Abstract
Background
β-Adrenoceptor antagonist (β-blocker) therapy results in a significant improvement in left ventricular (LV) systolic function and prognosis in patients with chronic heart failure. Both carvedilol and nebivolol produce hemodynamic and clinical benefits in chronic heart failure, but it is unknown whether their peculiar pharmacologic properties produce different effects on LV function.
Objective
To assess the effects on LV function of nebivolol compared with carvedilol in patients with chronic heart failure and reduced LV systolic function.
Methods
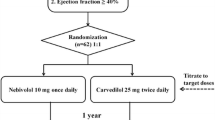
Seventy patients with a LV ejection fraction ≤40% and in New York Heart Association (NYHA) functional class II or III were randomly assigned to receive carvedilol or nebivolol therapy for 6 months. At baseline and after 6 months of treatment, all patients were assessed clinically and by biochemical and hematological investigation, ECG, 24-hour Holter monitoring, echocardiogram, measurement of ventilatory function, and a 6-minute walk test.
Results
Compared with baseline values LV end-systolic volume decreased and LV ejection fraction increased in both the carvedilol (from 79 ± 38mL to 73 ± 43mL and from 33% ± 6% to 37% ± 11%) and the nebivolol group (from 72 ± 35mL to 66 ± 32mL and from 34% ± 7% to 38% ± 10%), although the between-group differences were not statistically significant. ECG data showed a decrease in resting HR in both groups (from 83 ± 20 bpm to 66 ± 11 bpm for carvedilol and from 81 ± 15 bpm to 65 ± 11 bpm for nebivolol; p < 0.001 vs baseline for both groups) but no difference in the PQ, QRS, and QT intervals. Hematologic (in particular, N-terminal pro-brain natriuretic peptide), Holter monitoring (with the exception of HR), and respiratory functional data did not show any significant variation in either group after 6 months’ therapy. SBP and DBP decreased in both groups. A small reduction in mean NYHA functional class from baseline was seen in both groups (from 2.5 ± 0.5 to 2.2 ± 0.5 for carvedilol [p < 0.05] and from 2.3 ± 0.4 to 2.2 ± 0.5 for nebivolol [not significant]). The 6-minute walk test showed a trend toward an increase in the walking distance in both groups. During 6 months of treatment no significant differences in adverse events were observed between the groups.
Conclusion
Nebivolol is as effective as carvedilol in patients with symptomatic chronic heart failure and reduced LV systolic function.




Similar content being viewed by others
References
Packer M, Bristow MR, Cohn JN, et al., on behalf of The US Carvedilol Heart Failure Study Group. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. N Engl J Med 1996; 334: 1349–55.
CIBIS II Investigators and Committees. The Cardiac Insufficiency Bisoprolol Study II (CIBIS II): a randomized trial. Lancet 1999; 353: 9–13.
Cockroft JR, Chowenczyk PHJ, Brett SE, et al. Nebivolol vasodilates human forearm vasculature: evidence for L-arginin/NO dependent mechanism. J Pharmacol Exp Ther 1995; 274: 1067–71.
Brehm BR, Wolf SC, Bertsch D, et al. Effects of nebivolol on proliferation and apoptosis on human coronary artery smooth muscle and endothelial cells. Cardiovasc Res 2001; 49: 430–9.
Brehm BR, Wolf SC, Görner S, et al. Effect of nebivolol on left ventricular function in patients with chronic heart failure: a pilot study. Eur J Heart Fail 2002; 4: 757–63.
Wolf SC, Buck-Muller N, Gorner S, et al. Influence of the beta-blocker nebivolol on the left ventricular function in patients with chronic heart failure. Med Klin 2003; 98: 1–6.
Brune S, Schmidt T, Tebbe U, et al. Hemodynamic effects of nebivolol at rest and on exertion in patients with heart failure. Angiology 1990; 4: 696–701.
Nodari S, Metra M, Dei Cas L. Beta-blocker treatment of patients with diastolic heart failure and arterial hypertension: a prospective, randomized, comparison of the long-term effects of atenolol vs nebivolol. Eur J Heart Fail 2003; 5: 621–7.
Schiller NB, Shah PM, Crawford M, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. J Am Soc Echocardiogr 1989; 2(5): 358–67.
Quinones MA, Otto CM, Stoddard M, et al. Recommendations for quantification of Doppler echocardiography: a report from the Doppler Quantification Task Force of the Nomenclature and Standards Committee of the American Society of Echocardiography. J Am Soc Echocardiogr 2002; 15: 167–84.
The MERIT-HF Investigators. Effect of metoprolol CR/XL in chronic heart failure: metoprolol CR/XL randomised intervention trial in congestive heart failure (MERIT-HF). Lancet 1999; 353: 2001–7.
Mangrella M, Rossi F, Fici F, et al. Pharmacology of nebivolol. Pharmacol Res 1998; 38: 419–31.
Uhlir O, Dvorak I, Gregor P, et al. Nebivolol in the treatment of cardiac failure: a double-blind controlled clinical trial. J Card Fail 1997; 3(4): 271–6.
Evdokimova AG, Radzevich AE, Tereshchenko OI, et al. Nebivolol in the treatment of ischemic heart disease patients with chronic heart failure. Kardiologiia 2004; 44(2): 15–8.
Gromnatskii NI, Dius’mikeeva NB. Effect of nebivolol on remodelling of the heart and vessels and the state of hemodynamics in patients with hypertension. Kardiologiia 2002; 42: 27–30.
Rousseau MF, Chapelle F, Van Eyll C, et al. Medium-term effects of beta-blockade on left ventricular mechanics: a double-blind, placebo-controlled comparison of nebivolol and atenolol in patients with ischemic left ventricular dysfunction. J Card Fail 1996; 2(1): 15–23.
Wisenbaugh T, Katz I, Davis J, et al. Long term (3 month) effects of a new beta-blocker (nebivolol) on cardiac performance in dilated cardiomyopathy. J Am Coll Cardiol 1993; 21: 1094–100.
Kamp O, Sieswerda GT, Visser CA. Comparison of effects on systolic and diastolic left ventricular function of nebivolol versus atenolol in patients with uncomplicated essential hypertension. Am J Cardiol 2003; 92: 344–8.
Bristow MR, Roden RL, Lowes BD, et al. The role of third generation β-blocking agents in chronic heart failure. Clin Cardiol 1998; 21 Suppl. I: 3S–13S.
Acknowledgments
No sources of funding were used to assist in the conduction of this study. The authors have no conflicts of interest that are directly relevant to the content of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lombardo, R.M.R., Reina, C., Abrignani, M.G. et al. Effects of Nebivolol versus Carvedilol on Left Ventricular Function in Patients with Chronic Heart Failure and Reduced Left Ventricular Systolic Function. Am J Cardiovasc Drugs 6, 259–263 (2006). https://doi.org/10.2165/00129784-200606040-00006
Published:
Issue Date:
DOI: https://doi.org/10.2165/00129784-200606040-00006