economics of chronic heart failure. Eur J Heart Fail 2001; 3 (3): 283–91
Gold MR. Cost-effectiveness in health and medicine. New York: Oxford University Press, 1996
Drummond MF, McGuire A. Economic evaluation in health care: merging theory with practice. New York: Oxford University Press, 2001
Siebert U. When should decision-analytic modeling be used in the economic evaluation of health care? Eur J Health Econ 2003; 4 (3): 143–50
Cost-effectiveness Analysis Registry [online]. Available from URL: https://research.tufts-nemc.org/cear4/default.aspx [Accessed 2007 May 29]
Weinstein MC, O’Brien B, Hornberger J, et al. Principles of good practice for decision analytic modeling in health-care evaluation: report of the ISPOR Task Force on Good Research Practices — Modeling Studies. Value Health 2003; 6 (1): 9–17
Owens DK, Sanders GD, Harris RA, et al. Cost-effectiveness of implantable cardioverter defibrillators relative to amiodarone for prevention of sudden cardiac death. Ann Intern Med 1997; 126 (1): 1–12
Owens DK, Sanders GD, Heidenreich PA, et al. Effect of risk stratification on cost-effectiveness of the implantable cardioverter defibrillator. Am Heart J 2002; 144 (3): 440–8
Anderson AN, Moodley I, Kropman K. A South African pharmaco-economic analysis of theAcute lnfarction Ramipril Efficacy (AIRE) Study. Cardiovasc J S Afr 2000; 11 (2): 89–94
Carroll CA, Coen MM, Piepho RW. Economic impact of ramipril on hospitalization of high-risk cardiovascular patients. Ann Pharmacother 2003; 37 (3): 327–31
Sanders GD, Hlatky MA, Every NR, et al. Potential cost-effectiveness of prophylactic use of the implantable cardioverter defibrillator or amiodarone after myocardial infarction. Ann Intern Med 2001; 135 (10): 870–83
Weintraub WS, Zhang Z, Mahoney EM, et al. Cost-effectiveness of eplerenone compared with placebo in patients with myocardial infarction complicated by left ventricular dysfunction and heart failure. Circulation 2005; 111 (9): 1106–13
Angus DC, Linde-Zwirble WT, Tam SW, et al. Costeffectiveness of fixed-dose combination of isosorbide dinitrate and hydralazine therapy for blacks with heart failure. Circulation 2005; 112 (24): 3745–53
Calvert MJ, Freemantle N, Yao G, et al. Cost-effectiveness of cardiac resynchronization therapy: results from the CARE-HF trial. Eur Heart J 2005; 26 (24): 2681–8
Capomolla S, Febo O, Ceresa M, et al. Cost/utility ratio in chronic heart failure: comparison between heart failure management program delivered by day-hospital and usual care. J Am Coll Cardiol 2002; 40 (7): 1259–66
Schadlich PK, Huppertz E, Brecht JG. Cost-effectiveness analysis of ramipril in heart failure after myocardial infarction: economic evaluation of the Acute Infarction Ramipril Efficacy (AIRE) study for Germany from the perspective of Statutory Health Insurance. Pharmacoeconomics 1998; 14 (6): 653–69
van Hout BA, Wielink G, Bonsel GJ, et al. Effects of ACE inhibitors on heart failure in the Netherlands: a pharmacoeconomic model. Pharmacoeconomics 1993; 3 (5): 387–97
Paul SD, Kuntz KM, Eagle KA, et al. Costs and effectiveness of angiotensin converting enzyme inhibition in patients with congestive heart failure. Arch Intern Med 1994; 154 (10): 1143–9
Glick H, Cook J, Kinosian B, et al. Costs and effects of enalapril therapy in patients with symptomatic heart failure: an economic analysis of the Studies of Left Ventricular Dysfunction (SOLVD) Treatment Trial. J Card Fail 1995; 1 (5): 371–80
Cook JR, Glick HA, Gerth W, et al. The cost and cardioprotective effects of enalapril in hypertensive patients with left ventricular dysfunction. Am J Hypertens 1998; 11 (12): 1433–41
Delea TE, Vera-Llonch M, Richner RE, et al. Cost effectiveness of carvedilol for heart failure. Am J Cardiol 1999; 83 (6): 890–6
Gregory D, Udelson JE, Konstam MA. Economic impact of beta blockade in heart failure. Am J Med 2001; 110 Suppl. 7A: 74S–80S
Varney S. A cost-effectiveness analysis of bisoprolol for heart failure. Eur J Heart Fail 2001; 3 (3): 365–71
Levy AR, Briggs AH, Demers C, et al. Cost-effectiveness of beta-blocker therapy with metoprolol or with carvedilol for treatment of heart failure in Canada. Am Heart J 2001; 142 (3): 537–43
Glick HA, Orzol SM, Tooley JF, et al. Economic evaluation of the randomized aldactone evaluation study (RALES): treatment of patients with severe heart failure. Cardiovasc Drugs Ther 2002; 16 (1): 53–9
Barry M. Cost effectiveness of beta blocker therapy for patients with chronic severe heart failure in Ireland. Ir Med J 2002; 95 (6): 174, 176–7
Tilson L, McGowan B, Ryan M, et al. Cost-effectiveness of spironolactone in patients with severe heart failure. Ir J Med Sci 2003; 172 (2): 70–2
Inomata T, Izumi T, Kobayashi M. Cost-effectiveness analysis of carvedilol for the treatment of chronic heart failure in Japan. Circ J 2004; 68 (1): 35–40
Cowper PA, DeLong ER, Whellan DJ, et al. Economic effects of beta-blocker therapy in patients with heart failure. Am J Med 2004; 116 (2): 104–11
Chen L, Hay JW. Cost-effectiveness of primary implanted cardioverter defibrillator for sudden death prevention in congestive heart failure. Cardiovasc Drugs Ther 2004; 18 (2): 161–70
Heidenreich PA, Gubens MA, Fonarow GC, et al. Costeffectiveness of screening with B-type natriuretic peptide to identify patients with reduced left ventricular ejection fraction. J Am Coll Cardiol 2004; 43 (6): 1019–26
Morimoto T, Hayashino Y, Shimbo T, et al. Is B-type natriuretic peptide-guided heart failure management cost-effective? Int J Cardiol 2004; 96 (2): 177–81
Nichol G, Kaul P, Huszti E, et al. Cost-effectiveness of cardiac resynchronization therapy in patients with symptomatic heart failure. Ann Intern Med 2004; 141 (5): 343–51
Banz K. Cardiac resynchronization therapy (CRT) in heart failure: a model to assess the economic value of this new medical technology. Value Health 2005; 8 (2): 128–39
Sanders GD, Hlatky MA, Owens DK. Cost-effectiveness of implantable cardioverter-defibrillators. N Engl J Med 2005; 353 (14): 1471–80
Caro JJ, Migliaccio-Walle K, O’Brien JA, et al. Economic implications of extended-release metoprolol succinate for heart failure in the MERIT-HF trial: a US perspective of the MERIT-HF trial. J Card Fail 2005; 11 (9): 647–56
Clegg AJ, Scott DA, Loveman E, et al. The clinical and costeffectiveness of left ventricular assist devices for end-stage heart failure: a systematic review and economic evaluation. Health Technol Assess 2005; 9 (45): 1–132, iii-iv
Caro JJ, Guo S, Ward A, et al. Modelling the economic and health consequences of cardiac resynchronization therapy in the UK. Curr Med Res Opin 2006; 22 (6): 1171–9
Freudenberger RS, Kim J, Tawfik I, et al. Optimal medical therapy is superior to transplantation for the treatment of class I, II, and III heart failure: a decision analytic approach. Circulation 2006; 114 (1 Suppl.): I62–6
Mark DB, Nelson CL, Anstrom KJ, et al. Cost-effectiveness of defibrillator therapy or amiodarone in chronic stable heart failure: results from the Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT). Circulation 2006; 114 (2): 135–42
Caro JJ, Ward A, Deniz HB, et al. Cost-benefit analysis of preventing sudden cardiac deaths with an implantable cardioverter defibrillator versus amiodarone. Value Health 2007; 10 (1): 13–22
Yao G, Freemantle N, Calvert MJ, et al. The long-term costeffectiveness of cardiac resynchronization therapy with or without an implantable cardioverter-defibrillator. Eur Heart J 2007; 28 (1): 42–51
Girling AJ, Freeman G, Gordon JP, et al. Modeling payback from research into the efficacy of left-ventricular assist devices as destination therapy. Int J Technol Assess Health Care 2007; 23 (2): 269–77
Fox M, Mealing S, Anderson R, et al. The clinical effectiveness and cost-effectiveness of cardiac resynchronisation (biventricular pacing) for heart failure: systematic review and economic model. Health Technol Assess 2007; 11 (47): iii-iv, ix–248
Chan DC, Heidenreich PA, Weinstein MC, et al. Heart failure disease management programs: a cost-effectiveness analysis. Am Heart J 2008; 155 (2): 332–8
Aidelsburger P, Grabein K, Klauss V, et al. Cost-effectiveness of cardiac resynchronization therapy in combination with an implantable cardioverter defibrillator (CRT-D) for the treatment of chronic heart failure from a German health care system perspective. Clin Res Cardiol 2008; 97 (2): 89–97
Göhler A, Conrads-Frank A, Worrell SS, et al. Decisionanalytic evaluation of the clinical effectiveness and costeffectiveness of management programmes in chronic heart failure. Eur J Heart Fail 2008; 10 (10): 1026–32
Miller G, Randolph S, Forkner E, et al. Long-term costeffectiveness of disease management in systolic heart failure. Med Decis Making 2009; 29 (3): 325–33
Ribeiro RA, Stella SF, Camey SA, et al. Cost-effectiveness of implantable cardioverter-defibrillators in Brazil: primary prevention analysis in the public sector. Value Health 2010 Mar-Apr; 13 (2): 160–8
Rosen VM, Taylor DC, Parekh H, et al. Cost effectiveness of intensive lipid-lowering treatment for patients with congestive heart failure and coronary heart disease in the US. Pharmacoeconomics 2010; 28 (1): 47–60
Caro JJ. Pharmacoeconomic analyses using discrete event simulation. Pharmacoeconomics 2005; 23 (4): 323–32
Drummond M, Schwartz JS, Jonsson B, et al. Response from the authors of “Key principles for the improved conduct of health technology assessments for resource allocation decisions”. Int J Technol Assess Health Care 2008; 24 (3): 367–8
Acknowledgements
This work was supported by the Competence Network of Heart Failure, funded by the Federal Ministry of Education and Research (BMBF), Germany (funding no. 01GI0205).
The authors have no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Search Strategies
In MEDLINE/PreMEDLINE (1966 to June 2010), we used one of the following Medical Subject Heading (MeSH) terms: ‘Technology Assessment, Biomedical’, ‘Decision Support Techniques’, ‘Models, Statistical’, ‘Markov Chains’, ‘Monte Carlo Method’, ‘Economics’, ‘Health Planning’ or ‘Quality-Adjusted Life Years’, combined with the MeSH term ‘Heart Failure’.
In EMBASE Drugs and Pharmacology (1966 to June 2010), our keywords were ‘decision analysis’, ‘decision-analytic’, ‘decision model’, ‘health care model’, ‘health care evaluation model’, ‘decision tree’, ‘Markov model’, ‘cost-effectiveness’, ‘cost-utility’, ‘cost-benefit’, ‘cost-minimi[z/s]ation’ or ‘QALY’ in combination with the term ‘heart failure’.
In EconLit and the Cost-Effectiveness Analysis Registry, we searched for ‘Heart Failure’.
In addition, a hand search was conducted. We searched the references of retrieved papers for publications that might be eligible.
Rights and permissions
About this article
Cite this article
Goehler, A., Geisler, B.P., Manne, J.M. et al. Decision-Analytic Models to Simulate Health Outcomes and Costs in Heart Failure. Pharmacoeconomics 29, 753–769 (2011). https://doi.org/10.2165/11585990-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11585990-000000000-00000