Abstract
Multiple sclerosis (MS) is an inflammatory, demyelinating, autoimmune disease of the CNS. There are currently a number of disease-modifying medications for MS that modulate or suppress the immune system; however, these medications do not directly relieve MS symptoms, which include visual deficits, gait problems, sensory deficits, weakness, tremor, spasticity and pain, among others.
Pain is a common symptom in MS which has recently been estimated to be experienced by more than 40% of patients. Nociceptive pain occurs as an appropriate physiological response transmitted to a conscious level when nociceptors in bone, muscle or any body tissue are activated, warning the organism of tissue damage. Neuropathic pain is initiated as a direct consequence of a lesion or disease affecting the somatosensory system, with no physiological advantage. Nociceptive and neuropathic pain in MS may be present concurrently and at different stages of the disease, and may be associated with other symptoms. Central neuropathic pain has been reported to be among the most common pain syndromes in MS. It is described as constant, often spontaneous, burning occurring more frequently in the lower limbs. Treatment typically includes tricyclic antidepressants and antiepileptic medications, although studies have been conducted in relatively small samples and optimal dosing has not been confirmed. Cannabinoids have been among the few treatments studied in well designed, randomized, placebo-controlled trials for central neuropathic pain. In the largest of these trials, which included 630 subjects, a 15-week comparison between Δ9-tetrahydrocannabinol and placebo was performed. More patients receiving active treatment perceived an improvement in pain than those receiving placebo, although approximately 20% of subjects reported worsening of pain while on active treatment.
Trigeminal neuralgia, while affecting less than 5% of patients with MS, is the most studied pain syndrome. The pain can be extreme and is typically treated with carbamazepine, although adverse effects can mimic an MS exacerbation. Painful topic spasms occur in approximately 11% of the MS population and are treated with antispasticity medications such as baclofen and benzodiazepines. Gabapentin has also demonstrated efficacy, but all studies have included small sample sizes.
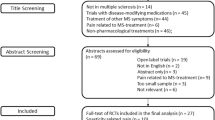
In general, evidence for treating pain in MS is limited. Many clinical features of pain are often unrecognized by clinicians and are difficult for patients to describe. Treatment is often based on anecdotal reports and clinical experience. We present a review of treatment options for pain in MS, which should serve to update current knowledge, highlight shortcomings in clinical research and provide indications towards achieving evidence-based treatment of pain in MS.


Similar content being viewed by others
References
Paty DW, Ebers GC. Clinical features. In: Paty DW, Ebers GC, editors. Multiple sclerosis. Philadelphia (PA): F.A. Davis Company, 1998: 135–91
Merskey H, Bogduk N. Classification of chronic paindescriptions of chronic pain syndromes and definitions of pain terms. 2nd ed. Seattle (WA): IASP Press, 1994
Brichetto G, Messmer UM, Mancardi GL, et al. Symptomatic medication use in multiple sclerosis. Mult Scler 2003 Oct; 9(5): 458–60
Hadjimichael O, Kerns RD, Rizzo MA, et al. Persistent pain and uncomfortable sensations in persons with multiple sclerosis. Pain 2007 Jan; 127(1–2): 34–41
Ehde DM, Gibbons LE, Chwastiak L, et al. Chronic pain in a large community sample of persons with multiple sclerosis. Mult Scler 2003 Dec; 9(6): 605–11
Solaro C, Brichetto G, Amato MP, et al. The prevalence of pain in multiple sclerosis: a multicenter cross-sectional study. Neurology 2004; 63: 919–21
Svendsen KB, Jensen TS, Overad K, et al. Pain in patients with multiple sclerosis. Arch Neurol 2003; 60: 1089–94
Moulin DE, Foley KM, Ebers GC. Pain syndromes in multiple sclerosis. Neurology 1988 Dec; 38(12): 1830–4
Kraft GH, Freal JE, Coryell JK. Disability, disease duration, and rehabilitation service needs in multiple sclerosis: patient perspectives. Arch Phys Med Rehabil 1986 Mar; 67(3): 164–8
Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health 1990; 13(4): 227–36
Grond S, Radbruch L, Meuser T, et al. Assessment and treatment of neuropathic cancer pain following WHO guidelines. Pain 1999 Jan; 79(1): 15–20
Treede RD, Jensen TS, Campbell JN, et al. Neuropathic pain: redefinition and a grading system for clinical and research purposes. Neurology 2008 Apr 29; 70(18): 1630–5
Cruccu G, Biasiotta A, Di Rezze S, et al. Trigeminal neuralgia and pain related to multiple sclerosis. Pain 2009 Jun; 143(3): 186–91
Cianchetti C, Zuddas A, Randazzo AP, et al. Lamotrigine adjunctive therapy in painful phenomena in MS: preliminary observations. Neurology 1999 Jul 22; 53(2): 433
Breuer B, Pappagallo M, Knotkova H, et al. A randomized double-blind, placebo-controlled two period crossover pilot trial of lamotrigine in patients with central pain due to multiple sclerosis. Clin Ther 2007; 29: 2022–30
Houtchens MK, Richert JR, Sami A, et al. Open label gabapentin treatment for pain in multiple sclerosis. Mult Scler 1997; 3(4): 250–3
Rossi S, Mataluni G, Codeca C et al. Effects of levetiracetam on chronic pain in multiple sclerosis: results of a randomized placebo-controlled study. EurJ Neurol 2009; 16: 360–6
Solaro C, Boemker M, Tanganelli P. Pregabalin for treating paroxysmal symptoms in multiple sclerosis: a pilot study. J Neurol 2009 Oct; 256(10): 1773–4
Svendsen KB, Jensen TS, Bach FW. Does the cannabinoid dronabinol reduce central pain in multiple sclerosis? Randomised double blind placebo controlled crossover trial. BMJ 2004 Jul 31; 329(7460): 253
Rog DJ, Nurmikko TJ, Friede T, et al. Randomized, controlled trial of cannabis-based medicine in central pain in multiple sclerosis. Neurology 2005 Sep 27; 65(6): 812–9
Solaro C, Brichetto G, Battaglia MA, et al. Antiepileptic medications in multiple sclerosis: adverse effects in a threeyear follow-up study. Neurol Sci 2005 Feb; 25(6): 307–10
McCleane G. Lamotrigine can reduce neurogenic pain associated with multiple sclerosis. Clin J Pain 1998 Sep; 14(3): 269–70
Samkoff LM, Daras M, Tuchman AJ, et al. Amelioration of refractory dysesthetic limb pain in multiple sclerosis by gabapentin. Neurology 1997 Jul; 49(1): 304–5
Solaro C, Tanganelli P. Acute delirium in patients with multiple sclerosis treated with pregabalin. Clin Neuropharmacol 2009 Jul–Aug; 32(4): 236–7
Herman RM, D’Luzansky SC, Ippolito R. Intrathecal baclofen suppresses central pain in patients with spinal lesions: a pilot study. Clin J Pain 1992 Dec; 8(4): 338–45
Sadiq S, Poopatana C. Intrathecal baclofen and morphine in multiple sclerosis patients with severe pain and spasticity. J Neurol 2007; 254: 1464–5
Kalman S, Österberg A, Sörensen J, et al. Morphine responsiveness in a group of well-defined multiple sclerosis patients: a study with i.v. morphine. Eur J Pain 2002; 6: 69–80
Sakurai M, Kanazawa I. Positive symptoms in multiple sclerosis: their treatment with sodium channel blockers, lidocaine and mexiletine. J Neurol Sci 1999 Jan 15; 162(2): 162–8
Dahm PO, Nitescu PV, Appelgren LK, et al. Long-term intrathecal (i.t.) infusion of bupivacaine relieved intractable pain and spasticity in a patient with multiple sclerosis. Eur J Pain 1998 Mar; 2(1): 81–5
Solari A. Role of health-related quality of life measures in the routine care of people with multiple sclerosis. Health Qual Life Outcomes 2005 Mar 18; 3: 16
Rog DJ, Nurmikko TJ, Young CA. Oromucosal delta9-tetrahydrocannabinol/cannabidiol for neuropathic pain associated with multiple sclerosis: an uncontrolled, openlabel 2-year extension trial. Clin Ther 2007 Sep; 29(9): 2068–79
Zajicek J, Fox P, Sanders H, et al., UK MS Research Group. Cannabinoids for treatment of spasticity and other symptoms related to multiple sclerosis (CAMS study): multicentre randomised placebo-controlled trial. Lancet 2003 Nov 8; 362(9395): 1517–26
Wade DT, Makela P, Robson P, et al. Do cannabis-based medicinal extracts have general or specific effects on symptoms in multiple sclerosis? A double-blind, randomized, placebo-controlled study on 160 patients. Mult Scler 2004 Aug; 10(4): 434–41
Parker HL. Trigeminal neuralgic pain associated with multiple sclerosis. Brain 1928; 51: 46–62
Jensen TS, Rasmussen P, Reske-Nielsen E. Association of trigeminal neuralgia with multiple sclerosis: clinical and pathological features. Acta Neurol Scand 1982; 65: 182–9
Hooge JP, Redekop WK. Trigeminal neuralgia in multiple sclerosis. Neurology 1995; 45(7): 1294–6
Osterberg A, Boivie J, Thuomas KA. Central pain in multiple sclerosis: prevalence and clinical characteristics. Eur J Pain 2005 Oct; 9(5): 531–42
Espir ML, Millac P. Treatment of paroxysmal disorders in multiple sclerosis with carbamazepine (Tegretol). J Neurol Neurosurg Psychiatry 1970; 33(4): 528–31
Solaro C, Messmer UM, Uccelli A, et al. Low-dose gabapentin combined with either lamotrigine or carbamazepine can be useful therapies for trigeminal neuralgia in multiple sclerosis. Eur Neurol 2000; 44(1): 45–8
Lunardi G, Leandri M, Albano C, et al. Clinical effectiveness of lamotrigine and plasma levels in essential and symptomatic trigeminal neuralgia. Neurology 1997; 48: 1714–7
Leandri M, Lunardi G, Inglese M, et al. Lamotrigine in trigeminal neuralgia secondary to multiple sclerosis. J Neurol 2000; 247(7): 556–8
Khan OA. Gabapentin relieves trigeminal neuralgia in multiple sclerosis patients. Neurology 1998; 51(2): 611–4
Solaro C, Lunardi GL, Capello E, et al. An open-label trial of gabapentin treatment of paroxysmal symptoms in multiple sclerosis patients. Neurology 1998; 51(2): 609–11
Zvartau-Hind M, Din MU, Gilani A, et al. Topiramate relieves refractory trigeminal neuralgia in patients with MS. Neurology 2000; 55(10): 1587–8
Solaro C, Uccelli MM, Brichetto G, et al. Topiramate relieves idiopathic and symptomatic trigeminal neuralgia. J Pain Symptom Manage 2001; 21(5): 367–6
Reder AT, Arnason BGW. Trigeminal neuralgia in multiple sclerosis relieved by a prostaglandin E analogue. Neurology 1995; 45: 1097–100
DMKG Study Group. Misoprostol in the treatment of trigeminal neuralgia associated with multiple sclerosis. J Neurol 2003; 250(5): 542–5
Ramsaransing G, Zwanikken C, De Keyser J. Worsening of symptoms of multiple sclerosis associated with carbamazepine. BMJ 2000 Apr 22; 320(7242): 1113
Juniper RP, Glynn CJ. Association between paroxysmal trigeminal neuralgia and atypical facial pain. Br J Oral Maxillofac Surg 1999; 37: 444–7
Elrasheed AA, Worthington HV, Ariyaratnam S, et al. Opinions of UK specialists about terminology, diagnosis, and treatment of atypical facial pain: a survey. Br J Oral Maxillofac Surg 2004; 42: 566–71
Rudick R, Goodkin D. Multiple sclerosis therapeutics. London: Martin Dunitz Ltd, 1999: 542
Al-Araji AH, Oger J. Reappraisal of Lhermitte’s sign in multiple sclerosis. Mult Scler 2005 Aug; 11(4): 398–402
Minagar A, Sheremata WA. Glossopharyngeal neuralgia and MS. Neurology 2000 Mar 28; 54(6): 1368–70
Solaro C, Uccelli MM, Guglieri P, et al. Gabapentin is effective in treating nocturnal painful spasms in multiple sclerosis. Mult Scler 2000; 6(3): 192–3
Solaro C, Tanganelli P. Tiagabine for treating painful tonic spasms in multiple sclerosis: a pilot study [letter]. J Neurol Neurosurg Psychiatry 2004 Feb; 75(2): 341
Restivo DA, Tinazzi M, Patti F, et al. Botulinum toxin treatment of painful tonic spasms in multiple sclerosis. Neurology 2003 Sep 9; 61(5): 719–20
Miro J, Garcia-Monco C, Leno C, et al. Pelvic pain: an undescribed paroxysmal manifestation of multiple sclerosis. Pain 1988; 32: 73–5
Moulin D. Pain in central and peripheral demyelinating disorders. Neurol Clin 1998 Nov; 16: 889–98
Thompson AJ. Symptomatic treatment in multiple sclerosis. Curr Opin Neurol 1998; 11: 305–9
Acknowledgements
The authors thank the Italian Multiple Sclerosis Society for providing administrative assistance in the preparation of the manuscript. No sources of funding were used to assist in the preparation of this review. The authors have no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Solaro, C., Uccelli, M.M. Pharmacological Management of Pain in Patients with Multiple Sclerosis. Drugs 70, 1245–1254 (2010). https://doi.org/10.2165/11537930-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11537930-000000000-00000