Abstract
Objectives: To assess trends in prescriptions, determinants and timing of treatment discontinuation and/or changes in antihypertensive drug therapy in a cohort of hypertensive patients living in Pavia, a city in the north of Italy.
Methods: The cohort included 61 493 patients aged ≥18 years who received their first antihypertensive drug prescription (monotherapy, fixed or extemporaneous combination) during the period 2003–6. Patients were classified as ‘persistent’ if 12 months after the beginning of treatment they were still taking a regular therapy (same drug = ‘same therapy users’, added one or more drugs = ‘add-on therapy users’, different drug = ‘switchers’). Otherwise, they were classified as ‘non-persistent’ (stopping therapy after the first prescription = ‘occasional users’; stopping treatment early = ‘stoppers’; taking medicines in an erratic fashion = ‘intermittent users’).
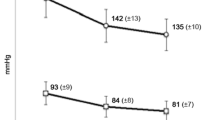
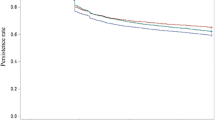
Results: ACE inhibitors were the most frequently prescribed drugs (22.8%), followed by β-adrenoceptor antagonists (β-blockers) [14.3%], diuretics (13.9%), Ca2+ antagonists (11.4%) and angiotensin II type 1 receptor antagonists (angiotensin receptor blockers [ARBs]) [9.3%]. After 12 months, persistent patients were only 11.2% (same therapy users 6.7%, switchers 3.2%, add-on therapy users 1.3%). Non-persistent patients were 88.8% (35.3% occasional users, 20.6% stoppers, 32.8% intermittent users). Patient-related predictors of persistence were older age, male sex, concomitant treatment with antidiabetic and hypolipidaemic drugs and previous hospitalizations for cardiovascular events. Highest level of persistence was seen in patients starting with ARBs (18.8%), followed by ACE inhibitors (11.4%), β-blockers (11.0%), Ca2+ antagonists (10.8%) and diuretics (3.0%). Among ARBs, considering separately monotherapy and fixed-combination therapy, highest level of persistence was observed in patients starting with candesartan, irbesartan, valsartan and telmisartan given in monotherapy, and with valsartan and telmisartan given in fixed-dose combination.
Conclusions: Persistence to antihypertensive treatment at 12 months is only 11.2%, being the lowest with diuretics (3.0%) and the highest with ARBs (18.8%).










Similar content being viewed by others
References
Psaty BM, Lumley T, Furberg CD, et al. Health outcomes associated with various antihypertensive therapies used as first-line agents: a network meta-analysis. JAMA 2003; 289: 2534–44
Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood pressure lowering regimens on major cardiovascular events: second cycle of prospectively designed overviews. Lancet 2003; 362: 1527–35
Chalmers J. Comparison of various blood pressure lowering treatments on the primary prevention of cardiovascular outcomes in recent randomised clinical trials. Clin Exp Hypertens 2004; 26: 709–19
Turnbull F, Neal B, Ninomiya T, et al. Effects of different regimens to lower blood pressure on major cardiovascular events in older and younger adults: meta-analysis of randomised trials. Blood Pressure Lowering Treatment Trialists’ Collaboration. BMJ 2008; 336 (7653): 1121–3
Wolf-Maier K, Cooper RS, Banegas JR, et al. Hypertension prevalence and blood pressure levels in 6 European Countries, Canada, and the United States. JAMA 2003; 289 (18): 2363–9
Kotseva K, Wood D, De Backer D, et al., for the EUROASPIRE Study Group. Cardiovascular prevention guidelines in daily practice: a comparison of EUROASPIRE I, II, and III surveys in eight European countries. Lancet 2009; 373: 929–40
Eni C, Okonofua EC, Simpson KN, et al. Therapeutic inertia is an impediment to achieving the Healthy People 2010. Blood Pressure Control Goals Hypertens 2006; 47: 345–51
Fujita T, Shimamoto K, Wu Z, et al. What are the major challenges in getting patients to the optimal BP goal? Difficulties in educating doctors and patients. Int J Clin Pract Suppl 2006; 150: 20–2
Costa FV. Compliance with antihypertensive treatment. Clin Exp Hypertens 1996 Apr-May; 18 (3-4): 463–72
Burnier M. Medication adherence and persistence as the cornerstone of effective antihypertensive therapy. Am J Hypertens 2006; 19: 1190–6
Lopatriello S, Berto P, Cramer J, et al. Different aspects of adherence to antihypertensive treatments [abstract]. Expert Rev Pharmacoeconomics Outcomes Res 2004; 4 (3): 317–33
Hyre AD, Krousel-Wood MA, Muntner P, et al. Prevalence and predictors of poor antihypertensive medication adherence in an urban health clinic setting. J Clin Hypertens (Greenwich) 2007 Mar; 9 (3): 179–86
Degli Esposti L, Degli Esposti E, Valpiani G, et al. A retrospective, population-based analysis of persistence with antihypertensive drug therapy in primary care practice in Italy. Clin Ther 2002 Aug; 24 (8): 1347–57
Degli Esposti E, Sturani A, Di Martino M, et al. Long-term persistence with antihypertensive drugs in new patients. J Hum Hypertens 2002; 16: 439–44
Mazzaglia G, Mantovani L, Sturkenboom MC, et al. Patterns of persistence with antihypertensive medications in newly diagnosed hypertensive patients in Italy: a retrospective cohort study in primary care. J Hypertens 2005; 23: 2093–100
Bourgault C, Senecal M, Brisson M, et al. Persistence and discontinuation patterns of antihypertensive therapy among newly treated patients: a population-based study. J Hum Hypertens 2005 Aug; 19 (8): 607–13
Corrao G, Zambon A, Parodi A, et al. Discontinuation of and changes in drug therapy for hypertension among newly-treated patients: a population-based study in Italy. J Hypertens 2008 Apr; 26 (4): 819–24
Costa FV, D’Ausilio A, Bianchi C, et al. Adherence to antihypertensive medications: a review and update. High Blood Pressure Cardiovasc Prev 2009 Sep; 16 (3): 101–10
Catalan VS, LeLorier J. Predictors of long-term persistence on statins in a subsidized clinical population. Value Health 2000 Nov-Dec; 3 (6): 417–26
Elliott WJ, Plauschinat CA, Skrepnek GH, et al. Persistence, adherence, and risk of discontinuation associated with commonly prescribed antihypertensive drug monotherapies. J Am Board Fam Med 2007; 20: 72–80
Hasford J, Mimran A, Simons WR. A population-based European cohort study of persistence in newly diagnosed hypertensive patients. J Hum Hypertens 2002; 16: 569–75
Erkens JA, Panneman MM, Klungel OH, et al. Differences in antihypertensive drug persistence associated with drug class and gender: a PHARMO study. Pharmacoepidemiol Drug Saf 2005 Nov; 14 (11): 795–803
Haynes RB, McDonald HP, Garg AX. Helping patients follow prescribed treatment: clinical applications. JAMA 2002; 288: 2880–3
Wolf-Maier K, Cooper RS, Kramer H, et al. Hypertension treatment and control in five European countries, Canada, and the United States. Hypertension 2004; 43: 10–7
Kettani FZ, Dragomir A, Côté R et al. Impact of a better adherence to antihypertensive agents on cerebrovascular disease for primary prevention. Stroke 2009; 40: 213–20
Breekveldt-Postma NS, Penning-van Beest FJA, Siiskonen SJ, et al. The effect of discontinuation of antihypertensives on the risk of acute myocardial infarction and stroke. Curr Med Res Opin 2008; 24: 121–7
Sokol MC, McGuigan KA, Verbrugge RR, et al. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care 2005; 43: 521–30
American Heart Association. High blood pressure 2009 [online]. Available from URL: http://www.americanheart.org/presenter.jhtml?identifier=2139 [Accessed 2009 Sep 15]
Hansson L, Lloyd A, Anderson P, et al. Excess morbidity and cost of failure to achieve targets for blood pressure control in Europe. Blood Press 2002; 11 (1): 35–45
Gaziano TA, Bitton A, Anand S, et al. The global cost of non optimal blood pressure. J Hypertens 2009; 27: 1472–7
Falaschetti E, Chaudhury M, Mindell J, et al. Continued improvement in hypertension management in England: results from the Health Survey for England 2006. Hypertension 2009; 53: 480–6
Theodoratou D, Maniadakis N, Fragoulakis V, et al. Analysis of published economic evaluations of angiotensin receptor blockers. Hellenic J Cardiol 2009; 50: 105–18
Poluzzi E, Strahinja P, Vargiu A, et al. Initial treatment of hypertension and adherence to therapy in general practice in Italy. Eur J Clin Pharmacol 2005; 61: 603–9
Acknowledgements
This study was funded by Boehringer Ingelheim Italia. For all authors, there is no conflict of interest and there are no persons who contributed to the work who do not meet the criteria for authorship.
Author information
Authors and Affiliations
Corresponding author
Additional information
† Population-Based Analysis of PErsistence with Treatment and Economics of TElmisartan Study.
Rights and permissions
About this article
Cite this article
Costa, F.V., Esposti, L.D., Cerra, C. et al. Trends in Prescription and Determinants of Persistence to Antihypertensive Therapy. High Blood Press Cardiovasc Prev 16, 167–176 (2009). https://doi.org/10.2165/11530410-000000000-00000
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.2165/11530410-000000000-00000