Abstract
Background: Peptic ulcer bleeding (PUB) is a serious and sometimes fatal condition. The outcome of PUB strongly depends on the risk of rebleeding. A recent multinational placebo-controlled clinical trial (ClinicalTrials.gov identifier: NCT00251979) showed that high-dose intravenous (IV) esomeprazole, when administered after successful endoscopic haemostasis in patients with PUB, is effective in preventing rebleeding. From a policy perspective it is important to assess the cost efficacy of this benefit so as to enable clinicians and payers to make an informed decision regarding the management of PUB.
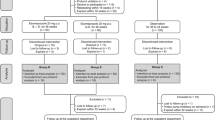
Objective: Using a decision-tree model, we compared the cost efficacy of highdose IV esomeprazole versus an approach of no-IV proton pump inhibitor for prevention of rebleeding in patients with PUB.
Method: The model adopted a 30-day time horizon and the perspective of third-party payers in the USA and Europe. The main efficacy variable was the number of averted rebleedings. Healthcare resource utilization costs (physician fees, hospitalizations, surgeries, pharmacotherapies) relevant for the management of PUB were also determined. Data for unit costs (prices) were primarily taken from official governmental sources, and data for other model assumptions were retrieved from the original clinical trial and the literature.
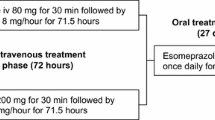
After successful endoscopic haemostasis, patients received either highdose IV esomeprazole (80mg infusion over 30 min, then 8mg/hour for 71.5 hours) or no-IV esomeprazole treatment, with both groups receiving oral esomeprazole 40mg once daily from days 4 to 30.
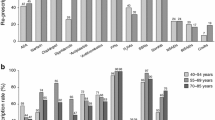
Results: Rebleed rates at 30 days were 7.7% and 13.6%, respectively, for the high-dose IV esomeprazole and no-IV esomeprazole treatment groups (equating to a number needed to treat of 17 in order to prevent one additional patient from rebleeding). In the US setting, the average cost per patient for the high-dose IV esomeprazole strategy was $US14 290 compared with $US14 239 for the no-IV esomeprazole strategy (year 2007 values). For the European setting, Sweden and Spain were used as examples. In the Swedish setting the corresponding respective figures were Swedish kronor (SEK)67 862 ($US9220 at average 2006 interbank exchange rates) and SEK67 807 ($US9212) [year 2006 values]. Incremental cost-effectiveness ratios were $US866 and SEK938 ($US127), respectively, per averted rebleed when using IV esomeprazole. For the Spanish setting, the high-dose IV esomeprazole strategy was dominant (more effective and less costly than the no-IV esomeprazole strategy) [year 2008 values]. All results appeared robust to univariate/threshold sensitivity analysis, with high-dose IV esomeprazole becoming dominant with small variations in assumptions in the US and Swedish settings, while remaining a dominant approach in the Spanish scenario across a broad range of values. Sensitivity variables with prespecified ranges included lengths of stay and per diem assumptions, rebleeding rates and, in some cases, professional fees.
Conclusion: In patients with PUB, high-dose IV esomeprazole after successful endoscopic haemostasis appears to improve outcomes at a modest increase in costs relative to a no-IV esomeprazole strategy from the US and Swedish thirdparty payer perspective. Whereas, in the Spanish setting, the high-dose IV esomeprazole strategy appeared dominant, being more effective and less costly.






Similar content being viewed by others
References
British Society of Gastroenterology Endoscopy Committee. Non-variceal upper gastrointestinal haemorrhage: guidelines. Gut 2002 Oct; 51 Suppl. 4: iv1–6
Vreeburg EM, Snel P, de Bruijne JW, et al. Acute upper gastrointestinal bleeding in the Amsterdam area: incidence, diagnosis, and clinical outcome. Am J Gastroenterol 1997 Feb; 92 (2): 236–43
Blatchford O, Davidson LA, Murray WR, et al. Acute upper gastrointestinal haemorrhage in west of Scotland: case ascertainment study. BMJ 1997 Aug 30; 315 (7107): 510–4
Kapsoritakis AN, Ntounas EA, Makrigiannis EA, et al. Acute upper gastrointestinal bleeding in Central Greece: the role of clinical and endoscopic variables in bleeding outcome. Dig Dis Sci 2009 Feb; 54 (2): 333–41
Theocharis GJ, Thomopoulos KC, Sakellaropoulos G, et al. Changing trends in the epidemiology and clinical outcome of acute upper gastrointestinal bleeding in a defined geographical area in Greece. J Clin Gastroenterol 2008 Feb; 42 (2): 128–33
van Leerdam ME, Vreeburg EM, Rauws EA, et al. Acute upper GI bleeding: did anything change? Time trend analysis of incidence and outcome of acute upper GI bleeding between 1993/1994 and 2000. Am J Gastroenterol 2003 Jul; 98 (7): 1494–9
Lewis JD, Bilker WB, Brensinger C, et al. Hospitalization and mortality rates from peptic ulcer disease and GI bleeding in the 1990s: relationship to sales of nonsteroidal anti-inflammatory drugs and acid suppression medications. Am J Gastroenterol 2002 Oct; 97 (10): 2540–9
Adam V, Barkun AN. Estimates of costs of hospital stay for variceal and nonvariceal upper gastrointestinal bleeding in the United States. Value Health 2008 Jan-Feb; 11 (1): 1–3
Targownik LE, Nabalamba A. Trends in management and outcomes of acute nonvariceal upper gastrointestinal bleeding: 1993-2003. Clin GastroenterolHepatol 2006 Dec; 4 (12): 1459–66
Rockall TA, Logan RF, Devlin HB, et al. Incidence of and mortality from acute upper gastrointestinal haemorrhage in the United Kingdom. Steering Committee and members of the National Audit of Acute Upper Gastrointestinal Haemorrhage. BMJ 1995 Jul 22; 311 (6999): 222–6
Barkun A, Sabbah S, Enns R, et al. The Canadian Registry on Nonvariceal Upper Gastrointestinal Bleeding and Endoscopy (RUGBE): endoscopic hemostasis and proton pump inhibition are associated with improved outcomes in a real-life setting. Am J Gastroenterol 2004 Jul; 99 (7): 1238–46
Longstreth GF. Epidemiology of hospitalization for acute upper gastrointestinal hemorrhage: a population-based study. Am J Gastroenterol 1995 Feb; 90 (2): 206–10
Laine L, Peterson WL. Bleeding peptic ulcer. N Engl J Med 1994 Sep 15; 331 (11): 717–27
Barkun A, Bardou M, Marshall JK. Consensus recommendations for managing patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med 2003 Nov 18; 139 (10): 843–57
Bardou M, Toubouti Y, Benhaberou-Brun D, et al. Metaanalysis: proton-pump inhibition in high-risk patients with acute peptic ulcer bleeding. Aliment Pharmacol Ther 2005 Mar 15; 21 (6): 677–86
Leontiadis GI, Sharma VK, Howden CW. Proton pump inhibitor therapy for peptic ulcer bleeding: Cochrane collaboration meta-analysis of randomized controlled trials. Mayo Clin Proc 2007 Mar; 82 (3): 286–96
Leontiadis GI, Sharma VK, Howden CW. Systematic review and meta-analysis: enhanced efficacy of proton-pump inhibitor therapy for peptic ulcer bleeding in Asia. A post hoc analysis from the Cochrane Collaboration. Aliment Pharmacol Ther 2005 May 1; 21 (9): 1055–61
Sung JJY, Barkun A, Kuipers EJ, et al. Intravenous esomeprazole for prevention of recurrent peptic ulcer bleeding: a randomized controlled trial. Ann Intern Med 2009; 150 (7): 455–64
Al-Sabah S, Barkun AN, Herba K, et al. Cost-effectiveness of proton-pump inhibition before endoscopy in upper gastrointestinal bleeding. Clin Gastroenterol Hepatol 2008 Apr; 6 (4): 418–25
Healthcare Cost and Utilization Project. Nationwide inpatient sample 2002 [online]. Available from URL: http://www.hcup-us.ahrq.gov/nisoverview.jsp [Accessed 2008 Jul 1]
Spiegel BM, Dulai GS, Lim BS, et al. The cost-effectiveness and budget impact of intravenous versus oral proton pump inhibitors in peptic ulcer hemorrhage. Clin Gastroenterol Hepatol 2006 Aug; 4 (8): 988–97
Spiegel BM, Chiou CF, Ofman JJ. Minimizing complications from nonsteroidal antiinflammatory drugs: costeffectiveness of competing strategies in varying risk groups. Arthritis Rheum 2005 Apr 15; 53 (2): 185–97
Gerson L, Lin OS. Cost-benefit analysis of capsule endoscopy compared with standard upper endoscopy for the detection of Barrett’s esophagus. Clin Gastroenterol Hepatol 2007 Mar; 5 (3): 319–25
Red Book 2006. Pharmacy’s fundamental reference (Red Book drug topics). Montvale (NJ): Thomson PDR, 2006
Swedish Association of Local Authorities and Regions (SALAR) [online]. Available from URL: http://www.skl.se [Accessed 2008 May 12]
Dental and Pharmaceutical Benefits Agency (TLV, formerly LFN). Kostnadseffektiva läkemedel [online]. Available from URL: http://www.tlv.se [Accessed 2008 May 12]
Decreto 83/2004, do 15 de abril, polo que se establecen as tarifas dos servizos sanitarios prestados nos centros dependentes do Servizo Galego de Saúde e nas fundacións públicas sanitarias. Diario Oficial de Galicia 2004 May 4; No. 85: 6235–49
Decreto 272/2005, de 27 de diciembre, por el que se establecen y regulan los precios públicos corespondientes a los servicios sanitarios del Servicio Extremeño de Salud. Diario Oficial de Extremadura 2005 Dec 31; No. 150: 18342–65
Orden SLT/483/2005, de 15 de diciembre, por la que se regulan los supuestos y conceptos facturables y se aprueban los precios públicos correspondientes a los servicios que presta el Instituto Catalán de la Salud. Diario Oficial de la Generalidad de Cataluña 2005 Dec 30; No. 4540
Resolución de 16-01-2006, del Sescam, sobre precios a aplicar por sus centros sanitarios a terceros obligados al pago o a los usuarios sin derecho a asistencia sanitaria. Diario Oficial de Castilla La Mancha 2006 Jan 26; No. 19: 1365–7
Resolución de 28 de octubre de 2005, del Presidente de la Gerencia Regional de Salud, de revisión de las condiciones económicas aplicables en el año 2005, a la perstacio n de servicios de asistencia sanitaria concertada en el àmbito de la Gerencia Regional de Salud. BOCyL 2005 Nov 7; No. 214
Orden de 7 de abril de 2006, por la que se revisan las condiciones económicas aplicables a la asistencia sanitaria prestada con medios ajenos en el ejercicio 2005. Boletín Oficial de Canarias 2006 Apr; No. 76: 7403–24
Decreto 34/2006 de 19 de abril, por el que se establecen los precios públicos por la prestación de los servicios y actividades de naturaleza sanitaria de los centros dependientes del Servicio de Salud del Principado de Asturias. Boletín Oficial del Principado de Asturias 2006 May 9; No. 105: 9353–8
Ministerio de Sanidad y Consumo. Cifras de referencia nacional de los Grupos Relacionados por el Diagnóstico (GRD). Pesos Españoles y Costes para el SNS. Año 2005 [online]. Available from URL: http://www.msc.es/estadEstudios/estadisticas/docs/pesosEspGRD_ApV18Ano2005.pdf [Accessed 2008 May 1]
Orden 234/2005, de 23 de febrero, del Consejero de Sanidad y Consumo, por la que se fijan los precios públicos por la prestación de los servicios y actividades de naturaleza sanitaria de la Red de Centros de la Comunidad Autónoma. Boletín Oficial de la Comunidad de Madrid 2005 Mar 8; No. 56
Hospital Clinic i Provincial de Barcelona. Barcelona: Tarifari de, 1997
Hospital de la Santa Creu i Sant Pau. Barcelona: Memoria, 1992
Ministry of Health. Nomenclator of medicines [online]. Available from URL: http://www.msc.es/profesionales/farmacia/nomenclatorDI.htm [Accessed 2008 May 1]
General Spanish Council of Pharmacists. Pharmaceutical Association [online]. Available from URL: http://www.portalfarma.com [Accessed 2008 May 1]
Barkun AN, Herba K, Adam V, et al. The cost-effectiveness of high-dose oral proton pump inhibition after endoscopy in the acute treatment of peptic ulcer bleeding. Aliment Pharmacol Ther 2004 Jul 15; 20 (2): 195–202
Barkun AN, Herba K, Adam V, et al. High-dose intravenous proton pump inhibition following endoscopic therapy in the acute management of patients with bleeding peptic ulcers in the USA and Canada: a cost-effectiveness analysis. Aliment Pharmacol Ther 2004 Mar 1; 19 (5): 591–600
Department of Health & Human Services. Centers for Medicare & Medicaid Services [online]. Available from URL: http://www.cms.hhs.gov/ [Accessed 2009 Nov 23]
Lee KK, You JH, Wong IC, et al. Cost-effectiveness analysis of high-dose omeprazole infusion as adjuvant therapy to endoscopic treatment of bleeding peptic ulcer. Gastrointest Endosc 2003 Feb; 57 (2): 160–4
Spiegel BM, Ofman JJ, Woods K, et al. Minimizing recurrent peptic ulcer hemorrhage after endoscopic hemostasis: the cost-effectiveness of competing strategies. Am J Gastroenterol 2003 Jan; 98 (1): 86–97
Leontiadis GI, Sharma VK, Howden CW. Systematic review and meta-analysis: proton-pump inhibitor treatment for ulcer bleeding reduces transfusion requirements and hospital stay. Results from the Cochrane Collaboration. Aliment Pharmacol Ther 2005 Aug 1; 22 (3): 169–74
Lau JY, Leung WK, Wu JC, et al. Omeprazole before endoscopy in patients with gastrointestinal bleeding. N Engl J Med 2007 Apr 19; 356 (16): 1631–40
Dorward S, Sreedharan A, Leontiadis GI, et al. Proton pump inhibitor treatment initiated prior to endoscopic diagnosis in upper gastrointestinal bleeding. Cochrane Database Syst Rev 2006; (4): CD005415
Enns RA, Gagnon YM, Rioux KP, et al. Cost-effectiveness in Canada of intravenous proton pump inhibitors for all patients presenting with acute upper gastrointestinal bleeding. Aliment Pharmacol Ther 2003 Jan; 17 (2): 225–33
Tsoi KK, Lau JY, Sung JJ. Cost-effectiveness analysis of high-dose omeprazole infusion before endoscopy for patients with upper-GI bleeding. Gastrointest Endosc 2008 Jun; 67 (7): 1056–63
Barkun AN. Should every patient with suspected upper GI bleeding receive a proton pump inhibitor while awaiting endoscopy? Gastrointest Endosc 2008 Jun; 67 (7): 1064–6
Sung JJY, Barkun A, Kuipers EJ, et al. Letter of reply to all correspondents [online]. Available from URL: http://www.annals.org/cgi/eletters/150/7/455#114442 [Accessed 2009 Oct 1]
Hearnshaw S, Logan R, Murphy M, et al. Results of the UK audit of 6750 patients with acute upper gastrointestinal haemorrhage. Gut. In press
Erstad BL. Cost-effectiveness of proton pump inhibitor therapy for acute peptic ulcer-related bleeding. Crit Care Med 2004 Jun; 32 (6): 1277–83
Spiegel BM, Ofman JJ, Woods K, et al. Minimizing recurrent peptic ulcer hemorrhage after endoscopic hemostasis: the cost-effectiveness of competing strategies. Am J Gastroenterol 2003 Jan; 98 (1): 86–97
Bala MV, Zarkin GA. Are QALYs an appropriate measure for valuing morbidity in acute diseases? Health Econ 2000 Mar; 9 (2): 177–80
Acknowledgements
Funding for this study was provided by AstraZeneca, who also had an advisory input into the design of the study, collected the data, monitored the conduct of the study, performed the statistical analyses and coordinated the writing of the manuscript with all authors.
Alan Barkun, Ernst Kuipers, Joachim Mössner, Robert Stuart, James Lau, Dennis Jensen and Joseph Sung acted as consultants for AstraZeneca for which they received payment, and E. Nauclér, J. Kilhamn, H. Granstedt, B. Liljas and T. Lind are employees of AstraZeneca.
The authors thank Richard Glover (inScience Communications, Chester, UK) who provided editorial assistance funded by AstraZeneca. All authors contributed to the various drafts and revisions and all approved the final manuscript. AstraZeneca had the opportunity to review the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Barkun, A.N., Adam, V., Sung, J.J.Y. et al. Cost Effectiveness of High-Dose Intravenous Esomeprazole for Peptic Ulcer Bleeding. Pharmacoeconomics 28, 217–230 (2010). https://doi.org/10.2165/11531480-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11531480-000000000-00000