Abstract
Background and objective: In the treatment of bone infections, a major determinant of the clinical response is the active drug concentration at the infected site. Because of the high prevalence of meticillin (methicillin)-resistant staphylococci and enterococci, glycopeptides are widely used for the treatment of bone and joint infections, but data on their penetration into human bone are lacking. The aim of our study was to measure vancomycin and teicoplanin concentrations in infected human bone under steady-state conditions and verify their relationship with inflammatory markers, patient demographic characteristics and pharmacodynamic microbiological markers.
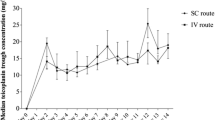
Methods and patients: Twenty-seven adult orthopaedic patients undergoing surgical debridement for septic pseudoarthrosis of the tibia and receiving either intravenous vancomycin (Vancocina® 1 g twice daily) or teicoplanin (Targosid® 10 mg/kg/day) were studied from January 2004 to January 2008. Plasma and bone specimens were simultaneously collected during surgery for pharmacokinetic and microbiological assays at a variable interval after antimicrobial administration. Bone samples were dissected into cortical and cancellous bone, cleaned of soft tissues, crushed and eluted into phosphate buffer. Necrotic samples and sequestra were not analysed.
Plasma and bone antimicrobial concentrations were measured by a validated method of high-performance liquid chromatography with UV detection, and bone/plasma concentration ratios were calculated. Cortical and cancellous bone area under the concentration-time curve (AUC) over 24 hours (AUC24) values were measured by the linear-log trapezoidal rule, using WinNonlin® software, and were compared with the minimum inhibitory concentrations (MICs) of the infecting agents.
Results: For vancomycin, the mean ± SD concentrations were 2.66 ± 1.2 mg/L in cortical bone and 11.53 ± 7.8 mg/L in cancellous bone (corresponding to 20.67% and 89.39% of intraoperative plasma concentrations), and the mean ± SD tissue AUC24 values were 55.15 ± 25.26 h · mg/L for cortical bone and 299.16 ± 299.54 h · mg/L for cancellous bone. For teicoplanin, the mean ± SD concentrations were 2.01 ± 1.7 and 7.51 ± 7.0 mg/L in cortical and cancellous bone, respectively (12.35% and 48.6% of intraoperative plasma concentrations), and the mean ± SD teicoplanin tissue AUC24 values were 34.08 ± 23.6 h · mg/L and 155.17 ± 132.8 h · mg/L for cortical bone and cancellous bone, respectively. The mean vancomycin AUC24/MIC ratios were 215.02 for plasma, 47.14 for cortical bone and 268.95 for cancellous bone. The mean teicoplanin AUC24/MIC ratios were 336.48, 36.27 and 197.21 for plasma, cortical bone and cancellous bone, respectively.
Conclusions: Bone penetration of both glycopeptides ranged from poor (<15%) to satisfactory (15–30%) in the cortical compartment, while it was far higher into the highly vascularized cancellous tissue. Vancomycin bone penetration was slightly higher than with teicoplanin, but the difference was not statistically significant. Higher bone concentrations were observed with higher inflammatory markers, possibly as a result of increased vascularization and vascular permeability under inflammatory conditions. Bone concentrations over the MIC and AUC/MIC ratios suggested that both glycopeptides achieve a satisfactory pharmacokinetic exposure in the cancellous bone, as far as Gram-positive pathogens are concerned. On the other hand, cortical bone exposure was suboptimal in most patients. Furthermore, as antimicrobial penetration may be affected by impaired blood supply, the role of radical surgical removal of purulent and necrotic tissues appears to be essential in order to shorten treatment duration and to reduce the risk of treatment failure.











Similar content being viewed by others
Notes
The use of trade names is for product identification purposes only and does not imply endorsement.
References:
Norden CW. Osteomyelitis. In: Mandell GL, Douglas RG, Bennett JE, editors. Principles and practice of infectious diseases, 3rd ed. New York: Churchill Livingstone, 1990: 922–30
Cierny G, Mader JT, Penninck JJ. A clinical staging system for adult osteomyelitis. Contemp Orthop 1985; 10: 17–37
Lieberman JR, Callaway GH, Salvati EA, et al. Treatment of the infected total hip arthroplasty with a two stage reimplantation protocol. Clin Orthopaed Related Res 1994; 301: 205–12
Redington J, Ebert SC, Craig WA. Role of antimicrobial pharmacokinetics and pharmacodynamics in surgical prophylaxis. Rev Infect Dis 1991; 13 Suppl. 10: 790–9
Tsukayama DT, Guay DRR, Peterson PK. Antibiotic therapy of chronic osteomyelitis. In: Gustilo RB, Gruninger RP, Tsukayama DT, editors. Orthopaedic infection: diagnosis and treatment. Philadelphia (PA): Saunders, 1989: 166–74
Darley ESR, MacGowan AP. Antibiotic treatment of Gram-positive bone and joint infections. J Antimicrob Chemother 2004; 53: 928–35
Djabarouti S, Boselli E, Allaouchiche B, et al. Determination of levofloxacin in plasma, bronchoalveolar lavage and bone tissues by high-performance liquid chromatography with ultraviolet detection using a fully automated extraction method. J Chromatogr B 2004; 799: 165–72
Roncoroni AJ, Manuel C, Nedjar C, et al. Cefamandole bone diffusion in patients undergoing total hip replacement. Chemotherapy 1981; 27(3): 166–72
Cristofolini L, Viceconti M, Cappello A, et al. Mechanical validation of whole bone composite femur models. J Biomechanics 1996; 29: 525–35
Martin C, Alaya M, Mallet MN, et al. Penetration of vancomycin into mediastinal and cardiac tissues in humans. Antimicrob Agents Chemother 1994; 38(2): 396–9
Vuorisalo S, Pokela R, Satta J, et al. Internal mammary artery harvesting and antibiotic concentrations in sternal bone during coronary artery bypass. Int J Angiol 2000; 9(2): 78–81
Kitzes-Cohen R, Farin D, Piva G, et al. Pharmacokinetics of vancomycin administered as prophylaxis before cardiac surgery. Ther Drug Monit 2000; 22(6): 661–7
Borner K, Hahn F, Koeppe P. Concentrations of vancomycin in human bone. J Chemother 1989; 1 (4 Suppl.): 588–9
Graziani AL, Lawson LA, Gibson GA, et al. Vancomycin in infected and non-infected human bone. Antimicrob Agents Chemother 1988; 32: 1320–2
Massias L, Dubois C, De Lentdecker P, et al. Penetration of vancomycin in uninfected sternal bone. Antimicrob Agents Chemother 1992; 36: 2539–41
Desplaces N, Mamoudy P, Ducroquet F, et al. Vancomycine en perfusion continue et infections ostéo-articulaires à staphylocoques multirésistants. Med Mal Infect 1997; 27: 969–74
Garcia-Zabarte A, Penalver D, Aguilera A, et al. Serum and bone levels of teicoplanin in total hip replacement [abstract no. 0445]. 34th Interscience Conference on Antimicrobial Agents and Chemotherapy; 1994 Oct 4–7; Orlando (FL)
Rosina R, Avai A, Suter F, et al. Pharmacokinetics of teicoplanin in human bone [abstract no. 249]. 16th International Congress of Chemotherapy; 1989 Jun 18–20; Jerusalem
Sirot J, Dumont C, Delisle JJ, et al. Pénétration de la teicoplanine dans l’os [abstract no. 221]. Réunion Interdisciplinaire de Chimiothérapie Anti-Infectieuse; 1986; Paris
Wilson AP, Taylor B, Treasure T, et al. Antibiotic prophylaxis in cardiac surgery: serum and tissue levels of teicoplanin, flucloxacillin and tobramycin. J Antimicrob Chemother 1988; 21(2): 201–12
Martin C, Bourget P, Alaya M, et al. Teicoplanin in cardiac surgery: intraoperative pharmacokinetics and concentrations in cardiac and mediastinal tissues. Antimicrob Agents Chemother 1997; 41(5): 1150–5
De Lalla F, Novelli A, Pellizzer G, et al. Regional and systemic prophylaxis with teicoplanin in monolateral and bilateral total knee replacement procedures: study of pharmacokinetics and tissue penetration. Antimicrob Agents Chemother 1993; 37(12): 2693–8
Lazzarini L, Novelli A, Marzano N, et al. Regional and systemic prophylaxis with teicoplanin in total knee arthroplasty. J Arthroplasty 2003; 18: 342–6
Nehrer S, Thalhammer F, Schwameis E, et al. Teicoplanin in the prevention of infection in total hip replacement. Arch Orthop Trauma Surg 1998; 118: 32–6
Mouton JW, Theuretzbacher U, Craig WA, et al. Tissue concentrations: do we ever learn? J Antimicrob Chemother 2008; 61: 235–7
Boselli E, Allaouchiche B. Diffusion osseuse des antibiotiques. Presse Med 1999; 28: 2265–76
Goldstein FW, Mainardi JL. Sensibilité et résistance des souches: quotients inhibiteurs. In: Mainardi JL, editor. Précis d’antibiothérapie pratique. Paris: Phase 5 Éditions Médicales, 1995: 81–147
Larsson AJ, Walker KJ, Raddaz JK, et al. The concentration-independent effect of monoexponential and biexponential decay in vancomycin concentrations on the killing of Staphylococcus aureus under aerobic and anaerobic conditions. J Antimicrob Chemother 1996; 38: 589–97
Ahmed A, Jafri H, Lutsar I, et al. Pharmacodynamics of vancomycin for the treatment of experimental penicillin- and cephalosporin-resistant pneumococcal meningitis. Antimicrob Agents Chemother 1999; 43: 876–81
Peetermans WE, Hoogeterp JJ, Hazekamp-van Dokkum AM, et al. Antistaphylococcal activities of teicoplanin and vancomycin in vitro and in experimental infection. Antimicrob Agents Chemother 1990; 34: 1869–74
Ambrose PG, Bhavnani SM, Rubino CM, et al. Pharmacokinetics-pharmacodynamics of antimicrobial therapy: it’s not just for mice anymore. Clin Infect Dis 2007; 44: 79–86
Hyatt JM, McKinnon PS, Zimmer GS, et al. The importance of pharmacokinetic/ pharmacodynamic surrogate markers to outcome: focus on antibacterial agents. Clin Pharmacokinet 1995; 28(2): 143–60
Moise-Broder PA, Forrest A, Birmingham MC, et al. Pharmacodynamics of vancomycin and other antimicrobials in patients with Staphylococcus aureus lower respiratory tract infections. Clin Pharmacokinet 2004; 43: 925–42
MacGowan AP, Bowker KE. Pharmacodynamics of antimicrobial agents and rationale for their dosing. J Chemother 1997; 9 Suppl. 1: S64–73
MacGowan A, White L, Reeves D, et al. Retrospective review of serum teicoplanin concentrations in clinical trials and their relationship to clinical outcome. J Infect Chemother 1996; 2: 197–208
Vuagnat A, Stern R, Lotthe A, et al. High dose vancomycin for osteomyelitis: continuous vs intermittent infusion. J Clin Pharm Therap 2004; 29: 351–7
Acknowledgements
No sources of funding were used to assist in the preparation of this study. The authors have no conflicts of interest that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Garazzino, S., Aprato, A., Baietto, L. et al. Glycopeptide Bone Penetration in Patients with Septic Pseudoarthrosis of the Tibia. Clin Pharmacokinet 47, 793–805 (2008). https://doi.org/10.2165/0003088-200847120-00004
Published:
Issue Date:
DOI: https://doi.org/10.2165/0003088-200847120-00004