Abstract
Background
Hypertension often occurs concomitantly with diabetes mellitus, such that >50% of adults with type 2 diabetes have hypertension. These individuals are at a greater risk of developing renal and cardiovascular disease. The currently recommended BP goal of <130/80 mmHg for patients with type 2 diabetes is achieved in only 37.5% of treated patients with diabetes and hypertension.
Methods
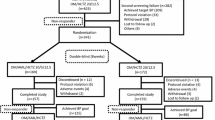
The antihypertensive efficacy of olmesartan medoxomil (OM) ± hydrochlorothiazide (HCTZ) was investigated in prespecified subgroups (age <65/≥65 years, Blacks/non-Blacks, males/females, or stage 1/ stage 2 hypertension) of patients with hypertension and type 2 diabetes enrolled in an open-label, single-arm study (n= 192). Patients started treatment with OM 20 mg/day and were uptitrated at 3-week intervals to OM 40, OM/HCTZ 40/12.5, and OM/HCTZ 40/25 mg/day if BP was ≥120/70 mmHg. The primary endpoint was the change in mean 24-hour ambulatory SBP from baseline to week 12, assessed by mean 24-hour ambulatory BP monitoring. Secondary endpoints included changes in mean 24-hour ambulatory DBP, mean daytime ambulatory BP, mean nighttime ambulatory BP, and mean office seated BP, and the proportions of patients achieving prespecified ambulatory BP targets.
Setting
This was a multicenter study (24 sites) that took place between November 2006 and November 2007 in the US.
Results
BP reductions were significant (p < 0.0001) and similar among subgroups of patients with type 2 diabetes. Following dose titration to OM/HCTZ 40/25 mg/day, similar proportions of patients in the age, race, and sex subgroups (approximately 60–64% across these subgroups) achieved an ambulatory BP target of <130/80 mmHg. A larger proportion of patients with type 2 diabetes and stage 1 hypertension achieved this same goal compared with patients with stage 2 hypertension (75% vs 46.3%). The combination of OM/HCTZ was well tolerated in all patient subgroups irrespective of age, race, sex, or hypertension severity.
Conclusions
In this open-label study, OM/HCTZ combination therapy was efficacious and well tolerated in subgroups of patients with diabetes and hypertension.
[Clinical Trials Registry Number: NCT00403481]










Similar content being viewed by others
References
Rosamond W, Flegal K, Furie K, et al. Heart disease and stroke statistics — 2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2008 Jan 29; 117(4): e25–146.
Kabakov E, Norymberg C, Osher E, et al. Prevalence of hypertension in type 2 diabetes mellitus: impact of the tightening definition of high blood pressure and association with confounding risk factors. J Cardiometab Syndr 2006 Spring; 1(2): 95–101.
Resnick HE, Foster GL, Bardsley J, et al. Achievement of American Diabetes Association clinical practice recommendations among U.S. adults with diabetes, 1999–2002: the National Health and Nutrition Examination Survey. Diabetes Care 2006 Mar; 29(3): 531–7.
Arauz-Pacheco C, Parrott MA, Raskin P. The treatment of hypertension in adult patients with diabetes. Diabetes Care 2002 Jan; 25(1): 134–47.
Legato MJ, Gelzer A, Goland R, et al. Gender-specific care of the patient with diabetes: review and recommendations. Gend Med 2006 Jun; 3(2): 131–58.
American Diabetes Association. Standards of medical care in diabetes — 2008. Diabetes Care 2008 Jan; 31 Suppl. 1: S12–54.
Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003 Dec; 42(6): 1206–52.
Mancia G, De Backer G, Dominiczak A, et al. 2007 Guidelines for the Management of Arterial Hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2007 Jun; 25(6): 1105–87.
Rodbard H, Blonde L, Braithwaite S, et al. American Association of Clinical Endocrinologists medical guidelines for clinical practice for the management of diabetes mellitus. Endocr Pract 2007 May–Jun; 13 Suppl. 1: 1–68.
Ong KL, Cheung BM, Man YB, et al. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension 2007 Jan; 49(1): 69–75.
McFarlane SI, Jacober SJ, Winer N, et al. Control of cardiovascular risk factors in patients with diabetes and hypertension at urban academic medical centers. Diabetes Care 2002 Apr; 25(4): 718–23.
Pessina AC. Target organs of individuals with diabetes caught between arterial stiffness and damage to the microcirculation. J Hypertens 2007 Jun; 25 Suppl. 1: S13–8.
Neutel JM, Kereiakes DJ, Waverczak WF, et al. Effects of an olmesartan medoxomil based treatment algorithm on 24-hour blood pressure control in patients with hypertension and type 2 diabetes. Curr Med Res Opin 2010 Mar; 26(3): 721–8.
Jula A, Puukka P, Karanko H. Multiple clinic and home blood pressure measurements versus ambulatory blood pressure monitoring. Hypertension 1999 Aug; 34(2): 261–6.
Mancia G, Parati G. Ambulatory blood pressure monitoring and organ damage. Hypertension 2000 Nov; 36(5): 894–900.
Mancia G, Parati G, Hennig M, et al. Relation between blood pressure variability and carotid artery damage in hypertension: baseline data from the European Lacidipine Study on Atherosclerosis (ELSA). J Hypertens 2001 Nov; 19(11): 1981–9.
Mancia G, Zanchetti A, Agabiti-Rosei E, et al. Ambulatory blood pressure is superior to clinic blood pressure in predicting treatment-induced regression of left ventricular hypertrophy. SAMPLE Study Group. Study on Ambulatory Monitoring of Blood Pressure and Lisinopril Evaluation. Circulation 1997 Mar 18; 95(6): 1464–70.
Neutel JM. The importance of 24-h blood pressure control. Blood Press Monit 2001 Feb; 6(1): 9–16.
Fliser D, Wagner KK, Loos A, et al. Chronic angiotensin II receptor blockade reduces (intra)renal vascular resistance in patients with type 2 diabetes. J Am Soc Nephrol 2005 Apr; 16(4): 1135–40.
Nakayama S, Watada H, Mita T, et al. Comparison of effects of olmesartan and telmisartan on blood pressure and metabolic parameters in Japanese early-stage type-2 diabetics with hypertension. Hypertens Res 2008 Jan; 31(1): 7–13.
Fukuda M, Yamanaka T, Mizuno M, et al. Angiotensin II type 1 receptor blocker, olmesartan, restores nocturnal blood pressure decline by enhancing daytime natriuresis. J Hypertens 2008 Mar; 26(3): 583–8.
Kereiakes DJ, Neutel J, Stoakes KA, et al. The effects of an olmesartan medoxomil-based treatment algorithm on 24-hour blood pressure levels in patients aged 65 and older. J Clin Hypertens (Greenwich) 2009; 11: 1–11.
Chavanu K, Merkel J, Quan AM. Role of ambulatory blood pressure monitoring in the management of hypertension. Am J Health Syst Pharm 2008 Feb 1; 65(3): 209–18.
Manios ED, Koroboki EA, Tsivgoulis GK, et al. Factors influencing whitecoat effect. Am J Hypertens 2008 Feb; 21(2): 153–8.
Palatini P. Too much of a good thing? A critique of overemphasis on the use of ambulatory blood pressure monitoring in clinical practice. J Hypertens 2002 Oct; 20(10): 1917–23.
Sega R, Cesana G, Milesi C, et al. Ambulatory and home blood pressure normality in the elderly: data from the PAMELA population. Hypertension 1997 Jul; 30(1 Pt 1): 1–6.
Calvo C, Hermida RC, Ayala DE, et al. The ‘ABPM effect’ gradually decreases but does not disappear in successive sessions of ambulatory monitoring. J Hypertens 2003 Dec; 21(12): 2265–73.
Pang TC, Brown MA. Accuracy of ambulatory blood pressure monitors in routine clinical practice. Am J Hypertens 2006 Aug; 19(8): 801–9.
Acknowledgments
This study was funded by Daiichi Sankyo, Inc. The authors would like to thank Alan J. Klopp, PhD, and Christopher J. Jones, PhD, of inScience Communications, a Wolters Kluwer business, for providing medical writing support funded by Daiichi Sankyo, Inc.
We thank the following participating investigators: Gregory Collins, MD (Charlotte Clinical Research, Charlotte, NC); Charles H. DeBusk, MD (Heartland Medical, PC, New Tazewell, TN); Andrew Feldman, DO (University Clinical Research Deland, Deland, FL); Robert Frederickson, MD (Brookwood Internists, PC, Birmingham, AL); David Johnson, MD (Searcy Medical Center, Searcy, AR); Dean J. Kereiakes, MD (Lindner Clinical Trial Center, Cincinnati, OH); Marc Kozinn, MD (Cardiology & Internal Medicine, Williamsville, NY); Gregory Lakin, MD (Professional Research Network of Kansas, Wichita, KS); Andrew Lewin, MD (National Research Institute, Los Angeles, CA); Thomas Littlejohn, MD (Piedmont Medical Research Associates, Winston-Salem, NC); Barry Lubin, MD (Hampton Roads Center for Clinical Research Inc., Norfolk, VA); Nicholas Messina, MD (Vista Medical Research, Inc., Mesa, AZ); Bradley Musser, MD (Bexar Clinical Trials, Richardson, TX); Joel Neutel, MD (Orange County Research Center, Tustin, CA); Stephen Ong, MD (MD Medical Research, Oxon Hill, MD); Irwin S. Plisco, MD (Florissant, MO); Jaime Sandoval, MD (Padre Coast Clinical Research, Corpus Christi, TX); Robert Strzinek, MD (Texas FamiliCare Clinical Research, Colleyville, TX); Dan Sugimoto, MD (Cedar-Cross Research Center, Chicago, IL); Jeffrey Wayne, MD (Clinical Trials Research, Lincoln, CA); Robert Weiss, MD (Maine Research Associates, Auburn, ME); Larry I. Gilderman, MD (University Clinical Research, Inc., Pembroke Pines, FL); Daniel Yarrish, MD (Salt Lake Research, LLC, Salt Lake City, UT); Andrea Phillips, MD (Philips Medical Services, Jackson, MS).
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Neutel, J.M., Kereiakes, D.J. & The BENIFICIARY Investigators. An Olmesartan Medoxomil-Based Treatment Algorithm is Effective in Achieving 24-Hour BP Control in Patients with Type 2 Diabetes Mellitus, Regardless of Age, Race, Sex, or Severity of Hypertension. Am J Cardiovasc Drugs 10, 289–303 (2010). https://doi.org/10.2165/11584690-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11584690-000000000-00000