Summary
Abstract
Letrozole is a highly selective nonsteroidal aromatase inhibitor. In postmenopausal women with advanced breast cancer, letrozole inhibits whole body aromatization by >98% and reduces plasma levels of estrone, estradiol and estrone sulfate by 74 to >95%. It also significantly inhibits aromatase activity and significantly reduces endogenous estrogen levels within breast tumors.
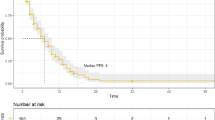
Letrozole is superior to tamoxifen in the first-line treatment of postmenopausal women with advanced breast cancer. In a large, well designed trial, letrozole recipients were significantly less likely than tamoxifen recipients to experience disease progression or treatment failure and significantly more likely to experience an objective response or clinical benefit. The survival rate was significantly higher in letrozole than in tamoxifen recipients at 1 and 2 years.
In the second-line treatment of postmenopausal women with advanced breast cancer, letrozole was at least as effective as megestrol and was superior to aminoglutethimide, according to the results of three large, well designed trials. Letrozole 2.5 mg/day recipients were significantly more likely than letrozole 0.5 mg/day recipients or megestrol recipients to achieve an objective response in one trial, while no difference between the three treatment groups was seen in a second study. However, in this study, a significantly lower risk of disease progression and treatment failure was seen in letrozole 0.5 mg/day than in megestrol recipients. In the other trial, letrozole 2.5 mg/day, compared with megestrol, recipients were significantly less likely to experience treatment failure and had significantly longer durations of objective response and clinical benefit. Compared with aminoglutethimide recipients, letrozole recipients were significantly less likely to experience disease progression or treatment failure, and had significantly prolonged survival.
Second-line therapy with letrozole was associated with a significantly higher overall response rate than anastrozole in postmenopausal women with advanced breast cancer.
Letrozole was generally well tolerated in postmenopausal women with advanced breast cancer with adverse events tending to be of mild-to-moderate severity. Letrozole had similar tolerability to tamoxifen in the first-line treatment of advanced breast cancer. In terms of second-line treatment, letrozole appeared to be better tolerated than megestrol, aminoglutethimide or anastrozole.
Conclusion: Letrozole is an effective option in the first- and second-line treatment of postmenopausal women with advanced who have hormone receptor-positive disease or disease of unknown receptor status. Letrozole is superior to tamoxifen in the first-line treatment of advanced breast cancer and at least as effective as megestrol, with better tolerability, in the second-line treatment of advanced breast cancer.
Pharmacodynamic Properties
Administration of letrozole 0.5 or 2.5 mg/day inhibited aromatization bys >98% in postmenopausal women with advanced breast cancer. Furthermore, letrozole 2.5 mg/day was associated with more complete inhibition of whole body aromatization than anastrozole 1 mg/day in a crossover study involving 12 postmenopausal women with advanced breast cancer. Aromatase levels were detectable in none of the 12 patients during letrozole administration (>99.1% inhibition) and in 11 of 12 patients during anastrozole administration (mean inhibition of 97.3%). A significant reduction from baseline in in situ aromatase activity was seen in nine out of ten breast tumors exposed to letrozole 2.5 mg/day.
Plasma levels of estrone, estradiol and estrone sulfate were reduced from baseline by 74 to >95% in postmenopausal women with advanced breast cancer who received letrozole 0.1 to 5 mg/day. In addition, significantly greater suppression of estrone and estrone sulfate was seen with administration of letrozole 2.5 mg/day, compared with administration of anastrozole 1 mg/day. A significant reduction from baseline in endogenous estrogen levels (estrone plus estradiol levels) within breast tumors was seen with administration of letrozole 2.5 mg/day to postmenopausal women with breast cancer.
Letrozole showed antitumor activity in amousemodel of postmenopausal hormone-dependent breast cancer. Tumor weights were significantly lower in recipients of letrozole, compared with controls.
Letrozole is highly selective for aromatase. Administration of letrozole 0.1 to 2.5 mg/day to postmenopausal women with advanced breast cancer did not significantly alter serum levels of aldosterone, thyroxine, liothyronine (triiodothyronine), thyroid-stimulating hormone, cortisol, 17α-hydroxyprogesterone, androstenedione, luteinizing hormone or follicle-stimulating hormone.
No statistically significant differences between letrozole and placebo recipients were seen with regards to changes from baseline in lipid levels in a double-blind, randomized study in healthy postmenopausal women. Similarly, no significant changes from baseline in lipid levels were seen in a noncomparative study in women with no active breast disease. However, significant increases from baseline in total cholesterol and low-density lipoprotein cholesterol levels were seen in postmenopausal women with metastatic breast cancer who received letrozole 2.5 mg/day in another noncomparative study.
Levels of bone resorption markers (urinary pyridinoline and deoxypyridinoline or serum levels of C-telopeptide crosslinks) were significantly increased from baseline in two studies in postmenopausal women who received letrozole 2.5 mg/day for 3 or 6 months. Serum estradiol levels were significantly reduced (versus baseline or placebo) in these studies and it should be noted that bone mineral density was not measured. Further studies are needed to determine the clinical significance of the observed changes in bone resorption markers.
In a mouse model of postmenopausal hormone-dependent breast cancer, administration of letrozole 5 to 60 μg/day was associated with significantly lower uterine weights, compared with controls.
Pharmacokinetic Properties
A mean maximum plasma concentration of 107 nmol/L was achieved a median of 1.98 hours after administration of a single dose of letrozole 2.5mg to postmenopausal women with advanced breast cancer. The systemic absorption of letrozole was almost complete (systemic bioavailability of 99.9%) with a large volume of distribution (1.87 L/kg). The pharmacokinetics of letrozole 2.5 mg/day did not differ between younger (age range 52 to 66 years) and older (age range 70 to 76 years) postmenopausal women with advanced breast cancer, although a slight decrease in the rate, but not the extent, of letrozole absorption was seen in the fed, compared with the fasting, state in 12 healthy men.
The major route of elimination of letrozole is by metabolism, via the cytochrome P450 enzyme system, to a pharmacologically inactive carbinol metabolite. Approximately 90% of the administered letrozole dose was recovered in the urine as unchanged drug plus its metabolites.
Exposure to letrozole was significantly increased in patients with severe hepatic impairment who received a single dose of letrozole. Renal impairment did not affect the pharmacokinetics of letrozole in volunteers or in women with advanced breast cancer.
Compared with administration of letrozole alone, the letrozole area under the plasma concentration-time curve was significantly reduced by a mean of approximately 40% after concomitant administration of letrozole 2.5 mg/day and tamoxifen 20 mg/day in postmenopausal women with advanced breast cancer. However, the pharmacokinetics of tamoxifen were not significantly altered by concomitant administration of letrozole.
Therapeutic Efficacy
Letrozole is superior to tamoxifen in the first-line treatment of postmenopausal women with advanced breast cancer. In a double-blind, randomized, multicenter study involving postmenopausal women with advanced breast cancer, recipients of letrozole 2.5 mg/day were significantly less likely than recipients of tamoxifen 20 mg/day to experience disease progression (the primary endpoint) [hazards ratio (HR) 0.70, 95% confidence interval (CI) 0.60 to 0.82] or treatment failure (HR 0.71, 95% CI 0.61 to 0.82) and were significantly more likely to experience an objective response [odds ratio (OR) 1.71, 95% CI 1.26 to 2.31] or clinical benefit (OR 1.55, 95% CI 1.19 to 2.01). The survival rate was significantly higher in letrozole than in tamoxifen recipients at 1 (83 vs 75%) and 2 (62 vs 57%) years.
Letrozole is a cost effective alternative to first-line treatment with tamoxifen in postmenopausal women with advanced breast cancer, according to the results of Canadian and UK decision-analysis modelling studies. In the Canadian study, letrozole and anastrozole were associated with costs of $Canl2 500 and $Canl9 600 per quality-adjusted progression-free year gained, compared with tamoxifen. In the UK study, letrozole, compared with tamoxifen, had a mean incremental cost of £500 per life-year gained.
Letrozole is at least as effective as megestrol in the second-line treatment of postmenopausal women with advanced breast cancer, according to the results of two large, double-blind, randomized, multicenter studies. In these studies, postmenopausal women with advanced breast cancer received letrozole 0.5 or 2.5 mg/day or megestrol 160 mg/day (the women had received prior antiestrogen therapy). No significant difference between treatment arms in the objective response rate (primary endpoint) was seen in one study, while in the other study letrozole 2.5 mg/day was the superior treatment (letrozole 0.5 mg/day vs letrozole 2.5 mg/day OR 0.42, 95% CI 0.23 to 0.76 and letrozole 2.5 mg/day vs megestrol OR 1.82, 95% CI 1.02 to 3.25). The duration of objective response was significantly longer in letrozole 2.5 mg/day, compared with megestrol, recipients in this same study (33 vs 17.9 months). No significant between-group differences were seen in either study in the clinical benefit rate. In one study, a significantly lower risk of disease progression (HR 0.80, 95% CI 0.64 to 0.99) and treatment failure (HR 0.78, 95% CI 0.63 to 0.96) was seen in letrozole 0.5 mg/day, compared with megestrol, recipients, although there was no significant between-group difference in the time to death. In the other trial, the risks of disease progression (HR 1.35,95% CI 1.04 to 1.75), treatment failure (HR 1.47,95% CI 1.15 to 1.89) and death (HR 1.34 95% CI 1.02 to 1.76) were significantly higher in letrozole 0.5 mg/day, compared with letrozole 2.5 mg/day, recipients. In addition, the risk of treatment failure was significantly lower (HR 0.77, 95% CI 0.61 to 0.99) and the median duration of clinical benefit was significantly longer (23.5 vs 14.5 months) in letrozole 2.5 mg/day recipients than in megestrol recipients. Letrozole and megestrol recipients had similar health-related quality-of-life scores in these studies.
A third large, randomized, multicenter study examining the second-line treatment of postmenopausal women with advanced breast cancer compared letrozole 0.5 or 2.5mg once daily with aminoglutethimide 250mg twice daily. There were no significant between-group differences in objective response rate or the rate of clinical benefit, although the risks of disease progression (HR 0.72, 95% CI 0.57 to 0.92), treatment failure (HR 0.70, 95% CI 0.55 to 0.88) and death (HR 0.64, 95% CI 0.49 to 0.85) were significantly lower in letrozole 2.5 mg/day recipients than in aminoglutethimide recipients. In addition, the risk of death was significantly lower in letrozole 2.5 mg/day, compared with letrozole 0.5 mg/day, recipients (HR 0.74, 95% CI 0.56 to 0.98).
Second-line therapy with letrozole 2.5mg once daily, compared with anastrozole 1mg once daily, resulted in a significantly higher objective response rate (19.1 vs 12.3%; secondary endpoint) in postmenopausal women (n = 713) with locally advanced or metastatic breast cancer in a nonblind, randomized, multicenter study. There was no significant between-group difference in the time to disease progression (primary endpoint). Patient preference was greater for letrozole than for anastrozole in a single-blind crossover study.
A significantly higher objective response rate (31.2 vs 13.0 %; primary endpoint) was seen with administration of letrozole lmg once daily than with administration of the second-generation aromatase inhibitor fadrozole lmg twice daily in a double-blind, randomized, multicenter study in postmenopausal women with advanced breast cancer.
Subgroup analyses showed that second-line therapy with letrozole was effective in postmenopausal women with advanced breast cancer who had predominantly visceral metastases. Historically, hormonal therapy has been considered less effective in patients with visceral metastases, compared with those who have predominantly bone or soft tissue metastases.
Letrozole appears to be a cost-effective option in the second-line treatment of postmenopausal women with advanced breast cancer, although data from prospective studies are lacking.
Tolerability
Letrozole was generally well tolerated in postmenopausal women with advanced breast cancer with adverse events tending to be of mild-to-moderate severity. The most common drug-related adverse effects experienced by letrozole 0.5 or 2.5mg recipients included nausea (6 to 13%), hot flushes (3 to 16%), hair thinning (4 and 6%) and fatigue (3 to 6%).
Letrozole had similar tolerability to tamoxifen in the first-line treatment of postmenopausal women with advanced breast cancer. Thromboembolic adverse events, irrespective of whether or not they were related to drug therapy, occurred in 1% of letrozole recipients and 2% of tamoxifen recipients. Overall (both treatment groups), 7% of patients discontinued therapy (most of the discontinuations for adverse events were for tumor-related symptoms associated with disease progression).
In the second-line treatment of postmenopausal women with advanced breast cancer, letrozole 0.5 or 2.5 mg/day recipients were significantly less likely than megestrol recipients to experience body weight increase (3 and 4 vs 13%), appetite increase (2 and 1 vs 11%), dyspnea (24 and 23 vs 38%), vaginal bleeding (3 and 0.5 vs 8%) or cardiovascular adverse events (11 and 10 vs 20%). In contrast, significantly more letrozole 2.5 mg/day recipients, compared with letrozole 0.5 mg/day or megestrol recipients, experienced headache (23 vs 12 and 12%).
In the second-line treatment of postmenopausal women with advanced breast cancer, letrozole 0.5 and 2.5 mg/day recipients were less likely than aminoglutethimide recipients to experience drug-related rash (1 and 3 vs 11%), somnolence (3 and 3 vs 7%) or abdominal pain (2 and 0.5 vs 5%).
The pooled incidence of adverse events was significantly lower in letrozole 2.5mg once daily than in anastrozole lmg once daily recipients (43 vs 65%) in a single-blind crossover study in postmenopausal women with advanced breast cancer receiving second-line therapy.
Dosage and Administration
In the US and Europe, letrozole is currently indicated for the first-line treatment of postmenopausal women with locally advanced or metastatic breast cancer that is hormone receptor positive or of unknown receptor status and in the treatment of advanced breast cancer in postmenopausal women who have disease progression after antiestrogen therapy. The recommended oral dosage of letrozole is 2.5mg once daily. No dosage adjustment is needed in elderly patients. Dosage adjustment is not needed in patients with renal impairment if their creatinine clearance is >-0.6 L/h (>-10 ml/min), according to US prescribing information. While no dosage adjustment is needed in patients with mild-to-mo derate hepatic impairment, US and European prescribing information recommend caution in administering letrozole to patients with severe hepatic impairment.








Similar content being viewed by others
References
Njar VCO, Brodie AMH. Comprehensive pharmacology and clinical efficacy of aromatase inhibitors. Drugs 1999; 58: 233–55
Clemons M, Goss P.Estrogens and the risk of breast cancer. N Engl J Med 2001 Jan 25; 344(4): 276–85
Higa GM. New generation aromatase inhibitors in breast cancer. Pharmacoeconomics 2000 Feb; 17(2): 121–32
Buzdar AU. Endocrine therapy in the treatment of metastatic breast cancer. Semin Oncol 2001 Jun; 28(3): 291–304
Lamb HM, Adkins JC. Letrozole: a review of its use in postmenopausal women with advanced breast cancer. Drags 1998; 56: 1125–40
Cohen MH, Johnson JR, Li N, et al. Approval summary: letrozole in the treatment of postmenopausal women with advanced breast cancer. Clin Cancer Res 2002 Mar; 8(3): 665–9
Eiermann W, Paepke S, Appfelstaedt J, et al. Preoperative treatment of postmeno-pausal breast cancer patients with letrozole: a randomized double-blind multi-center study. Ann Oncol 2001 Nov; 12(11): 1527–32
Ellis MJ, Coop A, Singh B, et al. Letrozole is more effective neoadjuvant endocrine therapy than tamoxifen for ErbB-1- and/or ErbB-2-positive, estrogen receptor-positive primary breast cancer: evidence from a phase III randomized trial. J Clin Oncol 2001 Sep; 19(18): 3808–16
Dixon JM, Love CDB, Bellamy COC, et al. Letrozole as primary medical therapy for locally advanced and large operable breast cancer. Breast Cancer Res Treat 2001 Apr; 66: 191–9
Shaw HS, Ellis MJ. Letrozole in the treatment of breast cancer. Expert Opin Pharmacother 2002 May; 3(5): 607–17
Michaud LB, Buzdar AU. Risks and benefits of aromatase inhibitors in post-menopausal breast cancer. Drag Saf 1999; 21: 297–309
Miller WR. Biology of aromatase inhibitors: pharmacology/endocrinology within the breast. Endocr. Relat. Cancer. 1999; 6: 187–95
Miller WR, Dixon JM. Local endocrine effects of aromatase inhibitors within the breast. J Steroid Biochem Mol Biol 2001 Dec; 79(1-5): 93–102
Bhatnagar AS, Batzl C, Häusler A, et al. Pharmacology of nonsteroidal aromatase inhibitors. In: Pasqualini JR, Katzenellenbogen BS, editors. Hormone-dependent cancer. New York: Marcel Dekker, Inc., 1996: 155–68
Kao Y-C, Cam LL, Laughton CA, et al. Binding characteristics of seven inhibitors of human aromatase: a site-directed mutagenesis study. Cancer Res 1996; 56: 3451–60
Kudoh M, Susaki Y, Ideyama Y, et al. The potent and selective inhibition of estrogen production by non-steroidal aromatase inhibitor, YM511. J Steroid Biochem Mol Biol 1995; 54: 265–71
Dowsett M, Jones A, Johnston SRD, et al. In vivo measurement of aromatase inhibition by letrozole (CGS 20267) in postmenopausal patients with breast cancer. Clin Cancer Res 1995; 1: 1511–5
Lønning PE. Pharmacology of new aromatase inhibitors. Breast 1996; 5(3): 202–8
Geisler J, Haynes B, Anker G, et al. Influence of letrozole and anastrozole on total body aromatization and plasma estrogen levels in postmenopausal breast cancer patients evaluated in a randomized, cross-over study. J Clin Oncol 2002 Feb l; 20(3): 751–7
Iveson T J, Smith IE, Ahern J, et al. Phase I study of the oral nonsteroidal aromatase inhibitor CGS 20267 in healthy postmenopausal women. J Clin Endocrinol Metab 1993; 77: 324–31
Iveson T J, Smith IE, Ahern J, et al. Phase I study of the oral nonsteroidal aromatase inhibitor CGS 20267 in postmenopausal patients with advanced breast cancer. Cancer Res 1993; 53: 266–70
Lipton A, Demers LM, Harvey HA, et al. Letrozole (CGS 20267): a phase I study of a new potent oral aromatase inhibitor of breast cancer. Cancer 1995; 75: 2132–8
Demers LM. Effects of fadrozole (CGS 16949A) and letrozole (CGS 20267) on the inhibition of aromatase activity in breast cancer patients. Breast Cancer Res Treat 1994; 30(1): 95–102
Klein KO, Demers LM, Santner S J, et al. Use of ultrasensitive recombinant cell bioassay to measure estrogen levels in women with breast cancer receiving the aromatase inhibitor, letrozole. J Clin Endocrinol Metab 1995; 80: 2658–60
Lu Q, Liu Y, Long BJ, et al. The effect of combining aromatase inhibitors with antiestrogens on tumor growth in a nude mouse model for breast cancer. Breast Cancer Res Treat l999; 57: 183–92
Brodie A, Lu Q, Yue W, et al. Intratumoral aromatase model: the effects of letrozole (CGS 20267). Breast Cancer Res Treat 1998; 49(Suppl.): S23–6
Yue W, Wang J, Savinov A, et al. Effect of aromatase inhibitors on growth of mammary tumors in a nude mouse model. Cancer Res 1995; 55: 3073–7
Lu Q, Yue W, Wang J, et al. The effects of aromatase inhibitors and antiestrogens in the nude mouse model. Breast Cancer Res Treat 1998; 50: 63–71
Long B J, Jelovac D, Thiantanawat A, et al. The effect of second-line antiestrogen therapy on breast tumor growth after first-line treatment with the aromatase inhibitor letrozole: long-term studies using the intratumoral aromatase postmenopausal breast cancer model. Clin Cancer Res 2002 Jul; 8(7): 2378–88
Long B J, Jelovac D, Thiantanawat A, et al. The effect of alternating letrozole and tamoxifen in comparison to sequential treatment with each drug alone or in combination [abstract no. 444 and poster]. Breast Cancer Res Treat 2001 Oct; 69(3): 287
Schieweck K, Bhatnagar AS, Batzl C, et al. Anti-tumor and endocrine effects of non-steroidal aromatase inhibitors on estrogen-dependent rat mammary tumors. J Steroid Biochem Mol Biol 1993; 44: 633–6
Bajetta E, Zilembo N, Dowsett M, et al. Double-blind, randomised, multicentre endocrine trial comparing two letrozole doses, in postmenopausal breast cancer patients. Eur J Cancer 1999; 35: 208–13
Heshmati HM, Khosla S, Robins SP, et al. Role of low levels of endogenous estrogen in regulation of bone resorption in late postmenopausal women. J Bone Miner Res 2002 Jan; 17(1): 172–8
Harper-Wynne C, Ross G, Sacks N, et al. Effects of the aromatase inhibitor letrozole on normal breast epithelial cell proliferation and metabolic indices in postmenopausal women: a pilot study for breast cancer prevention. Cancer Epidemiol Biomarkers Prev 2002 Jul; 11(7): 614–21
Elisaf MS, Bairaktari ET, Nicolaides C, et al. Effect of letrozole on the lipid profile in postmenopausal women with breast cancer. Eur J Cancer 2001; 37: 1510–3
Brodie A, Lu Q, Long B. Aromatase and its inhibitors. J Steroid Biochem Mol Biol 1999; 69: 205–10
Pfister CU, Martoni A, Zamagni C, et al. Effect of age and single versus multiple dose pharmacokinetics of letrozole (Femara) in breast cancer patients. Biopharm Drug Dispos 2001 Jul; 22(5): 191–7
Sioufi A, Gauducheau N, Pineau V, et al. Absolute bioavailability of letrozole in healthy postmenopausal women. Biopharm Drug Dispos 1997; 18: 779–89
Colussi DM, Parisot CY, Lefevre GY. Plasma protein binding of letrozole, a new nonsteroidal aromatase enzyme inhibitor. J Clin Pharmacol 1998; 38: 727–35
Sioufi A, Sandrenan N, Godbillon J, et al. Comparative bioavailabilityof letrozole under fed and fasting conditions in 12 healthy subjects after a 2.5 mg single oral administration. Biopharm Drug Dispos 1997; 18: 489–97
Novartis. Femara® (letrozole tablets) prescribing information [online]. Available from URL: http://www.femara.com [Accessed 2001 Jul 18]
Wirz B, Valles B, Parkinson A, et al. CYP3A4 and CYP2A6 are involved in the biotransformation of letrozole (®Femara) [abstract]. 7th North American Meeting of the International Society for the Study of Xenobiotics; 1996 Oct 20–24; San Diego (CA), 40
Pfister CU, Horak J, Horejsova M, et al. Pharmacokinetics of Femara® in subjects with severe liver impairment [abstract no. 2926]. Proceedings of the American Association for Cancer Research 2001 Mar; 42: 544
Dowsett M, Pfister C, Johnston SR, et al. Impact of tamoxifen on the pharmacokinetics and endocrine effects of the aromatase inhibitor letrozole in postmenopausal women with breast cancer. Clin Cancer Res 1999; 5: 2338–43
Ingle JN, Suman VJ, Johnson PA, et al. Evaluation of tamoxifen plus letrozole with assessment of pharmacokinetic interaction in postmenopausal women with metastatic breast cancer. Clin Cancer Res 1999; 5: 1642–9
Morgan JM, Palmisano M, Spencer S, et al. Pharmacokinetic effect of cimetidine on a single 2.5 mg dose of letrozole in healthy subjects [abstract no. 26]. J Clin Pharmacol 1996; 36: 852
Mouridsen H, Gershanovich M, Sun Y, et al. Superior efficacy of letrozole versus tamoxifen as first-line therapy for postmenopausal women with advanced breast cancer: results of a phase III study of the International Letrozole Breast Cancer Group. J Clin Oncol 2001; 19: 2596–606
Mouridsen H, Sun Y, Gershanovich M, et al. First-line therapy with letrozole (Femara®) for advanced breast cancer prolongs time to worsening of Karnofsky Performance Status (KPS) compared with tamoxifen [abstract no. 458 and poster]. Breast Cancer Res Treat 2001 Oct; 69(3): 291
Dranitsaris G, Verma S, Trudeau M. Cost utility of first line hormonal therapy in advanced breast cancer: a comparison of two aromatase inhibitors to tamoxifen [poster]. 24th Annual San Antonio Breast Cancer Symposium; 2001 Dec 10–13; San Antonio (TX)
Karnon JD, Jones TED. A stochastic economic evaluation of letrozole versus tamoxifen as a first-line therapy for postmenopausal women with advanced breast cancer [abstract no. 853]. Eur J Cancer 2001 Oct; 37(Suppl. 6): S232
Gershanovich M, Chaudri HA, Campos D, et al. Letrozole, a new oral aromatase inhibitor: randomised trial comparing 2.5 mg daily, 0.5 mg daily and aminoglutethimide in postmenopausal women with advanced breast cancer. Ann Oncol 1998; (9): 639-45
Dombernowsky P, Smith I, Falkson G, et al. Letrozole, a new oral aromatase inhibitor for advanced breast cancer: double-blind randomized trial showing a dose effect and improved efficacy and tolerability compared with megestrol acetate. J Clin Oncol 1998; 16: 453–61
Buzdar A, Douma J, Davidson N, et al. Phase III, multicenter, double-blind, randomized study of letrozole, an aromatase inhibitor, for advanced breast cancer versus megestrol acetate. J Clin Oncol 2001 Jul 15; 19(14): 3357–66
Rose C, Vtoraya O, Pluzanska A, et al. Letrozole (Femara) vs. anastrozole (Arimidex): second-line treatment in postmenopausal women with advanced breast cancer [abstract no. 131]. Proceedings of the American Society of Clinical Oncology 2002; 21 (Pt 1): 34a
Tominaga T, Morimoto T, Ohashi J, et al. A pivotal double-blind trial in Japan of an aromatase inhibitor letrozole (third generation) vs. its predecessor fadrozole hydrochloride (second generation): Japan Letrozole Study Group [abstract no. 100]. Ann Oncol 2000; 11(Suppl. 4): 25
Ingle JN, Johnson PA, Suman VJ, et al. A randomized phase II trial of two dosage levels of letrozole as third-line hormonal therapy for women with metastatic breast carcinoma. Cancer 1997; 80: 218–24
Tominaga T, Ohashi Y, Abe R, et al. Phase II trial of letrozole (a novel oral nonsteroidal aromatase inhibitor) in postmenopausal patients with advanced or recurrent breast cancer [abstract no. 490]. Eur J Cancer 1998; (31 A): S81
Chaudri HA, Trunet PF. Letrozole: updated duration of response [letter]. J Clin Oncol 1999; 17: 3856–60
Gershanovich M, Chaudri HA, Hornberger U, et al. Comparison of letrozole 2.5 mg (Femara®) with megestrol acetate (MA) and with aminoglutethimide (AG) in patients with visceral disease [abstract no. 212]. Breast Cancer Res Treat 1998;46: 53
Gardin G, Fornasiero A, Romieu G, et al. Long duration of response with letrozole 2.5 mg (Femara®) in two trials in postmenopausal women with advanced breast cancer after anti-estrogen therapy [abstract no. 46]. Eur J Cancer 1998 Sep; 34(Suppl.5): S13–4
Possinger K, Schmid P, Wischnewsky MB. Letrozole is highly effective in patients with soft tissue metastases [abstract no. 171]. Breast Cancer Res Treat 2000; 64: 53
Wischnewsky MB, Schmid P, Boehm R, et al. Letrozole and megestrol acetate in patients with advanced breast cancer resistant to tamoxifen [abstract no. 174]. Breast Cancer Res Treat 2000; 64: 54
Thomas R, Makris A, Bloomfield D, et al. Empowering patients to make informed treatment decisions based on tolerability, quality of life patient preference: a comparison of letrozole and anastrozole in a multicentre, randomised, single-blind cross over study [abstract no. 171 and poster]. Eur J Cancer 2002 Mar; 38(Suppl.3): S83
Nuijten M, Meester L, Waibel F, et al. Cost effectiveness of letrozole in the treatment of advanced breast cancer in postmenopausal women in the UK. Pharmacoeconomics 1999; 16(4): 379–91
Nuijten M, McCormick J, Waibel F, et al. Economic evaluation of letrozole in the treatment of advanced breast cancer in postmenopausal women in Canada. Value Health 2000; 3(1): 31–9
Dranitsaris G, Leung P, Mather J, et al. Cost-utility analysis of second-line hormonal therapy in advanced breast cancer: a comparison of two aromatase inhibitors to megestrol acetate. Anticancer Drugs 2000; 11: 591–601
European Agency for the Evaluation of Medicinal Products. European summary of product characteristics for letrozole [online]. Available from URL: http://www.emea.eu.int [Accessed 2002 Sep 12]
Lønning PE. Is there a growing role for endocrine therapy in the treatment of breast cancer? Drugs 2000; 60: 11–21
National Comprehensive Cancer Network. NCCN Practice Guidelines for Breast Cancer. Oncology 2000 Nov; 14(11 A): 33–49
National Comprehensive Cancer Network. NCCN Practice Guidelines for Breast Cancer [online]. Available from URL: http://www.nccn.org [Accessed 2002 Sep 11]
Bonneterre J, Thürlimann B, Robertson JFR, et al. Anastrozole versus tamoxifen as first-line therapy for advanced breast cancer in 668 postmenopausal women: results of the Tamoxifen or Arimidex Randomized Group Efficacy and Tolerability study. J Clin Oncol 2000 Nov 15; 18: 3748–57
Nabholtz JM, Buzdar A, Pollak M, et al. Anastrozole is superior to tamoxifen as first-line therapy for advanced breast cancer in postmenopausal women: results of a North American multicenter randomized trial. J Clin Oncol 2000 Nov 15; 18: 3758–67
Buzdar A, Nabholtz JM, Robertson JF, et al. Anastrozole (Arimidex) versus tamoxifen as first-line therapy for advanced breast cancer (Abc) in postmenopausal (Pm) women - combined analysis from two identically designed multicenter trials [abstract no. 609D]. Proceedings of the American Society of Clinical Oncology 2000; 19: 154
Thürlimann B, Beretta K, Bacchi M, et al. First-line fadrozole HC1 (CGS 16949A) versus tamoxifen in postmenopausal women with advanced breast cancer: prospective randomised trial of the Swiss Group for Clinical Cancer Research SAKK 20/88. Ann Oncol 1996; 7: 471–9
Falkson CI, Falkson HC. A randomised study of CGS-16949A (fadrozole) versus tamoxifen in previously untreated postmenopausal patients with metastatic breast cancer. Ann Oncol 1996; 7: 465–9
Paridaens R, Dirix LY, Beex L, et al. Exemestane (Aromasin) is active and well tolerated as first-line hormonal therapy (HT) of metastatic breast cancer (MBC) patients (Pts): results of a randomized phase II trial [abstract no. 316]. Proceedings of the American Society of Clinical Oncology 2000; 19: 83
Jonat W, Howell A, Blomqvist C, et al. A randomised trial comparing two doses of the new selective aromatase inhibitor anastrozole (Arimidex) with megestrol acetate in postmenopausal patients with advanced breast cancer. Eur J Cancer 1996; 32A: 404–12
Buzdar AU, Jones SE, Vogel CL, et al. A phase III trial comparing anastrozole (1 and 10 milligrams), a potent and selective aromatase inhibitor, with megestrol acetate in postmenopausal women with advanced breast carcinoma. Cancer 1997 Feb 15; 79: 730–9
Buzdar AU, Jonat W, Howell A, et al. Anastrozole versus megestrol acetate in the treatment of postmenopausal women with advanced breast carcinoma: results of a survival update based on a combined analysis of data from two mature phase III trials. Cancer 1998 Sep 15; 83: 1142–52
Buzdar AU, Smith R, Vogel C, et al. Fadrozole HC1 (CGS-16949A) versus megestrol acetate treatment of postmenopausal patients with metastatic breast carcinoma: results of two randomized double-blind controlled multiinstitutional trials. Cancer 1996 Jun 15; 77: 2503–13
Kvinnsland S, Anker G, Dirix L-Y, et al. High activity and tolerability demonstrated for exemestane in postmenopausal women with metastatic breast cancer who had previously failed on tamoxifen treatment. Eur J Cancer 2000; 36: 976–82
Kaufmann M, Bajetta E, Dirix LY, et al. Exemestane is superior to megestrol acetate after tamoxifen failure in postmenopausal women with advanced breast cancer: results of a phase III randomized double-blind trial. J Clin Oncol 2000 Apr; 18: 1399–411
Thürlimann B, Castiglione M, Hsu-Schmitz SF, et al.Formestane versus megestrol acetate in postmenopausal breast cancer patients after failure of tamoxifen: a phase III prospective randomised cross over trial of second-line hormonal treatment (SAKK 20/90). Eur J Cancer 1997; 33: 1017–24
Lipton A, Ali SM, Leitzel K, et al. Elevated serum HER-2/neu level predicts decreased response to hormone therapy in metastatic breast cancer. J Clin Oncol 2002 Mar 15; 20(6): 1467–72
Goss PE, Strasser K. Aromatase inhibitors in the treatment and prevention of breast cancer. J Clin Oncol 2001 Feb 1; 19(3): 881–94
Author information
Authors and Affiliations
Corresponding author
Additional information
Various sections of the manuscript reviewed by: S. Chan, Department of Clinical Oncology, City Hospital, Nottingham, United Kingdom; M. de Lena, Operative Unit of Medical Oncology, Oncology Institute, Bari, Italy; J.M. Dixon, Breast Research Unit, Western General Hospital, Edinburgh, United Kingdom; W.J. Gradishar, Robert H. Lurie Comprehensive Cancer Center, Northwestern University, Chicago, Illinois, USA; H.T. Mouridsen, Department of Oncology, The Finsen Center, Copenhagen, Denmark; S. Pyrhönen, Department of Oncology and Radiotherapy, Turku University Central Hospital, Turku, Finland.
Data Selection
Sources: Medical literature published in any language since October 1998 on Letrozole, identified using Medline and EMBASE, supplemented by AdisBase (a proprietary database of Adis International). Additional references were identified from the reference lists of published articles. Bibliographical information, including contributory unpublished data, was also requested from the company developing the drug.
Search strategy: Medline search terms were ‘Letrozole’ or ‘CGS 20267’. EMBASE search terms were ‘Letrozole’ or ‘CGS 20267’. AdisBase search terms were ‘Letrozole’ or ‘CGS 20267’. Searches were last updated Sep 20 2002.
Selection: Studies in patients with breast cancer who received Letrozole. Inclusion of studies was based mainly on the methods section of the trials. When available, large, well controlled trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic.
Index terms: Letrozole, breast cancer, pharmacodynamics, pharmacokinetics, therapeutic use, tolerability, dosage and administration.
Rights and permissions
About this article
Cite this article
Keating, G.M., Jarvis, B. Letrozole. Am J Cancer 1, 351–371 (2002). https://doi.org/10.2165/00024669-200201050-00007
Published:
Issue Date:
DOI: https://doi.org/10.2165/00024669-200201050-00007