Abstract
Objective
A high proportion of patients with gastro-oesophageal reflux disease experience recurrence of symptoms within a year of initial treatment. The key to preventing relapse is an effective maintenance therapy that maintains intragastric pH >4. This study was conducted to compare the effects on intragastric pH of maintenance doses of four proton pump inhibitors: esomeprazole 20mg, lansoprazole 15mg, rabeprazole 10mg and pantoprazole 20mg.
Study participants and methods
Three standardised, randomised, two-way crossover studies were performed in a total of 108 Helicobacter pylori-negative healthy subjects. Intragastric pH was monitored on day 5 of once-daily oral dosing. The percentage of time of a 24-hour period with intragastric pH >4 and 24-hour median pH were measured on day 5.
Results
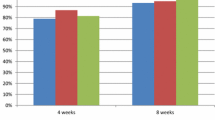
The mean percentage of time with intragastric pH >4 on day 5 was significantly longer following esomeprazole 20mg compared with either lansoprazole 15mg (esomeprazole 50.4% vs lansoprazole 43.0%, p = 0.026), rabeprazole 10mg (esomeprazole 59.8% vs rabeprazole 51.7%, p = 0.011) or pantoprazole 20mg (esomeprazole 59.6% vs pantoprazole 39.5%, p < 0.0001).
Conclusions
Maintenance dose esomeprazole 20mg provided greater acid control and maintained intragastric pH >4 for a longer period of time than maintenance dose lansoprazole 15mg, rabeprazole 10mg and pantoprazole 20mg in healthy subjects.



Similar content being viewed by others
References
Hunt RH. Importance of pH control in the management of GERD. Arch Intern Med 1999; 159(7): 649–57
Olbe L, Lundell L. Medical treatment of reflux esophagitis. Hepatogastroenterology 1992; 39(4): 322–4
Lagergren J, Bergstrom R, Lindgren A, et al. Symptomatic gastroesophageal reflux as a risk factor for esophageal adeno-carcinoma. N Engl J Med 1999; 340(11): 825–31
Bell NJV, Burget D, Howden CW, et al. Appropriate acid suppression for management of gastro-oesophageal reflux disease. Digestion 1992; 51 Suppl. 1: 59–67
Havelund TT, Lind T, Wiklund I, et al. Quality of life in patients with heartburn but without esophagitis: effects of treatment with omeprazole. Am J Gastroenterol 1999; 94(7): 1782–9
Revicki DA, Wood M, Maton PN, et al. The impact of gastro-esophageal reflux disease on health-related quality of life. Am J Med 1998; 104(3): 252–8
Chiba N, De Gara CJ, Wilkinson JM, et al. Speed of healing and symptom relief in grade II to IV gastroesophageal reflux disease: a meta-analysis. Gastroenterology 1997; 112(6): 1798–810
Lind T, Rydberg L, Kyleback A, et al. Esomeprazole provides improved acid control vs. omeprazole in patients with symptoms of gastro-oesophageal reflux disease. Aliment Pharmacol Ther 2000; 14(7): 861–7
Röhss K, Wilder-Smith C, Claar-Nilsson C, et al. Esomeprazole 40mg provides more effective acid control than standard doses of all other proton pump inhibitors [abstract]. Gastroenterology 2001; 120: A419
Miner PB, Katz PO, Chen Y, et al. Gastric acid control with esomeprazole, omeprazole, pantoprazole and rabeprazole: a five-way crossover study. Am J Gastroenterol 2003; 98: 2616–20
National Institute for Clinical Excellence 2000. Guidance on the use of proton pump inhibitors (PPIs) in the treatment of dyspepsia [online]. Available from URL: http://www.nice.org.uk [Accessed 2003 Sep 12]
DeVault KR, Castell DO, and The Practice Parameters Committee of the American College of Gastroenterology. Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease. Am J Gastroenterol} 1999}; 94}: 1434–42
Dent J, Brun J, Fendrick AM, et al. An evidence-based appraisal of reflux disease management: the Genval workshop report. Gut 1999; 44 Suppl. 2: Sl–16
Wilder-Smith C, Röhss K, Claar-Nilsson C. Esomeprazole 20mg provides more effective acid control than lansoprazole 15mg [abstract]. Gut 2000; 47 Suppl. 3: A62
Röhss K, Claar-Nilsson C, Jansson L. Esomeprazole 20mg provides more effective acid control than rabeprazole 10mg following repeated drug administration. Scand J Gastroenterol 2002; 37(6 Suppl. 235): 2–38
Nilsson-Pieschl C, Lundin C, Hjalmar K, et al. Esomeprazole 20mg provides faster and more effective acid control than pantoprazole 20mg in healthy volunteers. Scand J Gastroenterol 2003; 38Suppl 238: A–P3
Howden CW, Burget DW, Hunt RH. Appropriate acid suppression for optimal healing of duodenal ulcer and gastro-oesophageal reflux disease. Scand J Gastroenterol 1994; 29 Suppl. 201: 79–82
Thomson ABR, Claar-Nilsson C, Hasselgren G, et al. Esomeprazole 40mg provides more effective acid control than lansoprazole 30mg during single and repeated administration [abstract]. Gut 2000; 47 Suppl. 3: 63
Lauritsen K, Deviere J, Bigard M-A. Esomeprazole 20mg is more effective than lansoprazole 15mg in the maintenance treatment of patients with healed reflux oesophagitis. Aliment Pharmacol Ther 2003; 17(3): 333–41
Johnson DA, Vakil NB, Hwang C, et al. Impact of esomeprazole on symptom control in patients with healed erosive esophagitis [abstract 2247]. Gastroenterology 2001; 120(5 Suppl. 1): A441
Blum RA, Shi H, Karol MD, et al. The comparative effects of lansoprazole, omeprazole and ranitidine in suppressing gastric acid secretion. Clin Ther 1997; 19(5): 1013–23
Tutuian R, Katz PO, Bochenek W, et al. Dose-dependent control of intragastric pH by pantoprazole, 10, 20 or 40mg, in healthy volunteers. Aliment Pharmacol Ther 2002; 16: 829–36
Baisley KJ, Warrington S, Tejura B, et al. Rabeprazole 20mg compared with esomeprazole 40mg in the control of intragastric pH in healthy volunteers [abstract 148]. Am J Gastroenterol 2001; 96(9 Suppl. ): S48
Warrington S, Baisley K, Boyce M, et al. Effects of rabeprazole, 20mg, or esomeprazole, 20mg, on 24-h intragastric pH and serum gastrin in healthy subjects. Aliment Pharmacol Ther 2002; 16: 1301–7
Hirschowitz BI. A critical analysis with appropriate controls of gastric acid and pepsin secretion in clinical esophagitis. Gastroenterology 1991; 101: 1149–58
Acknowledgements
This study was supported by a grant from AstraZeneca R&D Mölndal, Mölndal, Sweden.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Röhss, K., Wilder-Smith, C., Nauclér, E. et al. Esomeprazole 20mg Provides More Effective Intragastric Acid Control than Maintenance-Dose Rabeprazole, Lansoprazole or Pantoprazole in Healthy Volunteers. Clin. Drug Investig. 24, 1–7 (2004). https://doi.org/10.2165/00044011-200424010-00001
Published:
Issue Date:
DOI: https://doi.org/10.2165/00044011-200424010-00001