Abstract
Background
Diabetes self-management education (DSME) is a critical component of the clinical management of diabetes mellitus. Although DSME is recognized as important, the number of patients with diabetes who receive education is disproportionately small. Several barriers to receiving diabetes education exist, including access and DSME delivery approaches.
Objective
The purpose of this project was to explore opportunities to meet the Healthy People 2010 goal of increasing the proportion of people with diabetes mellitus who receive diabetes education from 40% (as it was in 1998) to 60% (in 2010). Our objectives were to examine the provision of DSME in primary care, to determine if DSME delivery in primary care increases the number of people who receive DSME, and to evaluate the effect of DSME on glycosylated hemoglobin (HbA1c) and low-density lipoprotein-cholesterol (LDL-C) levels. DSME was delivered in primary care practices as part of the Pittsburgh Regional Initiative for Diabetes Education (PRIDE).
Research design and methods
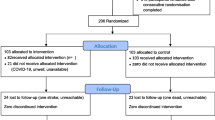
A nurse who was a certified diabetes educator (CDE) was deployed to provide Point-Of-Service diabetes Education (POSE) to four University of Pittsburgh Medical Center (UPMC) Community Medicine Practices (CMI) primary care practices. The group of patients who received POSE was compared with patients from the same practices who were identified as having diabetes and who received usual care. The number of patients was computed and a percentage calculated for comparison against Healthy People 2010 goals. The HbA1c values of patients were tracked from January 2003 through December 2006, during the timeframe that POSE was provided.
Results
Of the 5344 diabetes patients in the four practices, 784 received POSE. Mean HbA1c values were higher at baseline in those patients who received POSE than those who received usual care. There was a significant decrease in HbA1c and LDL-C levels in both groups. Although there was not a significant between-group difference in HbA1c, those who received POSE had significant improvement in LDL-C levels compared with the usual care group.
Conclusions
Providing DSME in primary care is feasible and offers the opportunity to reach patients who may not be receiving DSME services. However, further research is needed to evaluate other methodologies to increase access to DSME and other factors that may influence improvement in clinical outcomes.



Similar content being viewed by others
References
Zgibor JC, Peyrot M, Ruppert K, et al. Using the American Association of Diabetes Educators Outcomes System to identify patient behavior change goals and diabetes educator responses. Diabetes Educ 2007; 33(5): 839–42
Norris SL, Engelgau MM, Narayan KMV. Effectiveness of self-management training in type 2 diabetes. Diabetes Care 2001; 24(3): 561–87
Brown AS. Interventions to promote diabetes self-management: state of the science. Diabetes Educ 1999; 25 Suppl.: 52–61
US Department of Health and Human Services. Healthy people 2010: understanding and improving health. Washington, DC: US Department of Health and Human Services, Government Printing Office, 2000
Hiss RG, Anderson RM, Hess GE, et al. Community diabetes care: a 10-year perspective. Diabetes Care 1994; 17(10): 1124–34
Coonrod BA, Betschart J, Harris MI. Frequency and determinants of diabetes patient education among adults in the US population. Diabetes Care 1994; 17(8): 852–8
Pearson J, Mensing C, Anderson R. Medicare reimbursement and diabetes self-management training: national survey results. Diabetes Educ 2004; 30(6): 914–27
Siminerio L, Piatt G, Zgibor J. Implementing the chronic care model in a rural practice. Diabetes Educ 2005; 31(2): 225–34
Zgibor JC, Rao H, Wesche-Thobaben J, et al. Improving the quality of diabetes care in primary care practice. J Healthc Qual 2004; 26(4): 14–21
Suhl E, Bonsignore P. Diabetes self-management education for older adults: general principles and practical application. Diabetes Spectrum 2006; 19: 234–40
Janes GR. Ambulatory medical care for diabetes. In: Harris M, Cowie C, Stern M, et al., editors. Diabetes in America. Vol. 95–1468. Bethesda (MD): National Institutes of Health, 1995: 541–52
Glasgow RE, Toobert DJ, Hampson SE, et al. A brief office-based intervention to facilitate diabetes self-management. Health Educ Res 1995; 10(4): 467–78
Glasgow R, Eakin E. Medical-office based interventions. In: Snoek F, Skinner C, editors. Psychology in diabetes care. Hoboken (NJ): Wiley and Sons, Ltd: 141-68
Piatt GA, Orchard TJ, Emerson S, et al. Translating the chronic care model into the community: results from a randomized controlled trial of a multi-faceted diabetes care intervention. Diabetes Care 2006; 29(4): 811–7
Siminerio LM, Piatt GA, Emerson S, et al. Deploying the chronic care model to implement and sustain diabetes self-management training programs. Diabetes Educ 2006; 32(2): 253–60
Siminerio L, Zgibor J, Solano FX. Implementing the chronic care model for improvements in diabetes practice and outcomes in primary care: the University of Pittsburgh Medical Center experience. Clinical Diabetes 2004; 22(2): 54–8
American Diabetes Association. Standards of medical care for patients with diabetes (position statement). Diabetes Care 1999; 22 Suppl. 1: S32–41
Funnell M, Brown T, Childs B, et al. National standards for diabetes self-management education. Diabetes Care 2007; 30(6): 1630–7
Anderson RM, Fitzgerald JT, Gorenflo DW, et al. A comparison of the diabetesrelated attitudes of health care professionals and patients. Patient Educ Couns 1993; 21(1–2): 41–50
Larme AC, Pugh JA. Attitudes of primary care providers toward diabetes: barriers to guideline implementation. Diabetes Care 1998; 21(9): 1391–6
Zgibor JC, Songer TJ. External barriers to diabetes care: addressing personal and health systems issues. Diabetes Spectrum 2001; (14): 23–8
Beaven DW, Scott RS. The organisation of diabetes care. In: Alberti KGMM, Krall LP, editors. The diabetes annual: 2. New York: Elsevier, 1986: 39–48
Orlandi MA. Promoting health and preventing disease in health care settings: an analysis of barriers. Prev Med 1987; 16(1): 119–30
Siminerio LM, Funnell MM, Peyrot M, et al. US nurses’ perceptions of their role in diabetes care: results of the cross-national Diabetes Attitudes Wishes and Needs (DAWN) study. Diabetes Educ 2007; 23(1): 152–62
Lorig KR, Mazonson PD, Holman HR. Evidence suggesting that health education for self-management in patients with chronic arthritis has sustained health benefits while reducing health care costs. Arthritis Rheum 1993; 36(4): 439–46
Leveille SG, Wagner EH, Davis C, et al. Preventing disability and managing chronic illness in frail older adults: a randomized trial of a community-based partnership with primary care. J Am Geriatr Soc 1998; 46(10): 1191–8
Glasgow RE. A practical model of diabetes management and education. Diabetes Care 1995; 18(1): 117–26
Acknowledgments
Portions of this research were sponsored by funding from the US Air Force administered by the US Army Medical Research Acquisition Activity, Fort Detrick, MD, USA (award number W81XWH-04-2-003). Review of material does not imply Department of the Air Force endorsement of factual accuracy or opinion.
Sharlene Emerson is part of the diabetes education network for Eli Lilly, Inc. Dr Piatt has received honoraria from Johnson & Johnson. Dr Siminerio has received honoraria from Eli Lilly, Amylin, Sanofi Aventis, and Merck. Dr Solano has received honoraria from Sanofi Aventis. Dr Ruppert has no conflicts of interest that are directly relevant to the contents of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Siminerio, L.M., Ruppert, K., Emerson, S. et al. Delivering Diabetes Self-Management Education (DSME) in Primary Care. Dis-Manage-Health-Outcomes 16, 267–272 (2008). https://doi.org/10.2165/00115677-200816040-00007
Published:
Issue Date:
DOI: https://doi.org/10.2165/00115677-200816040-00007