Abstract
Background
Treatment for type 2 diabetes mellitus consists of dietary and exercise therapy, administration of oral hypoglycemic agents and insulin treatment for each stage. Compliance/adherence by patients to drug therapy and self care in their daily lives, not only in the stage of dietary and exercise therapy, but also after the start of drug therapy, are important factors. Disease management supporting self care may have a positive influence on the clinical management of diabetes. This study examined the effects of a disease management program implemented in the Yasugi-Nogi region of Shimane prefecture of Japan on clinical and behavioral aspects for type 2 diabetes in which intervention was implemented primarily by healthcare institutions.
Methods
The participants of this study consisted of 316 patients with diabetes. Routine care was provided based on the standards of care and standardized educational materials. Intervention was implemented by having patients set attainable goals with physicians and allied health professionals based on evaluations of their own lifestyle risks, and then using a diary to evaluate whether or not those goals were able to be attained. Evaluations were based on assessments of clinical parameters, patient behavior and health-related quality of life (HR-QOL).
Results
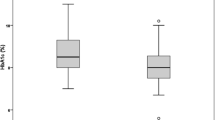
The results showed that significant improvement was observed in diastolic pressure, glycosylated hemoglobin (HbA1c) and triglyceride levels, regardless of the use of a diary. Improvement was also observed in diet and knowledge of diabetes, and improvement in HR-QOL was also observed, as assessed using the Problem Area in Diabetes Survey. A study of factors having an effect on the efficacy of disease management was conducted by focussing on HbA1c, diet score, knowledge score, and HR-QOL with respect to the type of treatment following intervention, diary use, and observence of physician guidance. In particular, the improvement in diet score was significantly better in the diary-user group.
Conclusion
The program employed in this region makes use of an easily deployable intervention method targeting diabetic patients with comparatively mild symptoms; therefore it is believed to be a realistic method for use as a disease management model led by physicians in regions where healthcare institutions play a central role.




Similar content being viewed by others
References
Disease Management Association of America (DMAA). Definition of disease management [online]. Available from URL: http://www.dmaa.org/definition.html/ [Accessed 2004 Sep 10]
The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993; 329: 977–86
Shichiri M, Kishikawa H, Ohkubo Y, et al. Long-term results of the Kumamoto Study on optimal diabetes control in type 2 diabetic patients. Diabetes Care 2000; 23 Suppl. 2: B21–9
The Diabetes Control and Complications Trial Research Group. Resource utilization and costs of care in the Diabetes Control and Complications Trial. Diabetes Care 1995; 18: 1468–78
Gillespie JL. The value of disease management. Part 2. atbalancing cost and quality in the treatment of diabetes mellitus. Dis Manag 2002; 5: 37–50
Rubin RJ, Dietrich KA, Hawk AD. Clinical and economic impact of implementing a comprehensive diabetes management program in managed care. J Clin Endocrinol Metab 1998; 83: 2635–42
Ministry of Health, Labour and Welfare. National diabetes survey [in Japanese]. Tokyo: Ministry of Health, Labour and Welfare: 1998 and 2003
Ministry of Health, Labour and Welfare. National medical expenditure [in Japanese]. Tokyo: Ministry of Health, Labour and Welfare: 2002
Ministry of Health, Labour and Welfare. National patient survey [in Japanese]. Tokyo: Ministry of Health, Labour and Welfare: 2002
Uchigata Y, Origasa H, Sakamaki H, et al. Health economic analysis for diabetic mellitus: examination of the relationship between diabetic complications and medical expenditure [in Japanese]. J Jpn Diabetes Society 1999; 42: 743–50
Sakamaki H, Kitaoka M, Taneda Y, et al. A study on cooperation between internists and ophthalmologists in regard to diabetic retinopathy: survey for the situation in the Nishi-Tokyo region [in Japanese]. Hospital Administration 2003; 40: 113–21
Lee ET, Keen H, Bennett PH, et al. Follow-up of the WHO Multinational Study of vascular disease in diabetes: general description and morbidity. Diabetologia 2001; 44 Suppl. 2: S3–13
Tajima N, Matsushima M, Baba S, et al. Japan. In: Eko JM, Zimmet P, Williams R, editors. The epidemiology of diabetes mellitus: an international perspective. Chichester: John Wiley & Sons, 2001
Campbell JC, Ikegami N. The art of balance in health policy: maintaining Japan’s low-cost, egalitarian system. Cambridge: Cambridge University Press, 1998
Todd WE, Nash D, ed. Disease management: a system approach to improving patient outcomes. San Francisco (CA): Jossey-Bass, 1996
Japan Diabetes Society. The food exchange list [in Japanese]. Bunkodo, Toyko: Japan Diabetes Association, 2002
Welch GW, Jacobson AM, Polonsky WH. The problem areas in diabetes scale: an evaluation of its clinical utility. Diabetes Care 1997; 20: 760–6
Ishii H, Furuya M, Okazaki K, et al. The Japanese version of problem area in diabetes scale: a clinical and research tool for the assessment of emotional functioning among diabetes patients [in Japanese]. J Jpn Diabetes Society 1999; 42: S262
Japanese EuroQol Translation Team. The development of the Japanese EuroQol instrument [in Japanese]. J Health Care Society 1997; 8: 109–23
Institute for Health Economics and Policy. Medical expenditure of the government-managed health insurance [in Japanese] [online]. Available from URL: https://www.ihep.jp/document/seikannkennpo.pdf [Accessed 2005 Nov 23]
Acknowledgments
This work was supported by a Health and Labor Science Research Grant from the Ministry of Health, Labour and Welfare Japan. The authors have no conflicts of interest that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sakamaki, H., Ikeda, S., Ikegami, N. et al. Clinical and Behavioral Impact of Implementing Community-Based Diabetes Disease Management in Japan. Dis-Manage-Health-Outcomes 14, 45–54 (2006). https://doi.org/10.2165/00115677-200614010-00006
Published:
Issue Date:
DOI: https://doi.org/10.2165/00115677-200614010-00006