Abstract
Background: The ongoing Type 1 Diabetes Prediction and Prevention Project in Finland (DIPP) is based on screening of genetic type 1 diabetes mellitus susceptibility, subsequent autoantibody follow-up and experimental preventive treatment with nasal insulin.
Objective: To analyse direct costs of type 1 diabetes prevention therapy with nasal insulin as it is now being studied in the DIPP project, and as it might be used as a part of routine healthcare in Finland.
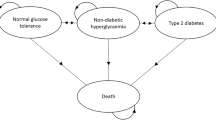
Data and methods: For the purposes of cost analysis, two different diabetes prevention models were constructed. The research-oriented model followed accurately the DIPP protocol and the practice-oriented model was based on the estimates of a panel of experts on how the prevention would be conducted as a part of the routine healthcare in Finland. To take into account the uncertainty and variability attached to the use of resources, a Monte Carlo simulation model was utilised. The costs of the two models comprising 500 iterations each were simulated using the Monte Carlo model.
Study perspective: This study was performed from the healthcare provider’s viewpoint.
Results: The total direct costs per person of the research-oriented model were 2102 and 1676 euros (EUR) in the first and second year and those of the practice-oriented model EUR827 and EUR675, respectively (EUR1 ≈ $US1.1; 2002 values). Subsequently, the costs rose only as a result of the increased use of insulin as the children grew older. After the 15th year, when the age structure of the population in the study had stabilised, the annual direct costs per person were EUR1798 (research-oriented model) and EUR797 (practice-oriented model).
Conclusions: The costs of prevention with nasal insulin are low when compared with estimates of the annual healthcare costs of type 1 diabetes. This study suggests, with some critical assumptions (in particular, that nasal insulin is effective in the prevention of type I diabetes), that a 2 to 3-year delay in the disease onset may make prevention according to the practice-oriented model cost saving.






Similar content being viewed by others
References
Kupila A, Muona P, Simell T, et al. Feasibility of genetic and immunological prediction of type I diabetes in a population-based birth cohort. Diabetologia 2001; 44: 290–7
Nejentsev S, Sjöroos M, Soukka T, et al. Population based genetic screening for type 1 diabetes mellitus risk in Finland: selective genotyping of the markers in the HLA-DQB1, HLA-DQA1 and HLA-DRB1 loci. Diabet Med 1999; 16: 985–92
Rewers M, Bugawan TL, Norris JM, et al. Newborn screening for HLA markers associated-with IDDM: diabetes autoimmunity study in the young (DAISY). Diabetologia 1996; 39: 807–12
Bowman MA, Leiter EH, Atkinson MA. Prevention of diabetes in the NOD mouse: implications for therapeutic intervention in human disease. Immunol Today 1994; 15: 115–20
Hahl J, Simell T, Ilonen J, et al. Costs of predicting IDDM. Diabetologia 1998; 41: 79–85
Vose D. Risk analysis: a quantitative guide. 2nd ed. Chichester: John Wiley & Sons, 2001
Kleijnen J, van Groenendaal W. Simulation: a statistical perspective. Chichester: John Wiley & Sons, 1992
Law AM, Kelton WD. Simulation modeling and analysis. New York: McGraw-Hill, 1982
Koopmanschap MA, Rutten FFH. The impact of indirect costs on outcomes of health care programs. Health Econ 1994; 3: 385–93
Koopmanschap MA, Rutten FFH, van Ineveld BM, et al. The friction cost method for measuring indirect costs of disease. J Health Econ 1995; 14: 171–89
Posnett J, Jan S. Indirect cost in economic evaluation: the opportunity cost of unpaid inputs. Health Econ 1996; 5: 13–23
Drummond MF, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press, 1987
Luce RB, Elixhauser A. Estimating costs in the economic evaluation of medical technologies. Int J Technol Assess Health Care 1990; 6: 57–75
Robinson R. Economic evaluation and health care: costs and cost-minimisation analysis. BMJ 1993; 307: 726–8
Heikkinen K, Hujanen T, Rusama H. Terveydenhuollon yksikkökustannukset Suomessa vuonna 2000 (Unit costs in Finnish health care in 2000) [in Finnish]. Helsinki: Stakes Aiheita, 2001
Turun Yliopistollinen Keskussairaala. TYKS tilastot 1999 (Turku University Central Hospital statistics, 1999) [in Finnish]. Turku: Turun Yliopistollinen Keskussairaala, 2000
Turun Yliopistollinen Keskussairaala. Yhteenveto vuoden 1999 kustannuslaskennasta (Turku University Central Hospital, summary of year 1999 cost accounting) [in Finnish]. Turku: Turun Yliopistollinen Keskussairaala, 2000
Palisade Corporation. @RISK advanced risk analysis for spreadsheets. Newfield: Palisade Corporation, 1996
Kangas T. The consumption and direct costs of health care services among persons with diabetes in Helenski. A case controlled cross-sectional study of the fiscal year 1997 [in Finnish with an English summary]. Studies in social security and health, 67. Helenski: The Social Insurance Institution, 2002
Acknowledgements
This study has been supported by Yrjö Jahnsson Foundation, Oskar Öflund Foundation, STAKES/FinOHTA, Foundation for Economic Education, Juvenile Diabetes Research Foundation International (grant # 4-1999-731 to O.S.), Diabetes Research Foundation Finland, Ane and Signe Gyllenberg Foundation, and Turku School of Economics and Business Administration. The authors thank Professor Harri Sintonen for his valuable comments and the DIPP staff and Alpo Rajaniemi for their help in compiling the data. The authors have no conflicts of interest directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hahl, J., Simell, T., Kupila, A. et al. A Simulation Model for Estimating Direct Costs of Type 1 Diabetes Prevention. Pharmacoeconomics 21, 295–303 (2003). https://doi.org/10.2165/00019053-200321050-00001
Published:
Issue Date:
DOI: https://doi.org/10.2165/00019053-200321050-00001