Abstract
Disease management, a new treatment model that may improve outcomes for patients with chronic illness, emphasises the need for formal assessments often not included in traditional approaches to healthcare, such as environmental exposures, self-care skills and functional status. This article discusses the importance of these measures in designing a disease management programme for asthma and presents the results of a study of patients referred to this programme.
The objectives of the programme were to determine: (i) baseline functional status; (ii) any barriers to treatment; (iii) home exposure to patient-reported asthma triggers; and (iv) patients’ self-care skills. The proportion of referred patients who actually enrolled in the programme and, among those patients, the proportion who completed the prescribed educational component and attended the scheduled follow-up visits were also calculated. The investigators developed a structured assessment battery that included standardised measures of functioning; this battery was administered by clinical and research staff at enrolment and at 3- and 6-month follow-up.
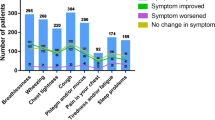
The patients (n = 228) had significantly lower functioning compared with the Medical Outcomes Study general US population norms and for patients with chronic lung disease. 71% (n = 127) of patients endorsed 1 or more of the 3 items on a depression screen. 85.5% of patients completed the 3 educational sessions; 104 of 228 patients (45.6%) returned for the 6-month follow-up visit.
This study contributes data about the design of disease management programmes and about asthma in inner city and minority patients, which are important topics in current research.
Similar content being viewed by others
References
Bottorff JL, Johnson JL, Ratner PA, et al. The effects of cognitiveperceptual factors on health promotion behavior maintenance. Nurs Res 1996; 45: 30–6
Fleetwood J, Packa DR. Determinants of health-promotion behaviors in adults. J Cardiovasc Nurs 1991; 5: 67–79
Kulbok PA, Baldwin JH. From preventive health behavior to health promotion: advancing a positive construct of health. ANS — Adv Nurs Sci 1992; 14: 50–64
Freundenberg N, Eng E, Flay B, et al. Strengthening individual and community capacity to prevent disease and promote health: in search of relevant theories and principles. Health Educ Q 1995; 22: 290–306
Mason JO, Koplan JP, Layde PM. The prevention and control of chronic diseases: reducing unnecessary deaths and disability: a conference report. Public Health Rep 1987; 102: 17–20
National Institutes of Health. Global Initiative for Asthma. Publication no. 95–365. Bethesda (MD): National Institutes of Health, 1995
Health Outcomes Institute. Asthma Type Specification, 1994
Neuhauser D, Headrick L, Miller DM. The best asthma care: a case problem in continuous quality improvement. Am J Med Qual 1992; 7: 76–80
Jones PK, Jones SL, Katz J. Improving compliance for asthmatic patients visiting the emergency department using a Health Belief Model intervention. J Asthma 1987; 24: 199–206
Tinkleman D, Flaum M, Lung CL. Take control of high cost asthma: turning patients into partners. Strategic Med 1997; 1: 42–51
Sullivan S, Elixhauser A, Buist AS, et al. National Asthma Education and Prevention Program working group report on the cost effectiveness of asthma care. Am J Respir Crit Care Med 1996; 154 Suppl. (3 Pt 2): 84–95
National Institutes of Health. International consensus report on diagnosis and management of asthma. National Heart, Lung and Blood Institute, Bethesda, MD. Eur Respir J 1992; 5: 601–41
National Institutes of Health. National asthma education program: expert panel report. Guidelines for the diagnosis and management of asthma. Bethesda (MD): National Heart, Lung, and Blood Institute, 1991: 1–136
Health Outcomes Institute. Health status questionnaire, 1993
National Institute of Mental Health. The center for epidemiological studies — depression scale. Bethesda (MD): National Institute of Mental Health, 1972
Nelson EC, Wasson JH, Johnson DJ, et al. The Dartmouth COOP functional health assessment charts: brief measures for clinical practice. In: Spilker B, editor. Quality of life and pharmacoeconomics in clinical trials. 2nd ed. Philadelphia (PA): Lippincott Raven Publishers, 1996
Ware Jr JE. The SF-36 Health Survey. Boston (MA): Medical Outcomes Trust, 1993
Rothman ML, Revicki DA. Issues in the measurement of health status in asthma research. Med Care 1993; 31(3 Suppl.): MS82–96
Richards JM, Hemstreet MP. Measures of life quality, role performance, and functional status in asthma research. Am J Respir Crit Care Med 1994; 149(2 Pt 2): S31–9, S40-3
Mahard RE. The CES-D as a measure of depressive mood in the elderly Puerto Rican population. J Gerontol 1988; 43: P24–5
Cho MJ, Moscicki EK, Narrow WE, et al. Concordance between two measures of depression in the hispanic health and nutrition examination survey. Soc Psychiatry Psychiatr Epidemiol 1993; 28: 156–63
Bosley, CM, Fosbury JA, Cochrane GM. The psychological factors associated with poor compliance with treatment in asthma. Eur Respir J 1995; 8: 899–904
Boulet LP, Chapman KR, Green LW, et al. Asthma education. Chest 1994; 106(4 Suppl.): 184S–196S
Tartasky D. Medicine use in an inner city asthmatic population. J Allergy Clin Immunol 1998; 101 (4 Pt 2)
Burnham MA, Wells KB, Leake B, et al. Development of a brief screening instrument for detecting depressive disorders. Med Care 1988; 16: 775–89
Magni G, Rossi MR, Rigatti-Luchini H, et al. Chronic abdominal pain and depression. Epidemiology findings in the United States. Hispanic health and nutrition examination survey. Pain 1992; 49: 77–85
Stout JW. The asthma outreach project: a promising approach to comprehensive asthma management. J Asthma 1998; 35: 119–37
Butler C, Rollnick S, Stott N. The practitioner, the patient and resistance to change: recent ideas on compliance. Can Med Assoc J 1996; 154: 1357–62
Morris LS, Schulz RM. Medication compliance — the patient’s perspective. Clin Ther 1993; 15: 593–606
Cochrane GM. Compliance and outcomes in patients with asthma. Drugs 1996; 6(52 Suppl.): 12–9
Jones KP, Charlton IH, Middletown M, et al. Targeting asthma care in general care practice using a morbidity index. BMJ 1992; 304: 1353–6
Weiss KB, Gergen PJ, Crain EF. Inner city asthma: the epidemiology of an emerging US public health concern. Chest 1992; 101(6 Suppl.): 362S–7S
McDermott MJ, Silva J, Rydman R, et al. Practice variations in treating urban minority asthmatics in Chicago. J Med Syst 1996; 20: 244–66
Rakowski W Persistence of public health practices over a one year period. Public Health Rep 1987; 10: 483–93
Author information
Authors and Affiliations
Corresponding author
Additional information
About the Authors: Rose Maljanian, RN, MBA is the Director of the Institute for Outcomes Research and Evaluation at Hartford Hospital, Hartford, Connecticut, USA. She has held a variety of clinical, quality and management appointments in both acute and long term care. Her current area of research focus is high volume, high risk patient populations served by an acute care based Integrated Delivery System. John Goethe, MD is the Medical Consultant for Outcomes Research and the Director of the Burlingame Center for Psychiatric Research and Education at the Institute of Living in Hartford, Connecticut. Dr Goethe is active in both clinical trial and outcomes research. He has published many articles in the mental health literature.
Scott Wolf, DO is the Medical Director of the Asthma Control and Education Program and the Director of Clinical Operations for Ambulatory Medicine at Hartford Hospital, Connecticut. Dr Wolf’s primary area of interest is disease management and public health with a current focus on the inner city asthma population.
Rights and permissions
About this article
Cite this article
Maljanian, R., Goethe, J.W., Wolf, S.A. et al. Baseline Assessment of an Inner City Population Enrolled in an Asthma Disease Management Programme. Dis-Manage-Health-Outcomes 5, 135–143 (1999). https://doi.org/10.2165/00115677-199905030-00002
Published:
Issue Date:
DOI: https://doi.org/10.2165/00115677-199905030-00002