Summary
Abstract
Cost estimates from developed countries indicate that asthma accounts for up to 2% of the economic cost of all diseases. A large proportion of asthma-related costs are attributable to poor asthma control. Treatment strategies which improve clinical outcomes in patients with asthma, therefore, have the potential for significant economic benefits, and it is important to evaluate new asthma therapies for cost effectiveness.
Several studies have established that salmeterol and fluticasone propionate combined in a single dry powder inhalation device are at least as effective as a combination of the 2 drugs administered via separate dry powder inhalers and more effective than monotherapy with fluticasone propionate or budesonide. Importantly, pharmacoeconomic analysis of several of these studies show that the salmeterol/fluticasone propionate combination is cost effective relative to monotherapy with fluticasone propionate or budesonide. Although the total cost of asthma management tended to be slightly higher with salmeterol/fluticasone propionate than with inhaled corticosteroid monotherapy, in most cases mean costeffectiveness ratios were lower (i.e. more favourable) for salmeterol/fluticasone propionate than either fluticasone propionate or budesonide. Cost effectiveness was assessed according to 3 end-points: successfully treated weeks, symptom free days and episode-free days. Mean cost-effectiveness ratios consistently favoured salmeterol/fluticasone propionate over the comparator drug for the endpoint successfully treated weeks, and in most cases the other 2 end-points also favoured the combination product over the comparator. In a further study, salmeterol/fluticasone was also less costly than therapy with formoterol and budesonide administered via 2 separate inhalers.
Studies of health-related quality of life (HR-QOL) using the Asthma Quality of Life Questionnaire indicate that salmeterol/fluticasone propionate produces clinically meaningful improvements in overall HR-QOL relative to salmeterol monotherapy or placebo. Improvements in overall HR-QOL were statistically significantly greater for salmeterol/fluticasone propionate than with fluticasone propionate or budesonide alone, although the differences between treatments did not exceed the threshold for clinical significance.
In conclusion, short term cost-effectiveness data show that salmeterol/ fluticasone propionate is more cost effective than the inhaled corticosteroids budesonide and fluticasone propionate alone. The combination product also appears to improve HR-QOL relative to placebo or salmeterol alone.
Burden of Asthma
Asthma is among the most common chronic diseases in industrialised countries and its prevalence continues to increase. Even though effective treatments are available, asthma-related mortality is also increasing in certain subpopulations in the US, but appears to have stabilised in several other countries. Reasons for the increasing prevalence of asthma are unknown.
Asthma is a chronic inflammatory disease. Among affected adults, lung function declines over time to a greater extent, and mortality rates are somewhat higher, than in individuals without asthma. It is estimated that ≈75% of patients with asthma have clinically mild or seasonal asthma, 15 to 20% have moderate persistent asthma and the remainder severe persistent asthma.
Cost estimates from developed countries indicate that asthma accounts for up to 2% of the economic cost of all diseases and that direct costs account for most of the total expenditures on asthma. However, the proportion of total direct costs accounted for by various items of healthcare varies widely between countries. The direct costs of managing patients with poorly controlled asthma are high and reflect the frequent requirement for costly interventions. Indeed, a large proportion of all asthma-related costs are attributable to poor asthma control. Disease severity is also an important determinant of cost. The under utilisation of prophylactic therapy by patients with mild to moderate disease may also increase the rate of exacerbations and require more costly interventions.
Health-related quality-of-life (HR-QOL) questionnaires generally show that asthma impairs physical ability relative to patients without asthma. In addition, patients with similar symptoms perceive the effects of the disease differently, depending on their ability to discern changes in symptoms and their lifestyle. Both generic and disease-specific quality-of-life instruments show that the impact of asthma worsens as disease severity increases.
Clinical Overview of Inhaled Salmeterol/Fluticasone Propionate
On the basis of evidence of a complementary effect, and because compliance with inhaled asthma medication has been shown to be generally poor, the long acting β2-agonist salmeterol and the corticosteroid fluticasone propionate have been combined in a single, multiple dose, dry powder inhalation device, hereafter referred to as salmeterol/fluticasone propionate.
Inhaled salmeterol/fluticasone propionate has been compared with salmeterol and/or fluticasone propionate in several double-blind studies in patients with asthma previously treated with inhaled corticosteroids. In all trials the same dosage of salmeterol (50µg twice daily) was combined (where applicable) with various dosages of fluticasone propionate (100, 250 or 500µg twice daily).
Studies comparing salmeterol/fluticasone propionate with the same dosages of salmeterol and fluticasone propionate via 2 separate inhalation devices (hereafter referred to as concurrent salmeterol and fluticasone propionate) found no significant difference between the 2 regimens in terms of morning peak expiratory flow rate (PEF) [35 to 43 L/min improvement in salmeterol/fluticasone propionate recipients vs 33 to 36 L/min in salmeterol plus fluticasone propionate recipients]. Forced expiratory volume in 1 second (FEV1) also improved to a similar extent with each treatment (0.23 to 0.29L increases with salmeterol/fluticasone propionate vs 0.23 to 0.26L increases with salmeterol plus fluticasone propionate).
As might be expected, salmeterol/fluticasone propionate was significantly more effective than placebo, and salmeterol or fluticasone alone.
Salmeterol/fluticasone propionate also improved daytime symptomscores versus baseline in all studies and was at least as effective in this regard as concurrent salmeterol and fluticasone propionate administered via separate inhalers.
Studies have also compared salmeterol/fluticasone propionate with the inhaled corticosteroid budesonide. The combination was more effective than budesonide alone in terms of morning PEF with a difference between the 2 treatment groups of 11 and 25 L/min after 12 and 24 weeks treatment, respectively. Mean clinic FEV1 measurements and symptom scores also improved with both treatments. In a further study, salmeterol/fluticasone propionate was as effective in improving morning PEF as budesonide plus formoterol administered via separate inhalers. The mean percentage of symptom-free days increased similarly in both treatment groups; however, salmeterol/fluticasone propionate was statistically significantly more effective than budesonide plus formoterol in improving nighttime asthma symptom control over the 3-month treatment period.
As salmeterol/fluticasone propionate is a combination of 2 drugs, the type and severity of adverse events associated with each component drug may be expected in patients receiving the combination product. Importantly, there is no evidence of additional adverse events following concurrent administration of the two drugs.
Analysis of tolerability data from clinical trials indicates that the most frequent adverse events associated with salmeterol/fluticasone propionate are headache (incidence 2 to 5%), throat irritation (1 to 4%), hoarseness (2 to 4%) and candidiasis (unspecified site 2 to 3%, oral 1 to 4%).
Pharmacoeconomic Analyses
Data from 3 clinical studies, each comparing a different dosage of salmeterol/fluticasone propionate (50/100, 50/250 or 50/500µg twice daily) with the corresponding dosage of fluticasone propionate alone, have been subjected to cost-effectiveness analysis. These analyses were conducted according to the endpoints successfully treated week, symptom-free day and episode-free day. Studies were conducted from the perspective of the Swedish healthcare system using 1998 costs and considered only direct costs, comprising hospital and general practitioner contacts and medication costs.
The total cost of asthma management was slightly higher in salmeterol/fluticasone propionate recipients versus the fluticasone propionate group in all 3 studies, primarily because of a higher drug acquisition cost.
In all 3 studies, salmeterol/fluticasone propionate was associated with lower costs per successfully treated week compared with fluticasone propionate monotherapy. Salmeterol/fluticasone propionate 50/250µg, but not 50/100µg, twice daily had a lower (i.e. more favourable) cost-effectiveness ratio for the episode free day and symptom-free day end-points versus the corresponding dosage of fluticasone propionate monotherapy. The 50/500µg twice daily dosage of the combination had a lower cost-effectiveness ratio than fluticasone propionate 500µg twice daily in terms of symptom-free days, but not episode-free days.
Incremental cost-effectiveness ratios for salmeterol/fluticasone propionate ranged between 3.9 Swedish kronor [SEK ($US0.47)] per additional symptom-free day in the salmeterol/fluticasone propionate 50/250µg versus fluticasone propionate 250µg study and SEK66.8 ($US8.10) per day in the salmeterol/ fluticasone propionate 50/500µg versus fluticasone propionate 500µg study. In these studies, the benchmark for an acceptable incremental cost per symptom-free day was $US5, based on the previous findings of Rutten-van Mölken et al.
In all 3 studies sensitivity analyses did not change the overall inferences, indicating that the results were robust to assumptions used in the economic analyses.
A 24-week clinical study comparing salmeterol/fluticasone propionate with budesonide has been subjected to cost-effectiveness analyses from a Swedish, German and UK perspective. Each analysis found salmeterol/fluticasone propionate to be more cost effective than budesonide. The cost per additional successfully treated week was lower for salmeterol/fluticasone propionate compared with budesonide in all 3 analyses. The Swedish and UK study reports included cost-effectiveness data for the episode-free day end-point which also indicated a significant advantage for salmeterol/fluticasone propionate over budesonide.
A study that compared salmeterol/fluticasone propionate with formoterol plus budesonide (administered via 2 separate inhalers) prospectively collected data pertaining to healthcare resource utilisation from the perspective of the Norwegian healthcare system. PEF in the week prior to the end of treatment, the primary efficacy outcome, was similar in both treatment groups. Importantly, salmeterol/fluticasone propionate was significantly less costly in terms of total asthma management costs than therapy with formoterol and budesonide.
Quality-of-Life Assessments
The efficacy of salmeterol/fluticasone propionate therapy in terms of improvement in HR-QOL, as measured by responses to the Asthma Quality of Life Questionnaire (AQLQ), has been evaluated in double-blind clinical trials, 2 based on US data and 1 based on multinational data.
In the first US trial, analysis of responses after 12 weeks showed clinically meaningful improvements in overall HR-QOL scores and in the 4 subscales of the AQLQ in patients receiving salmeterol/fluticasone propionate compared with values in patients receiving salmeterol alone or placebo. Improvements in total AQLQ and all but the activity limitation subscale score were also significantly greater with the combination than with fluticasone propionate alone (250µg twice daily), although the differences between each regimen were only clinically meaningful for one of the subscales (emotional function).
In the second US trial, salmeterol/fluticasone propionate 50/l00µg twice daily produced significantly greater improvements in overall AQLQ score than twice daily salmeterol 50µg or fluticasone propionate 100µg alone or placebo. The differences between treatments were considered clinically meaningful (a difference between groups in mean change from baseline of 7≥0.5) when the combination was compared with placebo (difference between groups 1.3) or salmeterol (1.0) but not fluticasone propionate (0.43).
The multinational trial compared the effects of salmeterol/fluticasone propionate 50/250µg twice daily on HR-QOL with those of budesonide 800µg twice daily. Salmeterol/fluticasone propionate improved overall AQLQ and the symptom subscore to a significantly (p < 0.05) greater extent than budesonide; however, the respective 0.27 and 0.32 differences observed between the 2 treatments were not considered clinically meaningful.







Similar content being viewed by others
Notes
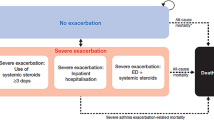
Defined as an increase of 3 puffs/day of as-needed salbutamol over baseline and/or night-time awakening because of asthma and/or a 20% decrease in PEF relative to baseline on ≤2 consecutive days.
References
National Institutes of Health. Global Initiative for Asthma. Global strategy for asthma management and prevention NHLB/ WHO workshop report [online]. Global Initiative for Asthma and National Heart, Lung and Blood Institute, 1995 Jan. Available from: URL: http://www.ginasthma.com/workshop/default.html [Accessed 1999 May 5]
National Heart Lung and Blood Institute. Data fact sheet: asthma statistics [online]. Available from: http://www.nhlbi.nih.gov/health/prof/lung/asthma/asthstat.htm [Accessed 2000 Nov 29]
Hartert TV, Peebles Jr RS. Epidemiology of asthma: the year in review. Curr Opin Pulm Med 2000; 6: 4–9
Lenney W, Wells NEJ, O’Neill BA. The burden of paediatric asthma. Eur Resp Rev 1994 Jan; 4: 49–62
Peat JK, van den Berg RE, Green WF, et al. Changing prevalence of asthma in Australian children. BMJ 1994 Jun 18; 308 (6944): 1591–6
Sly RM, O’Donnel R. Stabilization of asthma mortality. Ann Allergy Asthma Immunol 1997; 78: 347–54
Mannino DM, Homa DM, Pertowski CA, et al. Surveillence for asthma- United States, 1960–1995. Morb Mortal Wkly Rep 1998 Apr; 47 (1): 1–27
Lang DM, Polansky M. Patterns of asthma mortality in Philadelphia from 1969 to 1991. N Engl J Med 1994; 331: 1542–6
Campbell MJ, Cogman GR, Holgate ST, et al. Age specific trends in asthma mortality in England and Wales, 1983–95: results of an observational study. BMJ 1997; 314: 1439–41
Peat JK, Li J. Reversing the trend: reducing the prevalence of asthma. J Allergy Clin Immunol 1999 Jan; 103 (1 Pt 1): 1–10
Sly RM. Changing prevalence of allergic rhinitis and asthma. Ann Allergy Asthma Immunol 1999; 82: 233–52
Lamb H, Culy C, Faulds D. Inhaled fluticasone propionate: a pharmacoeconomic review of its use in the management of asthma. Pharmacoeconomics 2000 Nov; 18 (5): 487–510
Suissa S, Ernst P, Benayoun S, et al. Low-dose inhaled corticosteroids and the prevention of death from asthma. N Engl J Med 2000 Aug 3; 343: 332–6
Sullivan SD. Cost-effectiveness of drug interventions. Eur Resp Rev 1996; 6 (35): 116–8
Grol MH, Gerritsen J, Postma DS, et al. Asthma: from childhood to adulthood. Allergy 1996; 51: 855–69
Lange P, Parner J, Vestbo J, et al. A 15-year follow-up study of ventilatory function in adults with asthma. N Engl J Med 1998; 339: 1194–200
Lange P, Ulrik CS, Vestbo J, et al. Mortality in adults with self-reported asthma. Lancet 1996; 347: 1285–9
Reed CE. The natural history of asthma in adults: the problem of irreversibility. J Allergy Clin Immunol 1999 Apr; 103 (4): 539–49
Jacobson L, Hertzman P, Lofdahl CG, et al. The economic impact of asthma and chronic obstructive pulmonary disease (COPD) in Sweden in 1980 and 1991. Respir Med 2000 Mar; 94: 247–55
Woo J, Cockram C. Cost estimates for chronic diseases. Dis Manage Health Outcomes 2000 Jul; 8: 29–41
Lundback B, Pieters WR, Johansson G, et al. Cost-effectiveness analyses of salmeterol/fluticasone propionate combination product and fluticasone propionate in patients with asthma. I: introduction and overview. Pharmacoeconomics 1999; 16 Suppl. 2: 1–8
Jarvis B, Faulds D. Inhaled fluticasone propionate: a review of its therapeutic efficacy at dosages <500µg/day in adults and adolescents with mild to moderate asthma. Drugs 1999 May; 57: 769–803
Weiss KB, Sullivan SD, Lyttle MS. Trends in the cost of illness for asthma in the United States, 1985–1994. J Allergy Clin Immunol 2000; 106: 493–9
Weiss KB, Gergen PJ, Hodgson TA. An economic evaluation of asthma in the United States. N Engl JMed 1992 Mar 26; 326: 862–6
Barnes PJ, Jonsson B, Klim JB. The costs of asthma. Eur Respir J 1996 Apr; 9: 636–42
Johnson KA, Ernst RL, Ogostalick AE. Analysis of direct, indirect, and total cost of asthma from patient survey data [abstract]. Value Health 1999 May–Jun; 2: 142
Serra-Batlles J, Plaza V, Morejon E, et al. Costs of asthma according to the degree of severity. Eur Respir J 1998 Dec; 12: 1322–6
Smith DH, Malone DC, Lawson KA, et al. A national estimate of the economic costs of asthma. Am J Respir Crit Care Med 1997 Sep; 156: 787–93
Sullivan SD. Economics of asthma and asthma treatments. Eur Resp Rev 1998 Sep; 8: 351–5
Bousquet J. Quality-of-life in allergic diseases. Rev Fr Allergol Immunol Clin 1998; 38 Suppl. 7S: S202–5
Osman LM, Calder C, Robertson R, et al. Symptoms, quality of life, and health service contact among young adults with mild asthma. Am J Respir Crit Care Med 2000; 161: 498–503
Okamoto LJ, Noonan M, DeBoisblanc BP, et al. Fluticasone propionate improves quality of life in patients with asthma requiring oral corticosteroids. Ann Allergy Asthma Immunol 1996 May; 76: 455–61
van der Molen T, Postma DS, Schreurs AJM, et al. Discriminative aspects of two generic and two asthma-specific instruments: relation with symptoms, bronchodilator use and lung function in patients with mild asthma. Qual Life Res 1997; 6: 353–61
Juniper EF, Guyatt GH, Epstein RS, et al. Evaluation of impairment of health related quality of life in asthma: development of a questionnaire for use in clinical trials. Thorax 1992 Feb; 47: 76–83
Ware Jr JE, Kemp JP, Buchner DA, et al. The responsiveness of disease-specific and generic health measures to changes in the severity of asthma among adults. Qual Life Res 1998; 7: 235–44
Dahl R. Salmeterol and fluticasone propionate in the treatment of asthma symptoms. Eur Resp Rev 1997 Aug; 7: 338–43
Jack D. The use of inhaled ß2-adrenergic bronchodilators and anti-inflammatory steroids in asthma. J Pharm Med 1996; 6 (1–2): 5–16
Chung KF. The complementary role of glucocorticosteroids and long-acting ß-adrenergic agonists. Allergy 1998; 53 Suppl. 42: 7–13
Eickelberg O, Roth M, Lorx R, et al. Ligand-independent activation of the glucocorticoid receptor by β2-adrenergic receptor agonists in primary human lung fibroblasts and vascular smooth muscle cells. J Biol Chem1999 Jan 8; 274 (2): 1005–10
Chapman KR, Walker L, Cluley S, et al. Improving patient compliance with asthma therapy. Respir Med 2000; 94: 2–9
Cochrane GM. Compliance in asthma. Eur Resp Rev 1998; 8 (56): 239–42
Cochrane GM, Horne R, Chanez P. Compliance in asthma. Respir Med 1999; 93: 763–9
Clark N, Jones P, Keller S, et al. Patient factors and compliance with asthma therapy. Respir Med 1999; 93: 856–62
Chapman KR. Effect of the inhaled route of administration on compliance in asthma. Eur Resp Rev 1998; 8 (56): 275–9
Markham A, Jarvis B. Inhaled salmeterol/fluticasone propionate combination: a review of its use in persistent asthma. Drugs 2000 Nov; 60 (5): 1207–33
Aubier M, Pieters WR, Schlosser NJJ, et al. Salmeterol/fluticasone propionate (50/500 µg) in combination in a Diskus inhaler (Seretide) is effective and safe in the treatment of steroid-dependent asthma. Respir Med 1999 Dec; 93: 876–84
Shapiro G, Lumry W, Wolfe J, et al. Combined salmeterol 50 µg and fluticasone propionate 250 µg in the Diskus device for the treatment of asthma. Am J Respir Crit Care Med 2000 Feb; 161: 527–34
Kavuru M, Melamed J, Gross G, et al. Salmeterol and fluticasone propionate combined in a new powder inhalation device for the treatment of asthma: a randomized, double-blind, placebo- controlled trial. J Allergy Clin Immunol 2000 Jun; 105 (Pt 1): 1108–16
Jenkins C, Woolcock AJ, Saarelainen P, et al. Salmeterol/fluticasone propionate combination therapy 50/250 µg twice daily is more effective than budesonide 800 µg twice daily in treating moderate to severe asthma. Respir Med 2000 Jul; 94: 715–23
Bateman ED, Britton M, Carrillo J, et al. Salmeterol/fluticasone combination inhaler: a new, effective and well tolerated treatment for asthma. Clin Drug Invest 1998 Sep; 16: 193–201
Chapman KR, Ringdal N, Backer V, et al. Salmeterol and fluticasone propionate (50/250 µg) administered via combination Diskus inhaler: as effective as when given via separate Diskus inhalers. Can Respir J 1999; 6 (1): 45–51
Nathan R, LaForce C, Mitchell D, et al. The salmeterol/fluticasone propionate combination (50/100mcg) via Diskus has a rapid onset of effect in asthma patients on salmeterol or inhaled corticosteroids [abstract]. Am J Respir Crit Care Med 1999 Mar; 159 (3 Pt 2) Suppl.: A637
Lumry W, Windom H, Mendelson L, et al. The salmeterol/fluticasone propionate (50/250mcg) dry powder combination Diskus has a faster onset of effect compared with salmeterol or fluticasone propionate in patients with asthma [abstract]. J Allergy Clin Immunol 1999; 103 (Pt 2): S132
Johansson G, McIvor RA, Purello D’Ambrosio F, et al. Seretide (salmeterol 50mcg/fluticasone propionate 100mcg bid) compared with budesonide (400mcgbid) in mild to moderate asthma [abstract]. Am J Respir Crit Care Med 1999 Mar; 159 (3 Pt 2) Suppl.: A637
Ringdal N, Chuchalin AG, Chovan L, et al. A comparison of Advair/Seretide (salmeterol 50 µg/fluticasone propionate 250 µg bid) with formoterol 12 µg + budesonide 800 µg bid in moderate-severe asthma [abstract]. Am J Respir Crit Care Med 2000 Mar; 161 (3 Pt 2) Suppl.: A196
Ringdal N, Chuchalin AG, Chovan L, et al. A comparison of Advair/Seretide (salmeterol 50 µg/fluticasone propionate 250 µg bid) with formoterol 12 µg + budesonide 800 µg bid in moderate-severe asthma [poster]. Presented at the International Conference of the American Thoracic Society; 2000May 5–10; Toronto
Lundback B, Jenkins C, Price MJ, et al. Cost-effectiveness of salmeterol/fluticasone propionate combination product 50/250 µg twice daily and budesonide 800 µg twice daily in the treatment of adults and adolescents with asthma. RespirMed 2000 Jul; 94: 724–32
Becker I, Kielborn A, Price MJ, et al. Cost-effectiveness of salmeterol/fluticasone combination product and budesonide in asthma patients in Germany [abstract no. P854]. 1999-ERS 1999 Oct 9: (abstracts on disk)
Sullivan S, Elixhauser A, Buist AS, et al. National Asthma Education and Prevention Program working group report on the cost effectiveness of asthma care. Am J Respir Crit Care Med 1996; 154: S84–95
Johansson G, Price MJ, Sondhi S. Cost-effectiveness analysis of salmeterol/fluticasone propionate 50/100µg vs fluticasone propionate 100µg in adults and adolescents with asthma. III: results. Pharmacoeconomics 1999; 16 Suppl. 2: 15–21
Palmqvist M, Price MJ, Sondhi S. Cost-effectiveness analysis of salmeterol/fluticasone propionate 50/250 µg vs fluticasone propionate 250 µg in adults and adolescents with asthma. IV: results. Pharmacoeconomics 1999; 16 Suppl. 2: 23–8
Pieters WR, Lundback B, Sondhi S, et al. Cost-effectiveness analysis of salmeterol/fluticasone propionate 50/500 µg vs fluticasone propionate 500 µg in patients with corticosteroiddependent asthma. V: results. Pharmacoeconomics 1999; 16 Suppl. 2: 29–34
Trubitt MJ. United HealthCare of Illinois: working to improve asthma care. Chest 1999 Oct; 116 (4 Suppl.): 208S-9S
Lloyd A, Browning D, Shrewsbury S. Cost-effectiveness of salmeterol/ fluticasone combination product and budesonide bd in the United Kingdom (asthma) [abstract]. Am J Respir Crit Care Med 2000 Mar; 161 (3 Pt 2) Suppl.: A196
Price MJ, Karia KP, Whitehead P. Comparison of asthma treatment costs of salmeterol/fluticasone combination product 50/ 250mcg bid with budesonide 800mcg bid plus formoterol 12mcg bid [abstract no. P2458]. Eur Respir J 2000; 16 Suppl. 31: 353s
Juniper EF, Guyatt GH, Ferrie PJ, et al. Measuring quality of life in asthma. Am Rev Respir Dis 1993; 147: 832–8
Juniper EF, Guyatt GH, Willan A, et al. Determining a minimal important change in a disease-specific quality of life questionnaire. J Clin Epidemiol 1994; 47: 81–7
Reese PR, Mahajan P, Woodring A. Salmeterol/fluticasone propionate combination product improves quality of life in asthma patients [abstract no. P0325]. Eur Respir J 1998 Sep; 12 Suppl. 28: 35s
Reese PR, Mather DB, Mahajan P, et al. Combination of salmeterol/fluticasone propionate via Diskus improves quality of life in asthma patients. J Allergy Clin Immunol 1999 Jan; 103 (Pt 2): S69
Juniper EF, Jenkins C, Price MJ, et al. Quality of life of asthma patients treated with salmeterol/fluticasone propionate combination product and budesonide. 1999-ERS 1999 Oct 9: (Abstr. on disk): Abstract no. P2460
National Institutes of Health. Highlights of the Expert Panel Report 2: guidelines for the diagnosis and management of asthma. Bethesda (MD): National Institutes of Health (National Heart, Lung, and Blood Institute), 1997 May. Publications No. 97–4051A. 1–50
British Asthma Guidelines Coordinating Committee. The British Guidelines on Asthma Management: 1995 review and position statement. Thorax 1997 Feb; 52 Suppl. 1: S1–21
National Asthma Education and Prevention Program. Expert Panel report 2: guidelines for the diagnosis and management of asthma. Bethesda (MD): National Heart, Lung, and Blood Institute Information Center, 1997 Jul. NIH Publication No. 97–4051
Adkins JC, McTavish D. Salmeterol: a review of its pharmacological properties and clinical efficacy in the management of children with asthma. Drugs 1997 Aug; 54: 331–54
Brogden RN, Faulds D. Salmeterol xinafoate: a review of its pharmacological properties and therapeutic potential in reversible obstructive airways disease. Drugs 1991; 42: 895–912
Holliday SM, Faulds D, Sorkin EM. Inhaled fluticasone propionate: a review of its pharmacodynamic and pharmacokinetic properties, and therapeutic use in asthma. Drugs 1994 Feb; 47: 318–31
Rutten-van Mölken MPMH, Van Doorslaer EKA, Jansen MCC, et al. Costs and effects of inhaled corticosteroids and bronchodilators in asthma and chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1995; 151: 975–82
Author information
Authors and Affiliations
Corresponding author
Additional information
Various sections of the manuscript reviewed by: P.J. Barnes, Department of Thoracic Medicine, National Heart & Lung Institute, Imperial College, London, England; D.W. Boulton, Medical University of South Carolina, Charleston, South Carolina, USA; K. Nishimura, Department of Respiratory Medicine, Graduate School of Medicine, Kyoto University, Kyoto, Japan; J.M. Negro, Allergology Section, HU Virgen de la Arrixaca, Murcia, Spain; M.P.M.H. Rutten-van Mölken, Erasmus University Rotterdam, Rotterdam, The Netherlands; R.E. Vestal, Clinical Pharmacology Consulting, Boise, Idaho, USA.
Data Selection
Sources: Medical literature published in any language since 1966 on salmeterol/fluticasone-propionate, identified using Medline supplemented by AdisBase (a proprietary database of Adis International, Auckland, New Zealand). Additional references were identified from the reference lists of published articles.Bibliographical information, including contributory unpublished data,was also requested from thecompany developing the drug.
Search strategy: AdisBase search terms were ‘salmeterol/fluticasone-propionate’ or ‘asthma’ and (‘health-economics’ or ‘pharmacoepidemiology’ or ‘prescribing’ or ‘hospitalisation’ or ‘formularies’ or ‘drug-utilisation’ or ‘meta-analysis’ or ‘therapeutic-substitution’ or ‘epidemiology’), or ‘salmeterol/fluticasone-propionate’ and ‘asthma’. Medline search terms were ‘salmeterol/fluticasone-propionate’ or ‘asthma’ and (‘economics’ or ‘health-policy’ or ‘quality-of-life’ or ‘models-statistical’ or ‘health-planning’ or ‘epidemiology’ or ‘guideline in pt’ or ‘practiceguidelines in pt’. Searches were last updated 20 November 2000.
Selection: Economic analyses in patients with asthma who received salmeterol/fluticasone-propionate in a single inhalation device. Inclusion of studies was based mainly on the methods section of the trials. Relevant background data on epidemiology and cost of illness are also included.
Index terms: Salmeterol, fluticasone propionate, asthma, pharmacoeconomics, cost effectiveness, therapeutic use.
Rights and permissions
About this article
Cite this article
Markham, A., Adkins, J.C. & Jarvis, B. Inhaled Salmeterol/Fluticasone Propionate Combination. Pharmacoeconomics 18, 591–608 (2000). https://doi.org/10.2165/00019053-200018060-00006
Published:
Issue Date:
DOI: https://doi.org/10.2165/00019053-200018060-00006