Abstract
Background and objective: Post-herpetic neuralgia (PHN) is a distressing neuropathic pain condition mainly affecting elderly patients. Neuropathic pain symptoms can be of a burning, shooting and stabbing nature, and may continue for prolonged periods and are often poorly controlled by polymedication. The aim of this study was to evaluate the analgesic efficacy and safety of topical analgesic treatment (5% lidocaine [lignocaine] medicated plaster) compared with placebo plaster in patients with PHN.
Methods: This was a double-blind, placebo plaster-controlled, parallel-group, multicentre study employing enriched enrolment with randomized withdrawal methodology. After an initial 8-week open-label, active run-in phase, responders entered a 2-week randomized, double-blind, placebo-controlled phase. The study was conducted at 33 outpatient investigational centres in 12 European countries. Patients with PHN were selected who were aged ≥50 years, had experienced neuropathic pain persisting for ≥3 months after rash healing, and had a mean pain intensity of ≥4 on an 11-point numerical rating scale. A total of 265 patients entered the open-label phase and subsequently a pre-defined number of 71 patients entered the randomized phase. Patients applied up to three 5% lidocaine medicated plasters for up to 12 hours per day. The primary endpoint of the study was time-to-exit due to a ≥2-point reduction in pain relief on two consecutive days of plaster application using a 6-point verbal rating scale.
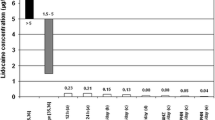
Results: Of the 265 patients entering the run-in phase, 51.7% achieved at least moderate pain relief. In the double-blind phase (full analysis set, n = 71), median times-to-exit were 13.5 (range 2–14) and 9.0 (range 1–14) days for lidocaine and placebo plaster groups, respectively (p = 0.151). For per-protocol patients (n = 34), median time-to-exit was 14.0 (range 3–14) and 6.0 (range 1–14) days for lidocaine and placebo plaster groups, respectively (p = 0.0398). Drug-related adverse events occurred in 13.6% of patients. Treatment with 5% lidocaine medicated plaster was associated with improvements in pain, allodynia, quality of life and sleep measures.
Conclusions: This study adds to a growing body of evidence that the 5% lidocaine medicated plaster can be considered a valuable treatment option for patients with PHN, providing beneficial effects on pain, allodynia, quality of life and sleep, with minimal adverse effects.










Similar content being viewed by others
References
Oster G, Harding G, Dukes E, et al. Pain, medication use, and health-related quality of life in older persons with postherpetic neuralgia: results from a population-based survey. J Pain 2005 Jun; 6(6): 356–63
Schmader KE. Epidemiology and impact on quality of life of postherpetic neuralgia and painful diabetic neuropathy. Clin J Pain 2002 Nov–Dec; 18(6): 350–4
Finnerup NB, Sindrup SH, Jensen TS. Chronic neuropathic pain: mechanisms, drug targets and measurement. Fundam Clin Pharmacol 2007 Apr; 21(2): 129–36
Hempenstall K, Nurmikko TJ, Johnson RW, et al. Analgesic therapy in postherpetic neuralgia: a quantitative systematic review. PLoS Med 2005 Jul; 2(7): e164
Fields HL, Rowbotham M, Baron R. Postherpetic neuralgia: irritable nociceptors and deafferentation. Neurobiol Dis 1998 Oct; 5(4): 209–27
Cruccu G, Anand P, Attal N, et al. EFNS guidelines on neuropathic pain assessment. Eur J Neurol 2004 Mar; 11(3): 153–62
Beydoun A. Postherpetic neuralgia: role of gabapentin and other treatment modalities. Epilepsia 1999; 40Suppl. 6: S51–6; discussion S73-4
Galer BS, Jensen MP, Ma T, et al. The lidocaine patch 5% effectively treats all neuropathic pain qualities: results of a randomized, double-blind, vehicle-controlled, 3-week efficacy study with use of the neuropathic pain scale. Clin J Pain 2002 Sep–Oct; 18(5): 297–301
Gammaitoni AR, Alvarez NA, Galer BS. Safety and tolerability of the lidocaine patch 5%, a targeted peripheral analgesic: a review of the literature. J Clin Pharmacol 2003 Feb;43(2): 111–7
Pappagallo M, Haldey EJ. Pharmacological management of postherpetic neuralgia. CNS Drugs 2003; 17(11): 771–80
Dworkin RH, O’Connor AB, Backonja M, et al. Pharmacologic management of neuropathic pain: evidence-based recommendations. Pain 2007 Dec 5; 132(3): 237–51
Attal N, Cruccu G, Haanpaa M, et al. EFNS guidelines on pharmacological treatment of neuropathic pain. Eur J Neurol 2006 Nov; 13(11): 1153–69
Finnerup NB, Otto M, Jensen TS, et al. An evidence-based algorithm for the treatment of neuropathic pain. Med Gen Med 2007; 9(2): 36
Christo PJ, Hobelmann G, Maine DN. Post-herpetic neuralgia in older adults: evidence-based approaches to clinical management. Drugs Aging 2007; 24(1): 1–19
Priano L, Gasco MR, Mauro A. Transdermal treatment options for neurological disorders: impact on the elderly. Drugs Aging 2006; 23(5): 357–75
Rowbotham MC, Davies PS, Fields HL. Topical lidocaine gel relieves postherpetic neuralgia. Ann Neurol 1995; 37: 246–53
Rowbotham MC, Davies PS, Verkempinck C, et al. Lidocaine patch: double-blind controlled study of a new treatment method for post-herpetic neuralgia. Pain 1996 Apr; 65(1): 39–44
Davies PS, Galer BS. Review of lidocaine patch 5% studies in the treatment of postherpetic neuralgia. Drugs 2004; 64(9): 937–47
McQuay HJ, Derry S, Moore RA, et al. Enriched enrolment with randomised withdrawal (EERW): time for a new look at clinical trial design in chronic pain. Pain 2008 Apr; 135(3): 217–20
Klepstad P, Dale O, Skorpen F, et al. Genetic variability and clinical efficacy of morphine. Acta Anaesthesiol Scand 2005; 49: 902–8
Nagasako EM, Kalauokalani DA. Ethical aspects of placebo groups in pain trials: lessons from psychiatry. Neurology 2005 Dec 29; 65(12 Suppl. 4): S59–65
Temple RJ. Special study designs: early escape, enrichment, studies in non-responders. Communications in statistics theory and methods 1994; 23(2): 499–531
Byas-Smith MG, Max MB, Muir J, et al. Transdermal clonidine compared to placebo in painful diabetic neuropathy using a two-stage ‘enriched enrollment’ design. Pain 1995 Mar; 60(3): 267–74
Galer BS, Rowbotham MC, Perander J, et al. Topical lidocaine patch relieves postherpetic neuralgia more effectively than a vehicle topical patch: results of an enriched enrollment study. Pain 1999 Apr; 80(3): 533–8
Hale ME, Ahdieh H, Ma T, et al. Efficacy and safety of OPANA ER (oxymorphone extended release) for relief of moderate to severe chronic low back pain in opioidexperienced patients: a 12-week, randomized, double-blind, placebo-controlled study. J Pain 2007 Feb; 8(2): 175–84
Hale ME, Dvergsten C, Gimbel J. Efficacy and safety of oxymorphone extended release in chronic low back pain: results of a randomized, double-blind, placebo- and activecontrolled phase III study. J Pain 2005 Jan; 6(1): 21–8
Kongsgaard UE, Poulain P. Transdermal fentanyl for pain control in adults with chronic cancer pain. Eur J Pain 1998 Mar; 2(1): 53–62
Lynch ME, Clark AJ, Sawynok J. Intravenous adenosine alleviates neuropathic pain: a double blind placebo controlled crossover trial using an enriched enrolment design. Pain 2003 May; 103(1-2): 111–7
Schnitzer TJ, Gray WL, Paster RZ, et al. Efficacy of tramadol in treatment of chronic low back pain. J Rheumatol 2000 Mar; 27(3): 772–8
European Medicines Agency: Committee for Medicinal Products for Human Use (CHMP). Guideline on clinical medicinal products intended for the treatment of neuropathic pain [online]. Available from URL: http://www.emea.europa.eu/ pdfs/human/ewp/025203enfin.pdf [Accessed 2009 Apr 9]
Ware Jr JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care 1992 Jun; 30(6): 473–83
Rowbotham M, Harden N, Stacey B, et al. Gabapentin for the treatment of postherpetic neuralgia: a randomized controlled trial. JAMA 1998 Dec 2; 280(21): 1837–42
Freedman LS. Tables of the number of patients required in clinical trials using the logrank test. Stat Med 1982 Apr–Jun; 1(2): 121–9
Meier T, Wasner G, Faust M, et al. Efficacy of lidocaine patch 5% in the treatment of focal peripheral neuropathic pain syndromes: a randomized, double-blind, placebocontrolled study. Pain 2003 Nov; 106(1-2): 151–8
Johnson RW, Wasner G, Saddier P, et al. Herpes zoster and postherpetic neuralgia: optimizing management in the elderly patient. Drugs Aging 2008; 25(12): 991–1006
Hans G, Sabatowski R, Binder A, et al. Efficacy and tolerability of a 5% lidocaine medicated plaster for the topical treatment of post-herpetic neuralgia: results of a long-term study. Curr Med Res Opin 2009; 25(5): 1295–1305
Baron R, Mayoral V, Leijon G, et al. Efficacy and safety of 5% lidocaine (lignocaine) medicated plaster in comparison with pregabalin in patients with postherpetic neuralgia and diabetic polyneuropathy: interim analysis from an openlabel, two-stage adaptive, randomized, controlled trial. Clin Drug Invest 2009; 29(4): 231–41
Katz NP, Gammaitoni AR, Davis MW, et al. Lidocaine patch 5% reduces pain intensity and interference with quality of life in patients with postherpetic neuralgia: an effectiveness trial. Pain Med 2002 Dec; 3(4): 324–32
Argoff CE. Conclusions: chronic pain studies of lidocaine patch 5% using the Neuropathic Pain Scale. Curr Med Res Opin 2004; 20Suppl. 2: S29–31
Herrmann DN, Barbano RL, Hart-Gouleau S, et al. An open-label study of the lidocaine patch 5% in painful idiopathic sensory polyneuropathy. Pain Med 2005 Sep–Oct; 6(5): 379–84
Dworkin RH, Turk DC, Wyrwich KW, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain 2008 Feb; 9(2): 105–21
Backonja M, Wallace MS, Blonsky ER, et al. NGX-4010, a high-concentration capsaicin patch, for the treatment of postherpetic neuralgia: a randomised, double-blind study. Lancet Neurol 2008 Dec; 7(12): 1106–12
Dworkin RH, Corbin AE, Young Jr JP, et al. Pregabalin for the treatment of postherpetic neuralgia: a randomized, placebo-controlled trial. Neurology 2003 Apr 22; 60(8): 1274–83
Plaghki L, Adriaensen H, Morlion B, et al. Systematic overview of the pharmacological management of postherpetic neuralgia: an evaluation of the clinical value of critically selected drug treatments based on efficacy and safety outcomes from randomized controlled studies. Dermatology 2004; 208(3): 206–16
Gloth FM. Pain management in older adults: prevention and treatment. J Am Geriatr Soc 2001; 49: 188–99
Leber PD, Davis CS. Threats to the validity of clinical trials employing enrichment strategies for sample selection. Control Clin Trials 1998 Apr; 19(2): 178–87
Electronic Medicines Compendium. Versatis® 5% medicated plaster: summary of product characteristics [online]. Available from URL: http://emc.medicines.org.uk/emc/ assets/c/html/DisplayDoc.asp?DocumentID = 19291 [Accessed 2009 Apr 9]
Finnerup NB, Otto M, McQuay HJ, et al. Algorithm for neuropathic pain treatment: an evidence based proposal. Pain 2005 Dec 5; 118(3): 289–305
Hanna M, O’Brien C, Wilson MC. Prolonged-release oxycodone enhances the effects of existing gabapentin therapy in painful diabetic neuropathy patients. Eur J Pain 2008 Aug; 12(6): 804–13
Acknowledgements
This study was funded by Grünenthal GmbH. The authors would like to thank the clinical investigators who took part in this study. Medical writing assistance was provided by Wolters Kluwer Health Medical Communications; this assistance was funded by Grünenthal GmbH.
A. Binder has received honoraria from Allergan, Schwarz, Pfizer and Grünenthal. J. Bruxelle is a consultant for Pfizer, Janssen-Cilag, Eli Lilly, Mundipharma, Grünenthal and Sanofi-Pasteur MSD. P. Rogers has received honoraria and research funding from Grünenthal. G. Hans has received research funding from Grünenthal and Pierre-Fabre. I. Bösl is an employee of Grünenthal. R. Baron has received honoraria from Allergan, Schwarz, Pfizer, Grünenthal, Sanofi-Pasteur and Genzyme and received research funding from Pfizer, Grünenthal and Genzyme.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Binder, A., Bruxelle, J., Rogers, P. et al. Topical 5% Lidocaine (Lignocaine) Medicated Plaster Treatment for Post-Herpetic Neuralgia. Clin. Drug Investig. 29, 393–408 (2009). https://doi.org/10.2165/00044011-200929060-00003
Published:
Issue Date:
DOI: https://doi.org/10.2165/00044011-200929060-00003