Abstract
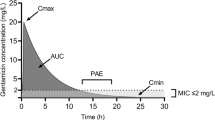
The appropriate dosage of antibacterial agents is essential in achieving both clinical and microbiologic success in the treatment of infections in children. By using in vitro experimental data and animal model outcome data, the pharmacokinetic-pharmacodynamic (PK-PD) parameters predictive of antibacterial effect have been elucidated. For time-dependent drugs such as β-lactams, the PK-PD parameter of interest is the percentage of time in a dosage interval for which drug concentrations remain above the minimum inhibitory concentration (MIC) of the infecting organism. For concentration-dependent drugs such as aminoglycosides, the PK-PD parameter of interest is the ratio of the area under the plasma concentration-time curve to the MIC. Recent studies using data on clinical and microbiologic outcomes from infected adults and children, combined with data on drug exposure, have confirmed the importance of these parameters and provided estimates of the PK-PD goals of therapy for various antibacterial agents. Application of these PK-PD principles allows rational dosage regimen selection, both for serious infections in critically ill children and for non-life-threatening community-acquired infections.




Similar content being viewed by others
References
Ambrose PG, Anon JB, Owen JS, et al. Use of pharmacodynamic end points in the evaluation of gatifloxacin for the treatment of acute maxillary sinusitis. Clin Infect Dis 2004; 38(11): 1513–20
Jumbe N, Louie A, Leary R, et al. Application of a mathematical model to prevent in vivo amplification of antibiotic-resistant bacterial populations during therapy. J Clin Invest 2003; 112(2): 275–85
Guillemot D, Carbon C, Balkau B, et al. Low dosage and long treatment duration of beta-lactam: risk factors for carriage of penicillin-resistant Streptococcus pneumoniae. JAMA 1998; 279: 365–70
Eagle H, Fleischman R, Levy M. “Continuous” vs. “discontinuous” therapy with penicillin: the effect of the interval between injections on therapeutic efficacy. New Engl J Med 1953; 248: 481–8
Dudley MN, Ambrose PG. Pharmacodynamics in the study of drug resistance and establishing in vitro susceptibility breakpoints: ready for prime time. Curr Opin Microbiol 2000; 5: 515–21
Forrest A, Nix DE, Ballow CH, et al. Pharmacodynamics of intravenous ciprofloxacin in seriously ill patients. Antimicrob Agents Chemother 1993; 37: 1073–81
Drusano GL, Preston SL, Fowler C, et al. Relationship between fluoroquinolone AUC: MIC ratio and the probability of eradication of the infecting pathogen in patients with nosocomial pneumonia. J Infect Dis 2004; 189: 1590–7
Craig WA. Pharmacodynamics of antimicrobials: general concepts and applications. In: Nightingale CH, Murakawa T, Ambrose PG, editors. Antimicrobial pharmacodynamics in theory and clinical practice. New York (NY): Marcel Dekker, Inc., 2002: 1–22
Lodise TP, Preston S, Bhargava V, et al. Pharmacodynamics of an 800-mg dose of telithromycin in patients with community-acquired pneumonia caused by extracellular pathogens. Diagn Microbiol Infect Dis 2005; 52: 45–52
Ambrose PG, Bhavnani SM, Owens RC. Clinical pharmacodynamics of quinolones. Infect Dis Clinics of North Am 2003; 17: 529–43
Bhavnani SM, Passarell JA, Owen JS, et al. Pharmacokinetic-pharmacodynamic relationships describing the efficacy of oritavancin in patients with Staphylococcus aureus bacteremia. Antimicrob Agents Chemother 2006; 50: 994–1000
Rayner CR, Forrest A, Meagher AK, et al. Clinical pharmacodynamics of linezolid in seriously ill patients treated in a compassionate use program. Clin Pharmacokinet 2003; 42: 1411–23
Ebert SC, Craig WA. Killing and re-growth of bacteria in vitro: a review. Scand J Infect Dis Suppl 1991; 74: 63–70
Ambrose PG, Bhavnani SM, Rubino CM, et al. Pharmacokinetics-pharmacodynamics of antimicrobial therapy: it’s not just for mice anymore. Clin Infect Dis 2007; 44: 79–86
Craig WA. Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin Infect Dis 1998; 26: 1–12
Moore RD, Lietman PS, Smith CR. Clinical response to aminoglycoside therapy: importance of the ratio of peak concentration to minimal inhibitory concentration. J Infect Dis 1987; 155: 93–9
Kashuba AD, Nafziger AN, Drusano GL, et al. Optimizing aminoglycoside therapy for nosocomial pneumonia caused by gram-negative bacteria. Antimicrob Agents Chemother 1999; 43(3): 623–9
Bertino Jr JS, Booker LA, Franck PA, et al. Incidence of and significant risk factors for aminoglycoside-associated nephrotoxicity in patients dosed by using individualized pharmacokinetic monitoring. J Infect Dis 1993; 167(1): 173–9
Sanchez-Alcaraz A, Vargas A, Quintana MB, et al. Therapeutic drug monitoring of tobramycin: once-daily versus thrice-daily dosage schedules. J Clin Pharm Ther 1998; 23: 367–73
van Lent-Evers NA, Mathot RA, Geus WP, et al. Impact of goal-oriented and model-based clinical pharmacokinetic dosing of aminoglycosides on clinical outcome: a cost-effectiveness analysis. Ther Drug Monit 1999; 21(1): 63–73
Lacy MK, Nicolau DP, Nightingale CH, et al. The pharmacodynamics of aminoglycosides. Clin Infect Dis 1998; 27: 23–7
Ali MZ, Goetz MB. A meta-analysis of the relative efficacy and toxicity of single daily dosing versus multiple daily dosing of aminoglycosides. Clin Infect Dis 1997; 24(5): 796–809
Bailey TC, Little JR, Littenberg B, et al. A meta-analysis of extended-interval dosing versus multiple daily dosing of aminoglycosides. Clin Infect Dis 1997; 24(5): 786–95
Bertino Jr JS, Rotschafer JC. Single daily dose of aminoglycosides: a concept whose time has not yet come. Clin Infect Dis 1997; 24(5): 820–3
Streetman DS, Nafziger AN, Destache CJ, et al. Individualized pharmacokinetic monitoring results in less aminoglycoside-associated nephrotoxicity and fewer associated costs. Pharmacotherapy 2001; 21: 443–51
Turnidge JD. The pharmacodynamics of beta-lactams. Clin Infect Dis 1998; 27: 10–22
Tam VH, McKinnon PS, Akins RL, et al. Pharmacokinetics and pharmacodynamics of cefepime in patients with various degrees of renal function. Antimicrob Agents Chemother 2003; 47(6): 1853–61
Burgess DS, Waldrep T. Pharmacokinetics and pharmacodynamics of piperacillin/tazobactam when administered by continuous infusion and intermittent dosing. Clin Therap 2002; 24(7): 1090–104
Krueger WA, Bulitta J, Kinzig-Schippers M, et al. Evaluation by Monte Carlo simulation of the pharmacokinetics of two doses of meropenem administered intermittently or as a continuous infusion in healthy volunteers. Antimicrob Agents Chemother 2005; 49(5): 1881–9
Pea F, Viale P, Damiani D, et al. Ceftazidime in acute myeloid leukemia patients with febrile neutropenia: helpfulness of continuous intravenous infusion in maximizing pharmacodynamic exposure. Antimicrob Agents Chemother 2005; 49(8): 3550–3
Bodey GP, Ketchel SJ, Rodriguez V. A randomized trial of carbenicillin plus cefamandole or tobramycin in the treatment of febrile episodes in cancer patients. Am J Med 1979; 67: 608–16
Craig WA, Andes DA. Correlation of the magnitude of the AUC24/MIC for six fluoroquinolones against Streptococcus pneumoniae with survival and bactericidal activity in an Animal Model [abstract no. 289] In: Abstracts of the 40th Interscience Conference of Antimicrobial Chemotherapy; 2000 Sep 17–20; Toronto (ON). Washington, DC: American Society of Microbiology, 2000
Meagher A, Passarell J, Cirincione B, et al. Exposure-response analysis of the efficacy of tigecycline in patients with complicated skin and skin structure infections [abstract]. 15th European Congress of Clinical Microbiology and Infectious Diseases; 2005 May 2–5; Copenhagen
Bhavnani SM, Rubino CM, Ambrose PG, et al. Pharmacokinetic-pharmacodynamic analyses of efficacy using estimates of serum and effect site tigecycline exposures in patients with complicated intra-abdominal infections [abstract]. 16th European Congress of Clinical Microbiology and Infectious Diseases; 2006 Apr 1–4; Nice
Mouton JW, Jacobs N, Tiddens H, et al. Pharmacodynamics of tobramycin in patients with cystic fibrosis. Diagn Microbiol Infect Dis 2005; 52: 123–7
Rubino CM, Caparelli EV, Bradley JS, et al. Population pharmacokinetic model for gatifloxacin in pediatric patients. Antimicrob Agents Chemother 2007; 51: 1246–52
Rubino CM, Ambrose PG, Cirincione B, et al. Pharmacokinetics and pharmacodynamics of gatifloxacin in children with recurrent otitis media: Application of sparse sampling in clinical development. Diagn Microbiol Infect Dis. In press
Craig WA, Andes D. Pharmacokinetics and pharmacodynamics of antibiotics in otitis media. Pediatr Infect Dis J 1996; 15(3): 255–9
Dagan R, Hoberman A, Johnson C, et al. Bacteriologic and clinical efficacy of high dose amoxicillin/clavulanate in children with acute otitis media. Pediatr Infect Dis J 2001; 20(9): 829–37
Dagan R, Klugman KP, Craig WA, et al. Evidence to support the rationale that bacterial eradication in respiratory tract infection is an important aim of antimicrobial therapy. J Antimicrob Chemother 2001; 47(2): 129–40
Elhanan K, Siplovich L, Raz R. Gentamicin once-daily versus thrice-daily in children. J Antimicrob Chemother 1995; 35: 327–32
de Alba Romero C, Gomez Castillo E, Manzanares Secades C, et al. Once daily gentamicin dosing in neonates. Pediatr Infect Dis J 1998; 17(12): 1169–71
Miron D. Once daily dosing of gentamicin in infants and children. Pediatr Infect Dis J 2001; 20(12): 1169–73
Smyth AR, Tan KH. Once-daily versus multiple-daily dosing with intravenous aminoglycosides for cystic fibrosis. Cochrane Database Syst Rev 2006 Jul 19; (3): CD002009
Rao SC, Ahmed M, Hagan R. One dose per day compared to multiple doses per day of gentamicin for treatment of suspected or proven sepsis in neonates. Cochrane Database Syst Rev 2006 Jan 25; (1): CD005091
Glover ML, Shaffer CL, Rubino CM, et al. A multicenter evaluation of gentamicin therapy in the neonatal intensive care unit. Pharmacother 2001; 21(1): 7–10
Blumer JL, Reed MD, Kaplan EL, et al. Explaining the poor bacteriologic eradication rate of single-dose ceftriaxone in group a streptococcal tonsillopharyngitis: a reverse engineering solution using pharmacodynamic modeling. Pediatr 2005; 116(4): 927–32
Kaplan EL, Johnson DR. Unexplained reduced microbiological efficacy of intramuscular benzathine penicillin G and of oral penicillin V in eradication of group a streptococci from children with acute pharyngitis. Pediatr 2001; 108: 1180–6
Lee J, Capparelli E, Bradley J. Once daily dosing of amoxicillin in pediatric patients with Group A streptococcus (GAS) pharyngitis using Monte Carlo simulation. Presented at the Western States Conference; 2004 May 24–25; Astlomar (CA)
Clegg HW, Ryan AG, Dallas SD, et al. Treatment of streptococcal pharyngitis with once-daily compared with twice-daily amoxicillin: a noninferiority trial. Pediatr Infect Dis J 2006; 25: 761–7
Capparelli E, Hochwald C, Rasmussen M, et al. Population pharmacokinetics of cefepime in the neonate. Antimicrob Agents Chemother 2005; 49: 2760–6
Pullen J, de Rozario L, Stolk LM, et al. Population pharmacokinetics and dosing of flucloxacillin in preterm and term neonates. Ther Drug Monit 2006; 28(3): 351–8
Capparelli E, Cannavino C, Rasmussen M, et al. Meropenem population pharmacokinetics in infants: developmental changes in elimination [abstract no. G-851]. In: Abstracts of the 46th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2006 Sep 17–20; San Francisco (CA): Washington, DC: American Society of Microbiology, 2006
van Enk JG, Touw DJ, Lafeber HN. Pharmacokinetics of meropenem in preterm neonates. Ther Drug Monit 2001; 23: 198–201
Giannoni E, Moreillon P, Cotting J, et al. Prospective determination of plasma imipenem concentrations in critically ill children. Antimicrob Agents Chemother 2006; 50: 2563–8
Ambrose PG, Bhavnani SM, Jones RN, et al. Use of pharmacokinetics-pharmacodynamics and Monte Carlo simulation as decision support for the re-evaluation of NCCLS cephem susceptibility breakpoints for Enterobacteriaceae [abstract no. A-138]. In: Abstract of the 44th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2004 Oct 30–Nov 2; Washington, DC. Washington, DC: American Society of Microbiology, 2004
Block SL, Busman TA, Paris MM, et al. Comparison of five-day cefdinir treatment with ten-day low dose amoxicillin/clavulanate treatment for acute otitis media. Pediatr Infect Dis J 2004; 23: 834–8
Adler M, McDonald PJ, Trostmann U, et al. Cefdinir versus amoxicillin/clavulanic acid in the treatment of suppurative acute otitis media in children. Eur J Clin Microbiol Infect Dis 1997; 16: 214–9
Bowlware KL, McCracken Jr GH, Lozano-Hernandez J, et al. Cefdinir pharmacokinetics and tolerability in children receiving 25 mg/kg once daily. Pediatr Infect Dis J 2006; 25: 208–10
Marchant CD, Carlin SA, Johnson CE, et al. Measuring the comparative efficacy of antibacterial agents for acute otitis media: the “Pollyanna phenomenon”. J Pediatr 1992; 120: 72–7
Rosenfeld RM, Kay DJ. Clinical efficacy of medical therapy. In Rosenfeld RM, Bluestone CD, editors. Evidence-based otitis media. Hamilton (ON): B.C. Decker, Inc., 2003: 199–226
Jacobs MR, Dagan R, Singer ME. Study design questions in treatment of children with acute otitis media. Antimicrob Agents Chemother 2004; 48: 2784–6
United States Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research. Guidance for industry. Acute otitis media: developing antimicrobial drugs for treatment. 1998 [online]. Available from URL: http://www.fda.gov/cder/guidance/2617dft.pdf [Accessed 2007 May 17]
Arrieta A, Arguedas A, Fernandez P, et al. High-dose azithromycin versus high-dose amoxicillin-clavulanate for treatment of children with recurrent or persistent acute otitis media. Antimicrob Agents Chemother 2003; 47: 3179–86
Dunne MW, Khurana C, Arguedas A, et al. Efficacy of single-dose azithromycin in treatment of acute otitis media in children after a baseline tympanocentesis. Antimicrob Agents Chemother 2003; 47: 2663–5
Aronovitz G. A multicenter, open label trial of azithromycin vs. amoxicillin/clavulanate for the management of acute otitis media in children. Pediatr Inf Dis J 1996; 15: S15–9
Hoberman A, Dagan R, Leibovitz E, et al. Large dosage amoxicillin/clavulanate, compared with azithromycin, for the treatment of bacterial acute otitis media in children. Pediatr Inf Dis J 2005; 24: 525–32
Hoberman A, Marchant CD, Kaplan SL, et al. Treatment of acute otitis media consensus recommendations. Clin Pediatr 2002; 41(6): 373–90
Anon JB, Jacobs MR, Poole MD et al., on behalf of the Sinus And Allergy Health Partnership. Antimicrobial treatment guidelines for acute bacterial rhinosinusitis. Otolaryngol Head Neck Surg 2004; 130Suppl. 1: 1–45
Acknowledgments
The authors would like to acknowledge the scientific contributions of Paul G. Ambrose to the preparation of this review. No sources of funding were used to assist in the preparation of this review. Christopher Rubino has previously received honoraria from Bristol-Myers Squibb for attending their pediatric advisory boards. While an employee of Cognigen Corporation, he received grants to conduct pediatric PK-PD analyses of data from the pediatric development program for gatifloxacin. John Bradley has no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rubino, C.M., Bradley, J.S. Optimizing Therapy with Antibacterial Agents. Pediatr Drugs 9, 361–369 (2007). https://doi.org/10.2165/00148581-200709060-00003
Published:
Issue Date:
DOI: https://doi.org/10.2165/00148581-200709060-00003