Summary
Abstract
Metopimazine (Vogalene®) is a dopamine D2receptor antagonist that has been used in France for many years for the prevention and treatment of nausea and vomiting. Guidelines suggest a role for dopamine receptor antagonists in the prevention of delayed chemotherapy-induced nausea and vomiting (CINV) following moderately emetogenic chemotherapy and as add-on therapy in refractory cases; recent data on sublingual metopimazine suggest it may have a role as an alternative to ondansetron in the prevention of delayed CINV in patients receiving moderately to highly emetogenic non-cisplatin-based chemotherapy. Trials comparing metopimazine with other drugs used in the prevention of delayed CINV would be of interest. Data also support the use of metopimazine as add-on therapy in the treatment of acute emesis in patients receiving moderately emetogenic chemotherapy who are refractory to initial therapy or unable to take corticosteroids, roles which are also suggested for dopamine receptor antagonists in guidelines, as is their potential use in rescue therapy for patients with breakthrough symptoms.
Pharmacologic Properties
Metopimazine is a phenothiazine derivative with anti-dopaminergic activity. It has a high affinity for dopamine D2receptors (and also α1-adrenoceptors and histamine H1receptors) but no affinity for serotonin 5-HT3receptors. It exerts its antiemetic effects via the chemoreceptor trigger zone. Although metopimazine itself can cross the blood-brain barrier, its acid metabolite, which is the predominant circulating form of the drug, crosses to a very limited extent, and extrapyramidal effects and effects on prolactin are uncommon. Metopimazine can occasionally be associated with orthostatic hypotension, which probably relates to its affinity for the α1-adrenoceptor.
Peak serum concentrations are reached within 60 minutes after fasting oral administration (≈20 minutes for sublingual tablets). The bioavailability of oral metopimazine is 19–34%. Oral absorption is reduced by food. Metopimazine is rapidly metabolized to its active acid metabolite, which constitutes approximately 78–89% of the circulating drug. Approximately 30% of a dose is recovered in the urine (mostly as the acid form), and the elimination half-life of the parent drug is approximately 4.5 hours.
Therapeutic Efficacy
Metopimazine has been evaluated for the prevention of acute or delayed CINV in adults in several randomized, controlled trials, some of which were performed a number of years ago and used treatment regimens that differ from current recommendations. In the earliest studies (performed in the 1970s and using different endpoints to later trials), the overall (and possibly acute) efficacy of oral metopimazine in the reduction of severity of CINV was superior to that of placebo in patients receiving low to highly emetogenic non-cisplatin-based chemotherapy, and similar to that of prochlorperazine in patients receiving fluorouracil.
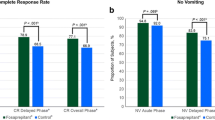
Results from trials performed since 1997 (which each evaluated similar endpoints) indicated that the addition of intravenous metopimazine to ondansetron plus methylprednisolone significantly increased antiemetic efficacy in the acute phase compared to ondansetron plus methylprednisolone in patients receiving cisplatin who were refractory to the dual therapy (87% vs 75% of patients experienced no acute emesis); also that intravenous metopimazine plus ondansetron was significantly more effective than ondansetron alone at preventing acute emesis in patients receiving highly emetogenic (cisplatin-based) chemotherapy. Oral metopimazine combined with prednisolone was significantly less effective than intravenous granisetron in the acute setting (comparison of all response categories), but more effective than granisetron (both in terms of overall response categories and complete response rate) in the prevention of delayed CINV in patients receiving moderately emetogenic chemotherapy.
Based on two recent studies specifically designed to evaluate efficacy in the prevention of delayed emesis, sublingual metopimazine was as effective as ondansetron when administered as monotherapy, and at least as effective when both drugs were coadministered with methylprednisolone, in patients receiving moderately to highly emetogenic (generally non-cisplatin-based) chemotherapy. The percentages of patients who experienced no delayed emesis (and ≤1 episode of nausea) when treated with metopimazine or metopimazine plus methylprednisolone were 53% and 74% compared with 50% and 58% for recipients of ondansetron or ondansetron plus methylprednisolone. Additional supportive data for the effectiveness of metopimazine in combination with other antiemetic agents (particularly ondansetron) for the prevention of delayed nausea and vomiting are available from studies that were not specifically designed to examine delayed emesis.
Tolerability
Metopimazine is generally well tolerated. In CINV trials, the overall incidence of adverse events with metopimazine monotherapy was similar to that seen with placebo and with ondansetron; however, metopimazine was associated with significantly fewer gastrointestinal adverse events than ondansetron.
The most common adverse events reported with sublingual metopimazine monotherapy in a large clinical trial in CINV included constipation, diarrhea, abdominal pain, headache, and asthenia (and also alopecia and mucositis, which were most probably related to the chemotherapy patients had received).
Based on a summary of periodic safety update reports, the adverse events most frequently reported with metopimazine (all formulations; cancer and non-cancer indications) include somnolence, heartburn, dry mouth, diarrhea, constipation, vertigo, tachycardia, dysuria, headache, and pruritus. Metopimazine can be associated with orthostatic hypotension at high dosages. Extrapyramidal symptoms, including dyskinesias, are very uncommon.






Similar content being viewed by others
Notes
The use of trade names is for product identification purposes only and does not imply endorsement.
References
National Comprehensive Cancer Network. Clinical practice guidelines in oncology: antiemesis. Version 1.2006 [online]. Available from URL: http:/www.nccn.org/professionals/physician_gls/PDF/antiemetics.pdf [Accessed 2006 Mar 31]
Hesketh PJ. Understanding the pathobiology of chemotherapy-induced nausea and vomiting: providing a basis for therapeutic progress. Oncology (Huntingt) 2004Sep; 18(10 Suppl. 6): 9–14
Herrstedt J, Aapro MS, Roila F, et al. ESMO minimum clinical recommendations for prophylaxis of chemotherapy-induced nausea and vomiting (NV). Ann Oncol 2005May; 16Suppl. 1: i77–9
Jordan K, Kasper C, Schmoll H-J. Chemotherapy-induced nausea and vomiting: current and new standards in the antiemetic prophylaxis and treatment. Eur J Cancer 2005Jan; 41(2): 199–205
Kris MG, Hesketh PJ, Herrstedt J, et al. Consensus proposals for the prevention of acute and delayed vomiting and nausea following high-emetic-risk chemotherapy. Support Care Cancer 2005; 13: 85–96
Roila F, Warr D, Clark-Snow RA, et al. Delayed emesis: moderately emetogenic chemotherapy. Support Care Cancer 2005; 13: 104–8
Herrstedt J, Koeller JM, Roila F, et al. Acute emesis: moderately emetogenic chemotherapy. Support Care Cancer 2005; 13: 97–103
Vogalene Lyoc: summary of product characteristics. Boulogne Billancourt: Laboratoires Schwarz Pharma
Herrstedt J, Hyttel J, Pedersen J. Interaction of the antiemetic metopimazine and anticancer agents with brain dopamine D2, 5-hydroxytryptamine3, histamine H1, muscarine cholinergic and (α1-adrenergic receptors. Cancer Chemother Pharmacol 1993Oct; 33: 53–6
Berger A, Clark-Snow RA. 53.1 Adverse effects of treatment: nausea and vomiting. In: DeVita JrVT, Hellman S, Rosenberg SA, editors. Cancer: principles and practice of oncology. 5thed. Philadelphia (PA): Lippincott-Raven, 1997: 2705–12
Vogalib® 7.5mg, oral lyophilisat: summary of product brochure. Boulogne Billancourt: Laboratoires Schwarz Pharma
Data on file. Boulogne Billancourt: Laboratoires Schwarz Pharma, 2005
Herrstedt J, Jorgensen M, Angelo HR. The effect of food on serum concentrations of metopimazine. Br J Clin Pharmacol 1990Aug; 30: 237–43
Herrstedt J, Jorgensen M, Angelo HR, et al. Bioavailability of the antiemetic metopimazine given as a microenema. Br J Clin Pharmacol 1996Jun; 41: 613–5
Moertel CG, Reitemeier RJ. Controlled studies of metopimazine for the treatment of nausea and vomiting. J Clin Pharmacol 1973Jul; 13: 283–7
Israel L, Rodary C. Treatment of nausea and vomiting related to anti-cancerous multiple combination chemotherapy: results of two controlled studies. J Int Med Res 1978; 6: 235–40
Bethune-Volters A, Chidiac J, Bensaoula O. A randomized, double-blind trial assessing the efficacy and safety of sublingual metopimazine and ondansetron in the prophylaxis of chemotherapy-induced delayed emesis. Anticancer Drugs 2006; 17: 217–24
Sigsgaard T, Herrstedt J, Handberg J, et al. Ondansetron plus metopimazine compared with ondansetron plus metopimazine plus prednisolone as antiemetic prophylaxis in patients receiving multiple cycles of moderately emetogenic chemotherapy. J Clin Oncol 2001Apr 1; 19(7): 2091–7
Herrstedt J, Sigsgaard T, Boesgaard M, et al. Ondansetron plus metopimazine compared with ondansetron alone in patients receiving moderately emetogenic chemotherapy. N Engl J Med 1993Apr 15; 328(15): 1076–80
Sigsgaard T, Herrstedt J, Andersen LJ, et al. Granisetron compared with prednisolone plus metopimazine as anti-emetic prophylaxis during multiple cycles of moderately emetogenic chemotherapy. Br J Cancer 1999May; 80(3–4): 412–8
Herrstedt J, Sigsgaard T, Handberg J, et al. Randomized, double-blind comparison of ondansetron versus ondansetron plus metopimazine as antiemetic prophylaxis during platinum-based chemotherapy in patients with cancer. J Clin Oncol 1997Apr; 15(4): 1690–6
Lebeau B, Depierre A, Giovannini M, et al. The efficacy of a combination of ondansetron, methylprednisolone and metopimazine in patients previously uncontrolled with a dual antiemetic treatment in cisplatin-based chemotherapy. Ann Oncol 1997Sep; 8: 887–92
Bloch J, Rixe O, Meric JB, et al. Comparison of the efficacy and safety of combinations of metopimazine or ondansetron with methylprednisolone in the prevention of delayed emesis in patients receiving chemotherapy. Curr Med Res Opin 2005; 21(11): 1763–71
Grunberg SM, Osoba D, Hesketh PJ, et al. Evaluation of new antiemetic agents and definition of antineoplastic agent emetogenicity: an update. Support Care Cancer 2005; 13: 80–4
Hesketh PJ, Kris MG, Grunberg SM, et al. Proposal for classifying the acute emetogenicity of cancer chemotherapy. J Clin Oncol 1997Jan; 15(1): 103–9
Herrstedt J, Sigsgaard T, Dombernowsky P. Antiemetic effects of ondansetron and metopimazine [reply]. N Engl J Med 1993Oct 28; 329(18): 1356–7
Herrstedt J, Sigsgaard T, Angelo HR, et al. Dose-finding study of oral metopimazine. Support Care Cancer 1997Jan; 5: 38–43
Dictionnaire Vidal. 80th ed. Issy-Les-Moulineaux, France, 2005
Hesketh PJ, VanBelle S, Aapro M, et al. Differential involvement of neurotransmitters through the time course of cisplatin-induced emesis as revealed by therapy with specific receptor antagonists. Eur J Cancer 2003; 39: 1074–80
Dando TM, Perry CM. Aprepitant: a review of its use in the prevention of chemotherapy-induced nausea and vomiting. Drugs 2004; 64(7): 777–94
Italian Group for Antiemetic Research. Double-blind, dose-finding study of four intravenous doses of dexamethasone in the prevention of cisplatin-induced acute emesis. J Clin Oncol 1998Sep; 16(9): 2937–42
Warr DG, Hesketh PJ, Gralla RJ, et al. Efficacy and tolerability of aprepitant for the prevention of chemotherapy-induced nausea and vomiting in patients with breats cancer after moderately emetogenic chemotherapy. J Clin Oncol 2005Apr 20; 23(12): 2822–30
Olver I, Paska W, Depierre A, et al. A multicentre, double-blind study comparing placebo, ondansetron and ondansetron plus dexamethasone for the control of cisplatin-induced delayed emesis. Ann Oncol 1996; 7: 945–52
Gralla R, Lichinitser M, Van derVegt S, et al. Palonosetron improves prevention of chemotherapy-induced nausea and vomiting following moderately emetogenic chemotherapy: results of a double-blind randomized phase III trial comparing single doses of palonestron with ondansetron. Ann Oncol 2003; 14: 1570–7
Eisenberg P, Figueroa-Vadillo J, Zamora R, et al. Improved prevention of moderately emetogenic chemotherapy-induced nausea and vomiting with palonosetron, a pharmacologically novel 5-HT3receptor antagonist. Cancer 2003Dec 1; 98(11): 2473–82
Herrstedt J. Chemotherapy-induced nausea and vomiting with special emphasis on metopimazine. Dan Med Bull 1998Sep; 45: 412–22
Author information
Authors and Affiliations
Corresponding author
Additional information
Various sections of the manuscript reviewed by: E. Ballatori, Department of Internal Medicine and Public Health, University of L’Aquila, L’Aquila, Italy; M. Di Palma, Department of Medical Oncology, Institut Gustave Roussy, Villejuif, France; L. Dupuis, Department of Pharmacy, The Hospital for Sick Children, Toronto, Ontario, Canada; J. Herrstedt, Department of Oncology, Copenhagen University Hospital Herlev, Herlev, Denmark; K. Jordan, Klinik füur Innere Medizin IV, Universitätsklinik Halle/Wittenberg, Halle, Germany; J.-E. Kurtz, Département d’Hématologie et d’Oncologie, Hôpitaux Universitaires de Strasbourg, Strasbourg, France; H. Link, Medizinische Klinik I, Westpfalz-Klinikum, Kaiserslautern, Germany; I. Olver, Department of Cancer Care, University of Adelaide, Adelaide, South Australia, Australia; P.J. Souquet, Hospices Civils de Lyon, Centre Hospitalier Lyon Sud, Pierre-Benite Cedex, France; G. Tonini, Oncology Department, Campus Bio-Medico University, Rome, Italy; S. Van Belle, Department of Medical Oncology, University Hospital Ghent, Ghent, Belgium.
Data Selection
Sources: Medical literature published in any language since 1980 on ‘metopimazine’, identified using MEDLINE and EMBASE, supplemented by AdisBase (a proprietary database of Adis International). Additional references were identified from the reference lists of published articles. Bibliographical information, including contributory unpublished data, was also requested from the company developing the drug.
Search strategy: MEDLINE search terms were ‘metopimazine’ and (‘chemotherapy-induced’ or ‘nausea’ or ‘vomiting’ or ‘antiemetics’). EMBASE search terms were ‘metopimazine’ and (‘chemotherapy-induced’ or ‘nausea’ or ‘vomiting’ or ‘antiemetic’). AdisBase search terms were ‘metopimazine’ and (‘chemotherapy-induced’ or ‘nausea’ or ‘vomiting’ or ‘antiemetics’ or ‘antiemesis’). Searches were last updated 27 March 2006.
Selection: Studies in patients treated with emetogenic cancer chemotherapy who received metopimazine. Inclusion of studies was based mainly on the methods section of the trials. When available, large, well controlled trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
Index terms: Metopimazine, chemotherapy-induced nausea and vomiting, dopamine receptor antagonist, pharmacodynamics, pharmacokinetics, phenothiazines, therapeutic use.
Rights and permissions
About this article
Cite this article
Croom, K.F., Keating, G.M. Metopimazine. Am J Cancer 5, 123–136 (2006). https://doi.org/10.2165/00024669-200605020-00006
Published:
Issue Date:
DOI: https://doi.org/10.2165/00024669-200605020-00006